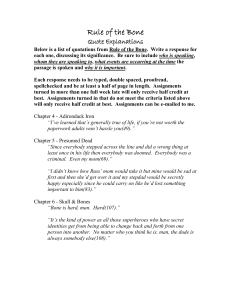
Bone grafting techniques
advertisement

Bone Grafting Bone grafting and augmentation is a surgical procedure that replaces missing bone by various materials and methods. Implants are placed in an area which is missing a tooth or in an area where the tooth will be soon extracted. Dental implants generally need some type of bone augmentation or grafting in a large number of cases as there will generally be loss of alveolar bone in this area. If there is insufficient bone a dental implant cannot be placed predictably and placement can be compromised. Bone grafts or materials attempt to increase bone by 3 ways; osteogenesis, osteoconduction and osteoinduction. Osteogenic cells in grafts promote cells to differentiate and change into bone, (living bone cells in the graft material contribute to bone remodelling). Osteogenesis only occurs with autogenous/autografts. Osteoconduction promotes bone apposition onto its surface, working as a scaffold for new bone and guiding the reparative growth of the natural bone. Osteoinduction provides a stimulus to induce bone into the area. It encourages undifferentiated cells to become active osteoblasts and new bone is laid down. There are 4 main subgroups to the various materials that can be used to regenerate bone through bone grafting techniques in an area deficient. Autogenous (meaning self generated or produced) Autogenous bone is bone extracted from a site surplus of bone and grafted to the deficient bony area in the same patient. The area where bone is harvested can be from extra oral or intra oral sources. Common areas to harvest bone extra orally include; the tibia, iliac crest, cranium, ribs and fibulas. Common intra oral areas to harvest bone include; the symphysis region, maxillary tuberosity, exostoses, debris from implant/oral surgery sites and the ramus/body of the mandible. A less common area used involves the coronoid process. Intra oral autogenous bone is considered the gold standard1,4. It can be harvested in block bone forms by cutting out section from the harvest site with saws, burs or trephines. The area is then chiselled and removed with greenstick fractures. It can also be harvested in particulate form by scraping the bone with various devices or instruments. The block graft may also be ground down by a bone grinder to produce a particulate form. Grafted bone can be cortical, trabecular or corticotrabecular. The trabecular bone contains osteogenic cells and survives best with a good blood supply and is placed closest to the host’s bone. This allows new blood vessels to enter the graft to revascularise it. The cortical plate supports the scaffold for the osteoconductive phase and provides bone morphogenic proteins for osteoinductive phase. Grafted autogenous bone heals in three phases. The first phase, the osteogenic cells that survive in the graft forms an osteoid by osteogenesis. This occurs within 4 weeks. Osteoinduction occurs between 2-6 weeks after grafting and up to 6months. New blood vessels and connective tissues are established from the host site. The graft is remodelled by resorption and new bone formation. Bone morphogenic proteins (BMP) are released and are resorbed by osteoclasts mainly from the cortical bone. In phase three the inorganic matrix acts as a scaffold for the osteoconductive part. The graft matrix is replaced by new bone2. Principles of Implant Dentistry Assignment 4 2 Year 2, March 2012 Student ID 1151830 The advantages to autogenous grafts are that they are osteoconductive, inductive and osteogenic and the only material to be so. There will unlikely be a rejection of the patients own tissue. However there are a number of disadvantages. The patient will undergo further surgery, morbidity and post operative pain. There is also a limited supply of graft from the patient’s own bone. Although autogenous is the best material for osteogenesis there are a number of substitutes/alternatives that can be employed. Allografts (meaning other generated or produced) Allograft bone is bone from within the same species. This normally means a bone graft from another person to the patient’s recipient site. The graft may come from living humans or cadavers. They are osteoconductive and osteoinductive but not osteogenic3,4 and therefore it takes longer to form new bone. However the advantages of allografts are that they are readily available and exclude the need for further surgery in the patient. The disadvantages are that allografts can also induce an immune response and the patient may reject the graft5,6. There is also a small risk of transmissible infectious diseases from the allograft7,8 with no reported cases of HIV since 1985. There are 4 commonly used types of allograft available. They are all different due to their preparations after being harvested. However they are all harvested from disease and infection free donor. Fresh Frozen9,10 allografts are removed and frozen. Proponents suggest that they have better biological and biomechanical properties as opposed to the other types. However they are more prone to transmitting infections. Principles of Implant Dentistry Assignment 4 3 Year 2, March 2012 Student ID 1151830 Freeze dried (lyophilized)11 allograft is freeze dried first and then the surrounding pressure is reduced sublimating the frozen water in the graft and dehydrating the allograft. Demineralised freeze dried12,13 allograft is similar to freeze dried but with the additional step of exposing the bone to hydrochloric or nitric acid for 6 to 16 hours. The BMP are not acid soluble but the calcium and phosphate ions are and removed. This then exposes the BMP. This then allows quicker osteoinduction as the BMP are more easily/readily available. Irradiated14,15 allografts. These bone grafts are harvested and exposed to varying levels of gamma radiation to remove any infectious pathogens to reduce the chances of transmissible diseases. It has been noted however that to remove the HIV virus 50kGy is needed but the upper limit in the USA is 25 kGy. A lot of allografts are a mixture of the above types. There are demineralised freeze dried irradiated allografts. Autogenous and allografts bone can be harvested as block pieces of bone or as particulate form. These block pieces can be placed over the host bone and fixed in place by screws. Xenografts (meaning guest/foreign material) The advantages to xenografts are that there is unlimited bank of bone graft available. There has been some protest to the killing of animals to harvest bone graft. There is also possibility of disease