Isolation Policy - Portsmouth Hospitals Trust
advertisement
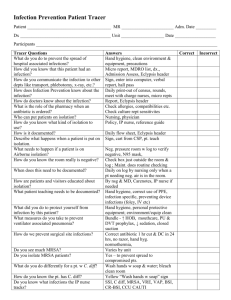
Isolation Policy Version 5 Name of responsible (ratifying) committee Infection Prevention Management Committee Date ratified 14 May 2015 Document Manager (job title) Dr Caroline Mitchell (Head of Infection Prevention) Date issued 17 July 2015 Review date 16 July 2017 Electronic location Infection Prevention and Control Policies Related Procedural Documents Key Words (to aid with searching) Hand Hygiene policy MRSA/MSSA policy Standard Infection Control Precautions policy Clostridium difficile infection (CDI) management policy Management of Outbreaks of Viral Diarrhoea & Vomiting policy Decontamination policy Viral Haemorrhagic Fever Policy Isolation, transmission precautions, source isolation, protective isolation Version Tracking Version Date Ratified 5 14/05/15 Brief Summary of Changes Author Update of Notification of Infectious Diseases, contact details for PHE Wessex Centre, addition of quick reference guide Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Caroline Mitchell Page 1 of 14 CONTENTS QUICK REFERENCE GUIDE ............................................................................................................. 3 1. INTRODUCTION.......................................................................................................................... 4 2. PURPOSE ................................................................................................................................... 4 3. SCOPE ........................................................................................................................................ 4 4. DEFINITIONS .............................................................................................................................. 4 5. DUTIES AND RESPONSIBILITIES .............................................................................................. 4 6. PROCESS ................................................................................................................................... 5 7. TRAINING REQUIREMENTS .................................................................................................... 10 8. REFERENCES AND ASSOCIATED DOCUMENTATION .......................................................... 10 9. EQUALITY IMPACT STATEMENT ............................................................................................ 10 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS ........................................ 12 APPENDIX 1: Standard Isolation Signage (available from Infection Prevention Team) ..................... 13 Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 2 of 14 QUICK REFERENCE GUIDE For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. Confirmed or suspected Infectious Disease (see 6.14 Alert Organisms) NO No further action required YES Refer to Infection Prevention or Medical Microbiology immediately YES Isolate and start transmission precautions (review need for isolation daily) YES Transfer patient into isolation and start transmission precautions (review need for isolation daily) YES Transfer patient into isolation and start transmission precautions. Inform medical team of transfer (review need for isolation daily) YES Suspected or confirmed MDR Tuberculosis or Viral Haemorrhagic Fever? NO Single room available within clinical area/ward? NO Escalate to Specialty Flow Coordinator Single room available within specialty footprint/CSC? NO Escalate to Bed Meeting / Duty Hospital Manager Single room available within hospital? NO Escalate to Infection Prevention Team (24 hours per day) for risk assessment Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Always explain the needs for isolation (including risks and benefits) to the patient Page 3 of 14 1. INTRODUCTION Isolation refers to the use of a single room as a physical barrier to help prevent the transmission of potentially infectious organisms. Isolation has been shown to be effective in reducing onwards spread of infection but is only one element of a successful infection prevention strategy. Other measures, such as environmental and equipment cleaning, the correct use of personal protective equipment (PPE) and above all hand hygiene are equally or more important. 2. PURPOSE The aim of this policy is to ensure appropriate use of isolation facilities based on local risk assessment in accordance with the Health & Social Care Act (DH 2010). This policy should be used with reference to the: Hand Hygiene policy MRSA/MSSA policy Standard Infection Control Precautions policy Clostridium difficile infection (CDI) management policy Management of Outbreaks of Viral Diarrhoea & Vomiting policy Decontamination policy 3. SCOPE This policy applies to all PHT Healthcare workers (HCW), including agency, bank and locum staff, Carillion staff including porters and house keepers and visiting HCW’s from other organisations. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ 4. DEFINITIONS Nil 5. DUTIES AND RESPONSIBILITIES Infection Prevention Team: Review and update Isolation policy Give additional advice regarding the management of patients requiring isolation where required Include isolation precautions in all induction and update training for clinical staff Promote good practice and challenge poor practice Conduct audit and inspection of isolation practice with feedback to clinical staff Microbiologists: Alert Infection Prevention Team and clinical teams of patients requiring isolation following confirmation of certain infections Advise clinical staff of the need for isolation at the time of notification of an infectious (or potentially infectious) disease Patient Flow / Duty Hospital Managers: Facilitate placement of patients with potential or known infections into appropriate isolation rooms as soon as possible Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 4 of 14 Monitor the appropriate usage of isolation rooms Escalate difficulties in isolation to the Infection Prevention Team Report breaches of isolation to Infection Prevention Team and by incident reporting Matrons / Senior and Ward Sisters: Must establish a cleanliness culture across their units and promote compliance with infection prevention guidelines Promote good practice and challenge poor practice Medical Staff: Ensure compliance with infection prevention policies Follow advice from the Infection Prevention Team relating to isolation of patients Review the need for isolation on a daily basis All Healthcare Staff: Must be familiar with and adhere to the relevant infection prevention policies to reduce the risk of cross infection of patients Must adhere to the full terms and conditions of isolation documented in this policy Must use the risk assessment process to identify the isolation priorities of individual patients Promote good practice and challenge poor practice Refer to the infection prevention team if unable to follow the policy guidelines Keep their patient informed of their infection status and provide information as necessary Must ensure that patients who are isolated have access to investigations and rehabilitation 6. PROCESS 6.1 Principles of Isolation: Isolation is one aspect of effective infection prevention policy and standard infection control precautions should be applied to all patients without exception Isolation must never compromise the safety or clinical care of a patient The benefits of isolation should be weighed against the potential risks to the patient (patient’s mental state, severity of illness etc) and to other (public health risk) and patients should receive preparatory and ongoing information relating to their condition, treatment and rationale behind isolation Infection risk should be constantly assessed as part of the ongoing clinical patient assessment and managed accordingly. Isolation must be discontinued as soon as the risk of onwards transmission of infection has diminished or resolved 6.2 Source Isolation: Refers to the physical isolation of a patient with suspected or confirmed transmissible infection in a single room in order to prevent or reduce the risk of onwards transmission by blocking the route of spread. Source isolation of infectious patients should occur in: A neutral pressure single room with ante room OR A negative pressure single room with ante room OR A standard single room The room should be cleaned after all other ward cleaning has been carried out 6.3 Protective Isolation: Refers to the physical isolation of a susceptible patient in a single room in order to reduce the risk of exposure to potentially harmful micro-organisms. Protective isolation of immunocompromised/susceptible patients should occur in: A positive pressure single room with ante room OR A neutral pressure single room Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 5 of 14 The room should be cleaned before any ward cleaning is carried out 6.4 Cohorting: An alternative of last resort to single room isolation is the cohorting of patients together with the same condition. However, not all patients with similar symptoms e.g. diarrhoea, have the same aetiology and many patients with the same organism e.g. C.difficile will have different strains. Cohorting should only be undertaken following discussion with and approval by the infection prevention team. 6.5 Escalation Strategy: Potentially infectious patients should be isolated within 2 hours of first suspicion Where no suitable single room is available in the immediate clinical area, staff should escalate to: i. Specialty flow coordinator and if no flow coordinator to Matron (then) ii. Duty hospital manager (then) iii. (On-call) Infection Prevention Team 6.6 Isolation Preference: i. Isolation room in the immediate clinical area/ward ii. Isolation room within the same Clinical Service Centre iii. Isolation room outside the Clinical Service Centre It is appropriate in most circumstances to transfer the patient outside the specialty of Clinical Service Centre to achieve isolation, provided the responsible medical team is aware. 