transmission from animal to human from xenografts. Principles of Implant Dentistry Assignment 4 4 Year 2, March 2012 Student ID 1151830 The donor graft material and the recipient patient are different species. A commonly used product in the UK is BioOss a bovine originated xenograft. But they can be from equine, ovine and porcine sources. Alloplast (meaning other structure/ particle/ granule) These are synthetically produced graft materials. They are classed due to their porosity (dense, macroporous, microporous) or if they are crystalline or amorphous and if they are granular or moulded. There are a large number of different products available, but they all generally consist of calcium/phosphate based materials. Most alloplasts are generally osteoconductive, acting as a scaffold for host bone to grow into the scaffold. It is beyond this assignment to go into detail the different types of alloplast available. The disadvantages of xenografts and alloplasts are that there is a possibility of rejection from a foreign based substance. Some patients may decline the use of xeno grafts due to religious beliefs (use of bovine substances for Hindus and porcine for Muslims). However the main advantage is that they come from an unlimited source. The alloplast/xenograft scaffold is resorbable or non resorbable. The resorbable type is replaced by new bone. As such alloplast/xenograft is generally osteoconductive. There is no scientific data to prove that allograft, alloplast or xenograft is better or more advantageous than the other. All four materials are used as inlay grafts, placed in defects with more than 2 walls. They are usually placed in defects like this in particulate/putty form. Collagen Membranes are used in guided bone regeneration during bone augmentation. Principles of Implant Dentistry Assignment 4 5 Year 2, March 2012 Student ID 1151830 These membranes are either resorbable or non resorbable. They also have chemotactic and haemostatic properties. It can bond and activate platelets to form a platelet plug and it accelerates healing. They prevent epithelial cells and soft tissue ingress in the grafted site during the healing process. They are normally placed over the graft area and under the patient’s own mucosa and soft tissue. The soft tissues are then sutured over the membrane. They resorption rates of collagen membranes can vary16.They allow and maintain space which creates the ideal environment for bone regeneration. Principles of Implant Dentistry Assignment 4 6 Year 2, March 2012 Student ID 1151830 Bone grafting techniques There are various techniques of bone grafting. These are performed and depend on the situation (walled defect), skill of the operator, the patient’s medical and financial situation. Tooth extraction and socket grafting A tooth which is to be replaced by an implant may be removed and an implant placed a number of weeks later after the alveolar bone has healed. However there is strong evidence to suggest that grating the socket may preserve bone width and certainly decrease the rate of resorption in bone height17,18,19,20,21. Without socket grafting there could be bone loss which can compromise ideal implant placement. The amount of bone loss according to studies ranges from 2.6mm -6.1mm loss of alveolar ridge width and 0.2mm – 1.5mm in height. Not only that but in aesthetic areas it maintains soft tissue in high smile lines, where loss of ridge height may compromise the end result. It can also prevent the need of sinus augmentation and avoid id nerve complications at a later date if the socket height and width is preserved. After a simple extraction maintaining 5 or 4 bony wall defect simple graft material may be placed in to the socket site. It has been suggested that after a tooth has been extracted as atraumatically as possible. Ideally this is done with periotomes or other tools that can maintain the socket walls. All fibrous tissue can be removed from the socket by excavation Principles of Implant Dentistry Assignment 4 7 Year 2, March 2012 Student ID 1151830 leaving a 5 walled defect. All infected soft tissue and other fragments should be removed. The 5 walls should be checked, especially the buccal wall, to ensure it is intact before placing graft material into the socket. The socket can be filled with particulate bone graft with a barrier membrane (BM) over the socket graft which is tucked in, under the attached mucosa but over the periosteum, completely covering the socket. The 5 walls maintain the space to allow new bone growth. However when it is a 2,3,or 4 wall defect space maintenance is lost, there is less vascularisation from surrounding bony walls and soft tissue ingress can occur. The socket cannot regenerate the lost bone if left untreated. There is bony healing by repair and not regeneration.22. It is even more important that socket grafting is considered if implant placement is to be considered. The facial/palatal wall mucosa may be reflected to visualise the defect(s) if needed and elevate the soft tissue tunnelling over the periosteum. This then allows the BM to be tucked in under the soft tissue over the bone defect(s) to the remaining lateral and adjacent walls. The bone graft is then placed into the socket. The BM is then tucked into the palatal tissues. Sutures are then placed to secure the graft and BM in place. It has been suggested that with 2,3 or 4 bony wall defects it is more important to place autogenous bone graft23. It has been researched through various studies that after an extraction an implant can be placed immediately, if primary stability can be gained, and ridge augmentation simultaneously at the same time. The results have shown that immediate placement after extraction with ridge augmentation to fill in the bony defect is predictable and successful23,24,25. However to gain height is very technique sensitive but achievable by an experienced operator44. Principles of Implant Dentistry Assignment 4 8 Year 2, March 2012 Student ID 1151830 The advantage to these particulate bone grafts are that they are easier to learn and perform, relatively small surgical site, post op pain is relatively low and the material is easy to adapt to the adjacent structures. Inlay bone particulate grafts are very predictable and stable26. However the larger the defect the less predictable the graft will be. Other disadvantages include poorer quality bone is produced, bone height and width are limited to 3-4mm , extended healing times are needed and unpredictable results with doing full mouth arches or 1-2 bony wall defects27,28. Onlay Grafting For 1 and 2 walled large defects an onlay bone graft is recommended and considered gold standard29,30,31,32,33. The bone, as previously mentioned, can be harvested intra or extraorally. The advantages to extraoral sites are that there is more abundant bone, which may be needed depending on the amount of reconstruction. The bone has been shown to be stabile and not to resorb after grafting34. It was first described by Branemark using the iliac crest35. However there are a number of disadvantages. General anaesthesia is needed, hospital stay is needed, higher costs and decreased movement/ambulation. Intraoral bone for grafting was originally used to correct cleft palates. Jensen in 1991 36 and Misch in 199237 has since utilised the technique for dental implants. The intraoral bone has a number of advantages over extraoral bone. It is an acceptable surgical procedure which can be performed by dental surgeons. Obviously there is little need for general anaesthesia, so less cost, morbidity overnight stays in the hospital is avoided. There is no visible extra oral scarring and less post op Principles of Implant Dentistry Assignment 4 9 Year 2, March 2012 Student ID 1151830 discomfort. Intraoral bone such as alveolar, maxillary and mandibular bone with exception to the condyles develop intramembranously. As the harvest bone is similar to the recipient bone there seems to be physiological benefits as opposed to the endochondral bone of extraoral sites. Intra oral bone show less resorption38 and revascularise quicker with more stable long term results39,40. The selection of symphysis or ramus for donor site depends on a number of factors. According to Misch22 if the width needed is 4mm or more then the symphysis is used. If less than 4mm then the ramus of the mandible is used. If the augmentation is for increased vertical height the symphysis is used including its inferior cortical border within the graft. If the recipient site is the anterior mandible the symphysis is used as the donor. Posterior mandible recipient site uses the ramus. A maxillary site uses the ramus as donor too. To prepare for onlay block bone the recipient site is fully exposed to visualise and measure the extent on donor graft needed. The crestal incisions needed are usually lingually made to allow more bulk of keratinised tissue for primary closure. The vertical primary incisions are usually 1 tooth distal from the graft site to allow for more tissue for primary closure again and for good blood supply to the flap. Releasing the periosteum with incisions gains further keratinised tissue for flap closure. Full primary closure of the sutures which are also tension free are needed for success. This needs to be assessed before donor graft is removed. After this has been achieved the cortical bone is perforated with a small diameter drill no bigger than the screws that will be used to fix the graft in place. The holes are 35mm apart over the area to allow the bone to bleed, increasing the availability of revascularisation, bone remodelling and osteogenic/osteoclastogenic cells. It also promotes graft union41,42. Principles of Implant Dentistry Assignment 4 10 Year 2, March 2012 Student ID 1151830 The symphysis graft has a number of advantages to it in harvesting the donor block graft. A good wide and long block of bone can be harvested. The area is away from the ID canal. Access is relatively simple, especially if a patient has a small mouth. However there will likely be trauma to the incisal nerves and neurosensory complications can occur. There can also be difficulty in primary closure due to the strong fraenum’s present and lack of attached gingivae in the lower anterior region. There can also be a change in the facial profile as the chin shape is altered. The symphysis can cause more post operative discomfort relative to the ramus22. The general size rules for the symphysis is to remain 5mm away from the apices of the lower anterior teeth, 5mm for the lower border of the mandible and 5mm mesial to the mental foramen22. There are also limitations for the ramus block graft. Grafts from this area need knowledge of the mandibular nerve. The first limitation is to be aware of how deep the ID nerve lies to the buccal cortical plate. Second is to assess the length and width of the ramus and external oblique ridge in relation to the nerve. If the distance is 10mm in height from the external oblique to the ID nerve then access is better and little risk of paraesthesia. If less than 5mm then the graft width can only be 3mm in width, or there will be risk to the nerve, as the whole graft will be lateral/above the nerve and its canal. The last limit is the width of the ramus. It is wider in males than for females. The block bone grafts are then fixated to the recipient site with titanium screws. Autogenous and other types of particulate graft can be added over the block only graft and a barrier membrane over the whole graft. The flap is then closed with primary closure and tension free sutures. The donor site may have particulate bone and barrier membrane added to regenerate bone. Block bone grafting can be Principles of Implant Dentistry Assignment 4 11 Year 2, March 2012 Student ID 1151830 used to augment vertical and horizontal bone height. There is a good number of sources available that claim the height and width gained is considerable (up to 5.5mm in height) and stable26,43,44 but more studies are needed for long term assessment of bone45. Sinus Augmentation Implant surgery in the posterior maxillae can be complicated by the presence of the maxillary sinuses. The maxillary sinus is the largest of the paranasal sinuses. It is a cavity filled with air bilaterally above the posterior teeth from the region of the upper premolars to the upper molars. The sinus is lined by a schneiderian membrane which is a very thin pseudostratified ciliated membrane. Below the sinus and the schneiderian membrane is the maxillary alveolar ridge and the maxillary teeth. The alveolar bone has external cortical bone in contact with the sinus membrane and internal cortical bone which is in contact with the teeth, mucosa and gingivae. In-between the 2 cortical bone plates is spongy trabecular bone. On some occasions there is insufficient bone height to place an implant and the sinus floor and lining maybe lying low and close to the alveolar crest. There are a few techniques that can be utilised to increase the vertical bone. The most common and longest used methods include the Tatum4647/Open sinus graft through the buccal bone and elevating the sinus