6.7 Asset List: The Trust currently has: 10 positive pressure single rooms with ante room (protective isolation) F6 ward 6 neutral pressure single rooms with ante room (source or protective) E5 ICU 12 neutral pressure single rooms with ante room (source or protective) G5 ward (emergency use only) 2 adjustable positive/neutral pressure single rooms with ante room F5 ward >220 standard single rooms across all wards 6.7 Common Principles of Isolation: The need for isolation should be clearly communicated to the patient, family members (if appropriate) and clinical staff The need for isolation should be reviewed on a daily basis. Discuss specific cases with the Infection Prevention Team A generic isolation sign should be prominently displayed on the room door to alert people to potential risk without compromising confidentiality (appendix 1 & 2) Ensure that the door remains closed, especially when airborne infections are suspected/confirmed e.g. pulmonary TB, influenza 6.8 Hand Hygiene & PPE: (see hand hygiene and Standard Infection Control Precautions Policies) Hand hygiene facilities should be easily accessible inside and outside of the single room Clinical staff and visitors must decontaminate hands on entry and exit of the room Patients should be strongly encouraged to clean hands regularly, either with soap and water, or cleansing wipes, particularly after using the toilet and before eating PPE (gloves, aprons/gowns, face masks/visors (where appropriate)) should be prominently available outside the room entrance Protective equipment should only be worn by relatives carrying out direct ‘hands on care’ and not for routine social visiting Limit and restrict the number of staff and visitors who come into contact with the patient to reduce the potential to spread or introduce infection. Where immunity to a condition occurs e.g. Chicken Pox, staff and visitors should be restricted to those who are non-susceptible Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 6 of 14 6.9 Cleaning, Linen & Waste: The room must be cleaned at least once daily with dedicated cleaning equipment using a suitable agent (hypochlorite e.g. Actichlor plus or chlorine dioxide e.g. Difficil-S) focusing on common touch points (door handles, bed rails, tables, chair arms, taps etc) Carillion are responsible for cleaning the clinical environment, clinical staff are responsible for cleaning clinical equipment Ensure that the room is kept clean and uncluttered, with flat surfaces clear of unnecessary items Only stock that is required should be taken into the room Clinical equipment inside the room must be dedicated to the patients until the patient is discharged or no longer deemed to be infectious. The equipment must then be appropriately decontaminated before being used on other patients. If equipment cannot be restricted to a single patient then equipment must receive a thorough clean with a chlorine agent before leaving the room Charts and notes should be kept outside the room to reduce the risk of contamination Clinical waste bin with either a yellow/black ‘tigerstripe’ bag (non-infectious offensive waste for protective isolation) or orange (infectious offensive waste for source isolation) should be kept in the room as appropriate All linen should be bagged at the bedside as infectious linen in appropriate coloured bags 6.10 Transport of Infectious Patients: Movement of infectious or potentially infectious patients should be kept to a minimum. When it is necessary to transfer patients to other wards or departments, precautions to minimise the risk of transmission, based on the route of spread, must continue If it is possible to delay an investigation without adversely affecting the patients management this should be considered. However, infectious disease should not compromise urgent clinical investigations The receiving area must be informed prior to transfer to ensure appropriate precautions are in place and that suitable segregation facilities are available Patients with known or suspected infections should not be placed in waiting areas and adequate time for post procedure cleaning should be built into clinic/theatre schedules 6.11 Terminal Room Cleaning: All rooms must be thoroughly cleaned with hypochlorite e.g. Actichlor plus or chlorine dioxide e.g. Difficil-S when vacated. This includes between patients with the same organism. Curtains must be removed and sent to the laundry as infected linen All disposable equipment should be discarded into orange clinical waste bags All clinical equipment, including bed frames should be thoroughly cleaned by clinical staff All areas of the room should be cleaned using dispoable clothes with particular attention paid to touch points and horizontal surfaces e.g. door handles, taps, dispensers, nurse call system, toilet areas, bed frame, tables, lockers, chairs For certain infections (e.g. C.difficile, Carbapenem resistant Organisms, Gylcopeptide resistant Enterococi, Acinetobacter, other multi-drug resistant organisms), decontamination with Hydrogen Peroxide Vapour may be required – contact the Infection prevention Team to arrange. 6.12 Very High Risk Patients: Adults and children with suspected or known infectious Multi Drug Resistant (MDR TB) and Extensively Drug Resistant TB (XDR-TB) must be admitted to a negative pressure room. These patients should be referred to University Hospital Southampton Isolation Unit via Medical Microbiology. Clinicians caring for a patient with recent foreign travel with suspected Viral Haemorrhagic Fevers (VHF) must immediately contact the Microbiologist on call for advice on where to refer the patient. The patient must be isolated (preferably in a negative pressure single room – currently designated Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 7 of 14 G5 ward) as soon as possible. For confirmed VHF, the patient should be transferred to the Royal Free Hospital London which has appropriate facilities for