laterally. Graft bone of various types can then be added. The other common technique is the Summers/Closed lift48. This involves a crestal approach to the bone near the floor of the sinus lining with osteotomes and/or pilot drill. As the distance reaches close to the sinus, the Principles of Implant Dentistry Assignment 4 12 Year 2, March 2012 Student ID 1151830 bone it is then compacted with use of osteotomes and both the bone and sinus lining is lifted to approximately up to 4-5mm. Obviously if there is adequate space and bone for an implant then a modification to the sinus is not needed. Misch in 198749 devised a classification system for the need of sinus augmentation. The SA classification by Misch is dependent on height of bone available, size of sinus, and width of crestal ridge. In 2006 Misch, Chiapasco and Jensen50 et al developed proposed a new classification. This includes when to not provide sinus augmentation, but also when to provide sinus augmentation via crestal approach or through a full sinus graft by the Tatum lateral window technique. Ideally 12mm of bone height is needed for a conventional implant (depending on type of implant). The technique of adding bone graft into the osteotomy is called Bone Added Osteotome Sinus Floor Elevation (BAOSFE) and was coined by Summers in1994 3. There are risks with adding bone graft materials to the osteotome technique. If too much bone is added, the membrane can tear and the graft material can enter the sinus51,52. There is new written evidence and trials demonstrating that BAOSFE may be of no real value10,53 and there may be no actual need of grafting after elevating the sinus. If further evidence proves this, then the addition of this bone graft could be actually increasing the risks of sinus perforations with no actual real benefit to the patient with unnecessary costs. In soft D3 or D4 type bone of the maxilla it is better to condense bone with a osteotome technique to allow better primary stability of the implant than to use drills. This is a key to Osteointegration and implant success54. With the osteotome technique the bone is condensed laterally through micro fractures with osteotomes and a surgical mallet technique. This generally will require a separate operator for Principles of Implant Dentistry Assignment 4 13 Year 2, March 2012 Student ID 1151830 the gentle malleting. This leaves a stiff wall of dense bone. Maxillary bone is generally soft bone which if condensed will make it thicker and allow the implant to be more stabile. The surgical mallet also can risk the patient to anxiety and discomfort during the malleting. Postoperatively the patient can also suffer from vertigo 55,56. Osteotomes allow better tactile feedback and produce no heat, improving success rates57. Using the osteotome and surgical mallet can be unnerving for some clinicians. There needs to be some experience in its use Open flap technique to the internal/summers lift has been recommended. There are many advantages to open flap surgery. There is direct visualisation of the bony crest, width and existing height. This can prove to be very useful, especially in the inexperienced operator. It can allow good visualisation for correct angulation and placement of the implant. Generally this method is used if there is less than 8mm width of bone. The upper maxilla often has width of 8mm or more. A flapless approach could be used. This would allow better healing and less trauma which is experienced from flap reflection58. The Tatum/Caldwell Luc technique advantage is that there can be large gains in bone height that can be gained. However there is a possibility of tearing the sinus while elevating the sinus or also while adding the bone graft material after elevation. There can be large amounts of post operative swelling, bruising and pain. The technique is complex and done only by competent experienced surgeons. Principles of Implant Dentistry Assignment 4 14 Year 2, March 2012 Student ID 1151830 Bone manipulation techniques Bone manipulation can be used to describe similar techniques. The aim is to manipulate and expand the existing labial/buccal and palatal/lingual cortical bone plates to increase the width of the alveolar bone. It does not aim to increase the ridge height. This in turn will allow for an implant with a diameter wider than the existing alveolar ridge to be placed. The techniques are performed with a variety of instruments to progressively widen the alveolar ridge without fracturing the cortical plates. It can be performed flapless or with a minimal open flap. Bone manipulation includes; ridge splitting and bone expansion. The advantages these techniques have are that there is no increased waiting/healing time to allow ridge augmentation/bone graft to successfully integrate. They also do not rely on patient compliance like distraction osteogenesis. The results from bone manipulation have shown to be stabile over long term59,60. Bone manipulation techniques allow a segment of bone to be displaced into the defect. It also moves the overlying soft tissue overlying the bone, increasing bone and gingivae. Where the ridge has been made is left a crevice that can regenerate new bone. The ridge is therefore enlarged with native mature autogenous bone and soft tissue, which is ideal. It generally allows the existing bone to be preserved instead of being lost from drilling procedures. It also avoids the bone being damaged from the heat developed on drilling. Bone expansion14,61,62 is usually performed by increasingly wider osteotomes being introduced between the 2 cortical plates. A surgical mallet is used to push the osteotome into the bone, however hand pressure can be used in very soft Principles of Implant Dentistry Assignment 4 15 Year 2, March 2012 Student ID 1151830 bone. Ridge splitting63,64 involves a longitudinal split formed by saws or chisels separating the facial and lingual/palatal cortical bone plates. At the end of each split a vertical split is put buccally to help move the buccal plate expand facially65. The lateral split is then gradually enlarged with increasing sizes of chisels till implants are able to fit within the split. Osteotomes may be used in the areas of implant placement. The gaps between the implants and the cortical plates are then filled normally with bone graft material66,67. The technique allows a better tactile feedback as opposed to drilling. The other advantages to osteotomes are that it condenses soft bone for better primary stability to the implant. As there is immediate of the implant, there is no increased morbidity or healing like in the case for onlay grafts. The disadvantages include cases reports of vertigo due to the malleting. There is also an uncertain amount of force being used in the osteotome. Access to the posterior region can be difficult, however offset osteotomes have been made to account for this. Ridge splitting can cause total loss of the buccal plate and a large bone defect if the bone becomes necrotic and fails68. Distraction osteogenesis techniques Distraction Osteogenesis (DO) is a viable and successful alternative to increasing bone in an area deficient. It is a process that forms new bone between two plates of bone which are gradually separated by incremental traction. The two plates of bone are separated by corticotomies and external or internal distractor devices. Osteoblasts and. DO has been used in the mandible since the early 1990’s with success69,70 but it was innovated in 1905 by Codvilla71 but refined and Principles of Implant Dentistry Assignment 4 16 Year 2, March 2012 Student ID 1151830 popularised by the Russian Illizarov72,73. The greatest advantage of DO is that it can increase bone in all 3 planes of dimension using multidirectional distraction devices74,75. There are 4 phases in DO76. The first phase is the surgery in which the osteotomy is performed. Then there is a period of latency of approximately 4-5 days. Then distraction phase. The bone is distracted very slowly at a rate of 0.5mm to 2 mm a day. The last stage is the retention phase. If the distraction is too slow the bone heals over and hardens before completing the lengthening procedure. If too fast then the bone cannot heal in time and close the gap. It also overstretches the soft tissues77,78. DO has been showed to have excellent functional and aesthetic results as in not only increases the amount of bone but the surrounding soft tissue infrastructure79 especially when used in conjunction with dental implants80. The results have been showed to be stable with predictable results increasing vertical and horizontal bone81,82,83 but relapse has been reported84,85. DO has a high success rate86 compared to other forms of bone augmentation. However DO should be only performed by skilful experienced surgeons87. Even then the surgery can cause a number of complications similar to the other types of bone augmentation surgery, such as catastrophic failure from the surgical site and necrosis of the bone88. The distraction can be subjected to uncontrollable forces from surrounding muscles. This can alter and change the final result89. The surgery could involve damage to surrounding vital structures such as nerves 90,82 and lead to visible scarring if external fixators are used. The final problem with DO is that it the result is based on patient compliance86. It is the patient who has to turn the external/internal fixator for the distraction process. If they fail to do so due to compliance issues the result Principles of Implant Dentistry Assignment 4 17 Year 2, March 2012 Student ID 1151830 will be limited. Some patients have reported that the fixators are uncomfortable and bulky86,91. Other Techniques Vertical osteotomy92,93,94,95 can be used as an alternative to DO. There is a limitation to the amount of height gained (5mm) but has had stabile results documented 95. The most common technique is making a horizontal cut 10mm from the alveolar crest and vertical crests to connect it, after reflecting a full thickness flap. The cuts are made normally using reciprocating saws. This segment is then freed and moved 5mm vertically. The space interpositionally was then filled with particulate graft or block autogenous graft. The wound is then sutured gaining primary closure. This technique is aimed at only achieving vertical bone height for implants. Fixation was not generally needed but could be placed. This technique has been reported to be comparable and superior to onlay bone grafting96,97 as the surgery is 1 off, there is less patient compliance for height gains and less chances of complications. The disadvantage to this technique is that width cannot be improved greatly. There is also the risk of devascularising the segment of bone and cause complete failure of the surgery. Inferior dental nerve lateralisation98,99 is a technique where the inferior dental/alveolar (ID nerve) or mental nerve is laterally moved. This is often an option when the ID nerve is situation high up vertically, resulting in insufficient vertical depth to place implants. The ID nerve is located and the buccal bone overlying the canal is removed carefully. The bone was traditionally removed by burs but it is more advantageous to use with the peizo surgery device which can Principles of Implant Dentistry Assignment 4 18 Year 2, March 2012 Student ID 1151830 remove bone with less chance of traumatising the soft tissues100. However damage to the nerve by brute mechanical force is still a possibility. Also the peizo surgery removes bone very slowly, so the duration of the operation is longer for the patient. This is another advanced technique that should only be completed by capable and experienced dental and oral surgeons. . Conclusion All the available techniques have shown advantages and disadvantages. However there is a substantial lack of good long term data and evidence indicating long term results and stability of each technique101,102. As such it is difficult to choose which technique to apply in certain situations. Some techniques like bone expansion and ridge splitting is able to only alter the horizontal width of bone and not the vertical bone. Common sense should therefore be applied to each individual case. The option which will provide the least trauma, the least complications and still result in long term success should be offered to the patient. For example DO would not necessarily be in the patient’s if 1 tooth was missing in the arch. As such further good quality long term trials are needed to fully compare and critique which bone augmentation technique truly provides the best option for the patient. Principles of Implant Dentistry Assignment 4 19 Year 2, March 2012 Student ID 1151830 List of References 1 Brown, K. L. B.; Cruess, R. L. Bone and cartilage transplantation in orthopaedic surgery. J. Bone Jt. Surg. 64A1270-279; 1982 2 Christopher J. Damien and J. Russell Parsons George L. Bone Graft and Bone Graft Substitutes: A Review of Current Technology and Applications ~Schultz Laboratories for Orthopaedic Research, Department of Surgery, Section of Orthopaedics, UMDNJ-New Jersey Medical School, Newark, New Jersey 3 Agarwal R, Williams K, Umscheid CA, Welch WC Osteoinductive bone graft substitutes for lumbar fusion: a systematic review J Neurosurg Spine. 