the management of these patients. Arrangements should be made in conjunction with the Public Health England (Wessex Centre). Public Health England (Wessex Centre) Unit 8, Fulcrum 2, Solent Way, Whiteley Fareham, Hampshire PO15 7FN Tel: 0345 055 2022 6.13 Notification of Infectious Diseases: It is the responsibility of the attending registered medical practitioner to notify infectious diseases. Notification forms can be obtained via the GOV.UK website at https://www.gov.uk/government/collections/notifications-of-infectious-diseases-noids Diseases notifiable (to Local Authority Proper Officers) under the Health Protection (Notification) Regulations 2010: Acute encephalitis Acute infectious hepatitis Acute meningitis Acute poliomyelitis Anthrax Botulism Brucellosis Cholera Diphtheria Enteric fever (typhoid or paratyphoid fever) Food poisoning Haemolytic uraemic syndrome (HUS) Infectious bloody diarrhoea Invasive group A streptococcal disease Legionnaires’ Disease Leprosy Malaria Measles Meningococcal septicaemia Mumps Plague Rabies Rubella SARS Scarlet fever Smallpox Tetanus Tuberculosis Typhus Viral haemorrhagic fever (VHF) Whooping cough Yellow fever Other diseases that may present significant risk to human health should be reported under the category ‘other significant disease’. As of April 2010, it is no longer a requirement to notify the following diseases: Dysentery, Leptospirosis, Ophthalmia neonatorum, Relapsing fever and Viral hepatitis. 6.14 Alert Organisms: The following list is provided as guidance and is not exhaustive. For complicated presentations, please contact the Infection Prevention Team. Alert Organism Abscesses e.g. quinsy Blood borne virus e.g. HIV, Hepatitis B,C Risk Factors Assess the patient Campylobacter Immunocompromise Carbapenem Resistant Organisms Chicken Pox Hospital (particularly ICU) admission in at risk areas Rash developed within Assess the patient Isolation Requirement Isolate until 24-48 hours of appropriate antibiotics. Discuss with the Infection Prevention Team Isolation not required unless there is a high risk of blood or blood stained body fluid splash. Additional precautions may be required within the renal dialysis unit Isolate whilst acutely symptomatic (80-90% of cases resolve by day 7) but excretion in stools may continue for 2-7 weeks Isolate and full precautions for the duration of hospital admission (and any readmission) Immediate isolation required. Only staff with a history of Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 8 of 14 the previous 10 days or vesicles not crusted over Clostridium difficile Toxin positive Carriage (GDH or PCR positive, Toxin negative) CJD Cryptosporidium immunocompromise Diarrhoea (infectious) Exclude overflow, laxatives, ng feeds, crohns/colitis etc Extended Spectrum Beta-Lactamase (ESBL) producing organisms in urine Incontinent patient Catheterised or fully continent patient ESBL producing organisms in other sites GRE Glycopeptide resistant enterococci (including VRE) Assess individual risks e.g. weeping wounds etc. Influenza (including Avian flu and H1N1) Legionella (legionnaires disease) Malaria Confirmed Suspected Measles Suspected meningitismeningococcal Meticilin Resistant Staphylococcus aureus (MRSA) Mumps Norovirus Salmonella (inc. typhi (typhoid fever)) Sputum Positive with productive cough, flaking skin condition, wet wounds with break through Skin colonisation only Chicken pox (or serologically confirmed immunity) should have contact with this patient. Patient can be removed from isolation once vesicles fully crusted Isolate for duration of hospital admission, regardless of symptoms. Isolate if readmitted within 6 months of original diagnosis Isolate for duration of hospital admission, regardless of symptoms. Isolate if readmitted within 6 months of original diagnosis Isolation not required. See CJD policy for advice re surgical procedures. Inform microbiologist on call immediately if diagnosis is suspected to ensure safe handling of specimens Isolate whilst symptomatic (2 days to 4 weeks), immunocompromised patients will take longer to clear infection Immediate isolation, preferably within 2 hours of onset of symptoms until full resolution of diarrhoea and formed stool (with the exception of C.difficile patients who remain isolation for the duration of admission) Isolation required. Encourage good hand and personal hygiene. Dedicated commode (or lavatory) cleaned between each use Isolation preferable. Encourage good hand and personal hygiene. Dedicated commode (or lavatory) cleaned between each use Isolation required. Encourage good hand hygiene and personal hygiene. If possible use a dedicated toilet. Discuss with Infection Prevention Team if required Isolate for duration of hospital admission, regardless of symptoms. Isolate if readmitted. Patient will have longterm skin and intestinal carriage. Dedicated bathroom facilities. Encourage good hand hygiene and personal hygiene Isolate until patient has completed course of antivirals and is symptom free. FFP3 face masks to be worn for aerosol generating procedures. FFP1 face masks to be worn during non aerosol generating close contact. For avian influenza inform microbiologist on call immediately if diagnosis is suspected Not transmitted between individuals, no isolation required Not transmitted between individuals, no isolation required Febrile illness with a history of travel to tropical/subtropical area should be managed as high risk until malaria diagnosis confirmed Isolate until 5 days after onset of rash Isolate until 24 hours of antibiotics. FFP1 face mask to be worn during any procedure likely to generate respiratory droplets. Inform occupational health if in direct contact with respiratory secretions e.g. during resuscitation Immediate isolation required. Discuss with the Infection Prevention Team If no single room available, may be treated in a main bay if located next to a hand washing sink with full transmission precautions Isolate until 9 days after onset of rash Isolate immediately on first episode of projectile vomiting or diarrhoea, until 48 hours after complete cessation of symptoms Isolate infants until clinical recovery occurs. Cohort nursing may be considered in certain circumstances if all patients RSV status known Isolate immediately (excretion may continue for 2 days to 2 months, median 5 days) Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 9 of 14 Shigella Shingles Tuberculosis Rash in an exposed area with wet lesions Rash in a covered area with wet/drying lesions Confirmed pulmonary TB with a productive cough Suspected pulmonary TB AFB negative pulmonary TB/ TB closed site Suspected/ Confirmed drug resistant TB Norwegian Scabies Often affects immunocompromised patients Classical scabies Group A Streptococcus SARS Awaiting diagnosis Vancomycin resistant enterococci (VRE) Viral Hemorrhagic Fever See GRE Isolate whilst acutely symptomatic (excretion may continue for 2-4 weeks post acute illness) Isolate until lesions are fully dried. Only staff with a history of Chicken pox (or serologically confirmed immunity) should have contact with this patient May be treated in a main bay provided no immunocompromised patients are in the room Isolate until 14 days continuous, compliant treatment. Use FFP 2 or 3 facemask for contact Isolate until 3 negative sputum specimens on microscopy No requirement to isolate Discuss with TB nurse specialist and Infection Prevention Team. Will require isolation in a negative pressure side room and transfer to alternative site Highly transmissible, isolate until full course of treatment has been completed (minimum 2 treatments) Discuss with Infection Prevention Team Isolate until 48 hours of appropriate antibiotics Immediate isolation required. Inform Infection Prevention or Microbiologist on call immediately if diagnosis is suspected Discuss with Infection Prevention Team or Microbiologist on call immediately if diagnosis is suspected. Will require isolation in a negative pressure side room and transfer to alternative site 7. TRAINING REQUIREMENTS Clinical and non-clinical staff to receive practical hand hygiene training on induction and every 2 years thereafter (Infection Prevention Team) Clinical and non-clinical staff to receive face-to-face induction training on aspects of infection prevention & isolation (Infection Prevention Team) Update training to be delivered as part of Patient Safety & Quality Days, departmental and drop in days, Link Advisor days and Senior Doctors Training (Infection Prevention Team) 8. REFERENCES AND ASSOCIATED DOCUMENTATION Ayliffe, G.A.J, Babb, J.R, Taylor, L.Z (2001) Hospital Acquired Infection, Principles and Prevention. Third Edition, Arnold Page Department of Health (2010) The Health Act 2008 Code of Practice for the Prevention and Control of Health Care Associated Infections London DH, 2010 Kundrapu S, Sunkesula V, Jury LA, Sitzlar BM, Donskey CJ. Daily disinfection of high-touch surfaces in isolation rooms to reduce contamination of healthcare workers’ hands. Infect Control Hosp Epidemiol 2012;33:1039–1042. 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 10 of 14 Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviours our employees display in the workplace. Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do. We are committed to promoting a culture founded on these values which form the ‘heart’ of our Trust: Respect and dignity Quality of care Working together No waste This policy should be read and implemented with the Trust Values in mind at all times. Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 11 of 14 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS This document will be monitored to ensure it is effective and to assurance compliance. Minimum requirement to be monitored Lead Tool Frequency of Report of Compliance Time to isolation for patients with suspected infectious diarrhoea IPCT Infection Prevention Dashboard Weekly for all areas Policy audit report to: Quality of Isolation (PPE, Clutter, Signage, Chlorine Cleaning) IPCT Infection Prevention Dashboard Weekly for all areas Policy audit report to: Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Reporting arrangements Lead(s) for acting on Recommendations HoN HoN, MM, Consultants, Ward Managers, IPMC HoN, MM, Consultants, Ward Managers, IPCM Page 12 of 14 HoN APPENDIX 1: Standard Isolation Signage (available from Infection Prevention Team) Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 13 of 14 APPENDIX 2: Standard Isolation Signage (available from Infection Prevention Team) Isolation Policy Issue Number: 5 Issue Date: 17 July 2015 Review date: 16 July 2017 (unless requirements change) Page 14 of 14