2009 Dec;11(6):729-40. 4 Chai F, Raoul G, Wiss A, Ferri J, Hildebrand HF [Bone substitutes: Classification and concerns]. Rev Stomatol Chir Maxillofac. 2011 Sep;112(4):212-21. Epub 2011 Jul 23. 5 Hosny M. Recent concepts in bone grafting and banking. Erratum in Cranio 1987 Jul;5(3):289. Principles of Implant Dentistry Assignment 4 20 Year 2, March 2012 Student ID 1151830 6 Narang R, Wells H, Laskin DM. Ridge augmentation with decalcified allogeneic bone matrix grafts in dogs. J Oral Surg. 1972 Oct;30(10):722-6 7 Dodd CAF, Fergusson CM, Freedman L, et al: Allograft versus autograft bone in scoliosis surgery. J Bone Joint Surg Br 70:431, 1988 8 Grover V, Kapoor A, Malhotra R, Sachdeva S. Bone allografts: a review of safety and efficacy. Indian J Dent Res. 2011 May-Jun;22(3):496. 9 Viscioni A, Dalla Rosa J, Paolin A, Franco M Fresh-frozen bone: case series of a new grafting material for sinus lift and immediate implants. J Ir Dent Assoc. 2010 Aug-Sep;56(4):186-91. 10 Cintia Mussi Milani Contar, João Rodrigo Sarot, ,Jayme Bordini, Gustavo Holtz Galvão,Gastão Vale Nicolau, Maria Angela Naval Machado, Maxillary Ridge Augmentation With Fresh-Frozen Bone Allografts Dental implants 11 Kleczar H, Kozdoń L, Piasecki J. [Clinical and radiological assessment of the results of using grafts of allogenic lyophilized spongy bone for filling of large postoperative jaw bone defects]. Czas Stomatol. 1990 Mar;43(3):148-53. Principles of Implant Dentistry Assignment 4 21 Year 2, March 2012 Student ID 1151830 12 J Can Dent Assoc. 2012 Feb;78:c15. Preservation of posterior mandibular extraction site with allogeneic demineralized, freeze-dried bone matrix and calcium sulphate graft binder before eventual implant placement: a case series. Almasri M, Camarda AJ, Ciaburro H, Chouikh F, Dorismond SJ. 13 J Periodontol. 2012;83(3):329-36. Epub 2011 Jul 12. Histologic comparison of healing after tooth extraction with ridge preservation using mineralized versus demineralized freeze-dried bone allograft. Wood RA, Mealey BL. 14 Int J Oral Maxillofac Implants. 2009 Jul-Aug;24(4):609-15. Comparative histomorphometric analysis of extraction sockets healing implanted with bovine xenografts, irradiated cancellous allografts, and solvent-dehydrated allografts in humans. Lee DW, Pi SH, Lee SK, Kim EC 15 J Oral Surg. 1974 Sep;32(9):674-8. Irradiated allogeneic bone grafts in the treatment of odontogenic cysts. Spengos MN. 16 Journal of Periodontology February 2001, Vol. 72, No. 2, Pages 215-229 , DOI 10.1902/jop.2001.72.2.215 Collagen Membranes: A Review Pintippa Bunyaratavej 17 Implant Dent. 2011 Aug;20(4):267-72. Ridge preservation of the molar extraction socket using collagen sponge and xenogeneic bone grafts. Kim YK, Yun PY, Lee HJ, Ahn JY, Kim SG Principles of Implant Dentistry Assignment 4 22 Year 2, March 2012 Student ID 1151830 18 A bone regenerative approach to alveolar ridge maintenance following tooth extraction. Report of 10 cases. Lekovic V, Kenney EB, Weinlaender M, Han T, Klokkevold P, Nedic M, Orsini M. J Periodontol. 1997 Jun;68(6):563-70 19 J Periodontol. 1998 Sep;69(9):1044-9. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M. 20 Int J Periodontics Restorative Dent. 2003 Aug;23(4):313-23. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Schropp L, Wenzel A, Kostopoulos L, Karring T. 21 J Periodontol. 2003 Jul;74(7):990-9. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. Iasella JM, Greenwell H, Miller RL, Hill M, Drisko C, Bohra AA, Scheetz JP 22 Misch CE, Suzuki JB. Tooth extraction, socket grafting, and barrier membrane bone regeneration. In: Contemporary Implant Dentistry. 3rd ed. St Louis, MO: Mosby; 2007:870-904 Principles of Implant Dentistry Assignment 4 23 Year 2, March 2012 Student ID 1151830 23 J Periodontol. 2010 Jun;81(6):801-8. Immediate placement of implants into infected sites: a systematic review of the literature. Waasdorp JA, Evian CI, Mandracchia M. 24 British Dental Journal 201, 199 - 205 (2006) Published online: 26 August 2006 Immediate implant placement: treatment planning and surgical steps for successful outcomes W Becker 25 Int J Oral Maxillofac Implants. 2012 Jan-Feb;27(1):194-202. A retrospective analysis of immediately placed implants in 418 sites exhibiting periapical pathology: results and clinical considerations. Fugazzotto P 26 Clin Implant Dent Relat Res. 2009 Oct;11 Suppl 1:e69-82. Epub 2009 Aug 3. Inlay versus onlay iliac bone grafting in atrophic posterior mandible: a prospective controlled clinical trial for the comparison of two techniques. Felice P, Pistilli R, Lizio G, Pellegrino G, Nisii A, Marchetti C 27 Guided tissue regeneration in jawbone defects prior to implant placement N. P. Lang, C. H. F. Hämmerle, U. Brägger, B. Lehmann, S Clinical Oral Implants Research Volume 5, Issue 2, pages 92–97, June 1994 28 Clin Oral Implants Res. 1990 Dec;1(1):22-32. Regeneration and enlargement of jaw bone using guided tissue regeneration. Buser D, Brägger U, Lang NP, Nyman S. Principles of Implant Dentistry Assignment 4 24 Year 2, March 2012 Student ID 1151830 29 . Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Cordaro L, Amadé DS, Cordaro M. Clin Oral Implants Res. 2002 Feb;13(1):103-11. 30 Inlay-onlay grafting for three-dimensional reconstruction of the posterior atrophic maxilla with mandibular bone. Cordaro L, Torsello F, Accorsi Ribeiro C, Liberatore M, Mirisola di Torresanto V. Int J Oral Maxillofac Surg. 2010 Apr;39(4):350-7. Epub 2010 Mar 17 31 Effect of bovine bone and collagen membranes on healing of mandibular bone blocks: a prospective randomized controlled study. Cordaro L, Torsello F, Morcavallo S, di Torresanto VM. Clin Oral Implants Res. 2011 Oct;22(10):1145-50. Epub 2011 Feb 11. 32 The use of intraorally harvested autogenous block grafts for vertical alveolar ridge augmentation: a human study. Proussaefs P, Lozada J. Int J Periodontics Restorative Dent. 2005 Aug;25(4):351-63. Principles of Implant Dentistry Assignment 4 25 Year 2, March 2012 Student ID 1151830 33 The use of ramus autogenous block grafts for vertical alveolar ridge augmentation and implant placement: a pilot study. Proussaefs P, Lozada J, Kleinman A, Rohrer MD. Int J Oral Maxillofac Implants. 2002 Mar-Apr;17(2):238-48. 34 Swed Dent J Suppl. 2011;(211):11-66. Intra-oral soft tissue expansion and volume stability of onlay bone grafts. Abrahamsson P. 35 Reconstruction of the Defective Mandible 1975, Vol. 9, No. 2 , Pages 116-128 P.-I. Brånemark1, J. Lindström1, O. Hallén1, U. Breine1, P.-H. Jeppson1 and A. Öhman1 36 Autogenous mandibular bone grafts and osseointegrated implants for reconstruction of the severely atrophied maxilla: A preliminary report John Jensen, Steen Sindet-Pedersen, Journal of Oral and Maxillofacial Surgery Volume 49, Issue 12, December 1991, Pages 1277–1287 37 Int J Oral Maxillofac Implants. 1992 Fall;7(3):360-6. Reconstruction of maxillary alveolar defects with mandibular symphysis grafts for dental implants: a preliminary procedural report. Misch CM, Misch CE, Resnik RR, Ismail YH. Principles of Implant Dentistry Assignment 4 26 Year 2, March 2012 Student ID 1151830 38 Quantitative assessment of early healing of intramembranous and endochondral autogenous bone grafts using micro-computed tomography and Q-win image analyzer M Lu, A.B.M Rabie International Journal of Oral and Maxillofacial Surgery ,Volume 33, Issue 4, June 2004, Pages 369–376 39 The early revascularization of membranous bone. Kusiak JF, Zins JE, Whitaker LA Plastic and Reconstructive Surgery [1985, 76(4):510-6] 40 Plastic & Reconstructive Surgery: August 1998 - Volume 102 - Issue 2 - pp 291-299 Volume Maintenance of Onlay Bone Grafts in the Craniofacial Skeleton: Microarchitecture versus Embryologic Origin Ozaki, Wayne M.D., D.D.S.; Buchman, Steven R. M.D. 41 Am J Orthod Dentofacial Orthop. 2011 Apr;139(4 Suppl):S83-101. Mechanism of action and morphologic changes in the alveolar bone in response to selective alveolar decortication-facilitated tooth movement. Baloul SS, Gerstenfeld LC, Morgan EF, Carvalho RS, Van Dyke TE, Kantarci A. Principles of Implant Dentistry Assignment 4 27 Year 2, March 2012 Student ID 1151830 42 Clin Implant Dent Relat Res. 2012 Mar;14(1):112-20. Clinical, tomographic, and histological assessment of periosteal guided bone regeneration with cortical perforations in advanced human critical size defects. Verdugo F, D'Addona A, Pontón J. 43 Int J Oral Maxillofac Surg. 2010 Apr;39(4):350-7. Inlay-onlay grafting for three-dimensional reconstruction of the posterior atrophic maxilla with mandibular bone. Cordaro L, Torsello F, Accorsi Ribeiro C, Liberatore M, Mirisola di Torresanto V 44 Clin Oral Implants Res. 2009 Dec;20(12):1386-93 Vertical ridge augmentation of the atrophic posterior mandible with interpositional bloc grafts: bone from the iliac crest vs. bovine anorganic bone. Clinical and histological results up to one year after loading from a randomized-controlled clinical trial. Felice P, Marchetti C, Iezzi G, Piattelli A, Worthington H, Pellegrino G, Esposito M. 45 J Clin Periodontol. 2008 Sep;35(8 Suppl):203-15. Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. Rocchietta I, Fontana F, Simion M. 46 H. Tatum Maxillary subantral grafting. Lecture Alabama Implant Study Group 1977 Principles of Implant Dentistry Assignment 4 28 Year 2, March 2012 Student ID 1151830 47 H. Tatum, Maxillary and sinus implant reconstructions. Dent Clin North Am, 30 (1986), p. 207 48 Summers RB. A new concept in maxillary implant surgery: The osteotome technigue. Comped Contin Educ Dent 1994; 15: 152-160 49 Misch CE. Maxillary sinus augmentation for endosteal implants. Organized alternative treatments plans. Int J Oral Implantol 1987;4:49-58 50 Misch, Chiapasco and Jensen Indication for and classification of sinus grafts 2006 Quintessence 51 Endoscopic evaluation of the bone-added osteotome sinus floor elevation procedure M. Berengo, S. Sivolella, Z. Majzoub, G. Cordioli International Journal of Oral and Maxillofacial Surgery Volume 33, Issue 2, March 2004, Pages 189-194 52 Hernandez-Alfaro F, Torradeflot MM, Marti C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin Oral Implants Res. 2008;19:91–98. Principles of Implant Dentistry Assignment 4 29 Year 2, March 2012 Student ID 1151830 53 Transcrestal Sinus Floor Elevation: A Retrospective Study of 46 Patients up to 16 Years Giovanni B Bruschi, Roberto Crespi, Paolo Capparè, Enrico Gherlone 53 26 OCT 2010 Clinical Implant Dentistry and Related Research Summers RB. A new concept in maxillary implant surgery: The osteotome technique. Compendium of Dental Education 1994;15:152, 154-156, 158 passim 54Paroxysmal positional vertigo as a complication of osteotome sinus floor elevation Michele Di Girolamo, Bianca Napolitano, Carlo Andrea Arullani, Ernesto Bruno and Stefano Di Girolamo European Archives of Oto-Rhino-Laryngology Volume 262, Number 8, 631-633, 56 An unusual complication of osteotome sinus floor elevation: benign paroxysmal positional vertigo International Journal of Oral and Maxillofacial Surgery Volume 40, Issue 2, February 2011, Pages 216-218 S. Vernamonte, V. Mauro, 57 Heat generation during implant placement in low-density bone: effect of surgical technique, insertion torque and implant macro design. Marković A, Mišić T, Miličić B, Calvo-Guirado JL, Aleksić Z, Dinić A. Clin Oral Implants Res. 2012 Apr 2 Principles of Implant Dentistry Assignment 4 30 Year 2, March 2012 Student ID 1151830 58 Contemporary implant dentistry. 3rd edition C Misch Pg 673-678 59 Marginal bone stability using 3 different flap approaches for alveolar split expansion for dental implants: a 1-year clinical study. Jensen OT, Cullum DR, Baer D. J Oral Maxillofac Surg. 2009 Sep;67(9):1921-30 60 A 10-year multicenter retrospective clinical study of 1715 implants placed with the edentulous ridge expansion technique. Bravi F, Bruschi GB, Ferrini F. Int J Periodontics Restorative Dent. 2007 Dec;27(6):557-65 61 Dennis Flanagan (2002) Cortical Bone Spreader Osteotome and Method for Dental Implant Placement. Journal of Oral Implantology: December 2002, Vol. 28, No. 6, pp. 295-296. 62 J Oral Implantol. 1999;25(1):18-22. Aesthetic enhancement of anterior dental implants with the use of tapered osteotomes and soft tissue manipulation. Silverstein LH, Kurtzman GM, Moskowitz E, Kurtzman D, Hahn J. 63 Compend Contin Educ Dent. 2008 Mar;29(2):106-10. Ridge-splitting technique with simultaneous implant placement. Koo S, Dibart S, Weber HP. Principles of Implant Dentistry Assignment 4 31 Year 2, March 2012 Student ID 1151830 64 Int J Periodontics Restorative Dent. 1999 Jun;19(3):269-77. Bone regeneration in the edentulous ridge expansion technique: histologic and ultrastructural study of 20 clinical cases. Scipioni A, Bruschi GB, Calesini G, Bruschi E, De Martino C. 65 Int J Periodontics Restorative Dent. Vol 25 no2 2005 Alveolar Ridge Splitting Jong Jin Suh 66 Ridge splitting and implant techniques for the anterior maxilla. Ady Palti in Dental Implantology Update (2003) 67 Int J Oral Maxillofac Implants. 2006 May-Jun;21(3):445-9. Preliminary report on a staged ridge splitting technique for implant placement in the mandible: a technical note. Enislidis G, Wittwer G, Ewers R. 68 Oral Maxillofac Surg Clin North Am. 2004 Feb;16(1):65-74, vi. Implant site development using ridge splitting techniques. Misch CM. 69 McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH: Lengthening of the human mandible by gradual distraction. Plast Reconst Surg 1992, 89:1-10. PubMed Abstract Principles of Implant Dentistry Assignment 4 32 Year 2, March 2012 Student ID 1151830 70 Pensler JM, Goldberg DP, Lindell B, Carroll NC: Skeletal distraction of the hypoplastic mandible. Ann Plast Surg 1995, 34:130-137 71 Codivilla A. On the means of lengthening in the lower limbs, the muscles and tissues which are shortened through deformity. Am J Orthop Surg 1905;2:35369. 72 Illizarov GA. A new principle of osteosynthesis with the use of crossing pins and rings. In collection of scientific works of the Kurgan Regional scientific medical society. Kurgan: USSR; 1954. p. 145-60. 73 Illizarov GA. The principles of Illizarov method. Bull Hosp Joint Dis Orthop Inst 1988;48:1-11 74 Distraction osteogenesis in a severe mandibular deficiency Kerim Ortakoglu1, Seniz Karacay2, Metin Sencimen1*, Erol Akin2, Aykut H Ozyigit1 and Osman Bengi2 Head & Face Medicine 2007, 3:7 75 Gateno J, Teichgraeber JF, Aguilar E: Distraction osteogenesis: A new surgical technique for use with the multiplanar mandibular distractor. Plast Reconst Surg 2000, 105:883-888 Principles of Implant Dentistry Assignment 4 33 Year 2, March 2012 Student ID 1151830 76 J Plast Reconstr Aesthet Surg. 2009 Dec;62(12):1568-72 Effects of hyperbaric oxygen therapy on an accelerated rate of mandibular distraction osteogenesis. Salgado CJ, Raju A, Licata L, Patel M, Rojavin Y, Wasielewski S, Diarra C, Gordon A, Norcross A, Kent KA 77 Plast Reconstr Surg. 2005 Mar;115(3):831-7. The effect of rate of distraction osteogenesis on structure and function of anterior digastric muscle fibers. van der Meulen JH, Borschel GH, Lynch JB, Nicklin S, Ho KC, Gianoutsos MP, Walsh WR, Kuzon WM Jr 78 Journal of Cranio-Maxillofacial Surgery Volume 26, Issue 1, February 1998, Pages 43–49 Mandibular distraction osteogenesis: a comparison of distraction rates in the rabbit model K.J. Stewart, G.O. Lvoff, S.A. White, S.F. Bonar, W.R. Walsh, R.C. Smart, Michael D. Poole 79 Molina F, Monasterio FO. Mandibular elongation and remodeling by distraction: a farewell to major osteotomies. Plast Reconstr Surg 1995;96:825-42. 80 Chin Med J (Engl). 2008 Oct 5;121(19):1861-5. Clinical outcome of dental implants placed in fibula-free flaps for orofacial reconstruction. Wu YQ, Huang W, Zhang ZY, Zhang ZY, Zhang CP, Sun J. Principles of Implant Dentistry Assignment 4 34 Year 2, March 2012 Student ID 1151830 81 Hollier LH, Kim JH, McCarthy JG. Mandibular growth after distraction in patients under 48 months of age. Plast Reconstr Surg 1999;103:1361-70. 82Grayson BH, Santiago PE. Treatment planning and biomechanics of distraction osteogenesis from an orthodontic perspective. Semin Orthod 1999;5:9-16. 83 Carls FR, Sailer HF. Seven years clinical experience with mandibular distraction in children. J Maxillofac Surg 1998;26:197-208. 84 Marquez IM, Fish LC, Stella JP. Two year followup of distraction osteogenesis: its effects on mandibular ramal height in hemifacial microsomia. Am J Orthod Dentofac Orthop 2000;117:130-9 85 Huang CS, Ko WC, Lin WY, Liou EJ, Hong KF, Chen YR. Mandibular lengthening by distraction osteogenesis in children-a one year followup study. Cleft Plate Craniofac J 1999;36:269-74 86 Mandibular functional reconstruction using internal distraction osteogenesis. Wang X, Lin Y, Yi B, Wang X, Liang C, Li Z. Chin Med J (Engl). 2002 Dec;115(12):1863-7 87 World J Surg Oncol. 2005 Feb 3;3(1):7. A novel surgical procedure for bridging of massive bone defects. Knothe UR, Springfield DS Principles of Implant Dentistry Assignment 4 35 Year 2, March 2012 Student ID 1151830 88 J Indian Soc Pedod Prev Dent. 2006 Mar;24(1):30-9. Long term results of mandibular distraction. Batra P, Ryan FS, Witherow H, Calvert ML. 89 McCarthy JG, Stelnicki EJ, Grayson BH. Distraction osteogenesis of the mandible: a ten year experience. Semin Orthod 1999;5:3-8 90 Int J Oral Maxillofac Surg. 2005 May;34(3):238-42. Patients' responses to distraction osteogenesis: a multi-centre study. Primrose AC, Broadfoot E, Diner PA, Molina F, Moos KF, Ayoub AF. 91Rev Stomatol Chir Maxillofac. 2011 Sep;112(4):229-32. [Improvement of maxillofacial bone distraction osteogenesis: future prospects]. Wojcik T, Touzet S, Ferri J, Schouman T, Raoul G. 92 J Oral Implantol. 2008;34(6):313-8. Vertical alveolar ridge expansion and simultaneous implant placement in posterior maxilla using segmental osteotomy: report of two cases. Fujita A 93 J Oral Maxillofac Surg. 2011 Sep;69(9):2339-44. Epub 2011 Jul 28. Posterior maxillary segmental osteotomy concomitant with sinus lift using a piezoelectric device. Hwang JH, Jung BY, Lim CS, Cha IH, Park W. Principles of Implant Dentistry Assignment 4 36 Year 2, March 2012 Student ID 1151830 94 Oral Maxillofac Surg Clin North Am. 2011 May;23(2):301-19, vi. Orthognathic and osteoperiosteal flap augmentation strategies for maxillary dental implant reconstruction. Jensen OT, Ringeman JL, Cottam JR, Casap N. 95J Oral Maxillofac Surg. 2006 Feb;64(2):290-6. Alveolar segmental sandwich osteotomy for anterior maxillary vertical augmentation prior to implant placement. Jensen OT, Kuhlke L, Bedard JF, White D 96 D.E. Frost, J.M. Gregg, B.C. Terry et al. Mandibular interpositional and onlay bone grafting for treatment of mandibular bony deficiency in the edentulous patient J Oral Maxillofac Surg, 40 (1982), p. 353 97 T. Chow, C. Yu, S. Fung et al. Pyriform rim osteotomyA new regional osteotomy for correction of a para-alar deficiency J Oral Maxillofac Surg, 62 (2004), p. 259 98 Rev Stomatol Chir Maxillofac. 1995;96(3):171-4. [Complete lateralization of the inferior alveolar nerve. A preliminary study, apropos of a case]. Chossegros C, Cheynet F, Aldegheri A, Blanc JL Principles of Implant Dentistry Assignment 4 37 Year 2, March 2012 Student ID 1151830 99 Int J Oral Maxillofac Implants. 2002 Jan-Feb;17(1):101-6. Lateralization of the inferior alveolar nerve with simultaneous implant placement: a modified technique. Peleg M, Mazor Z, Chaushu G, Garg AK 100 Transposition of the mental nerve by piezosurgery followed by postoperative neurosensory control: A case report Nikolaos Sakkas, Joerg-Elard Otten, Ralf Gutwald, Rainer Schmelzeisen 101 Int J Oral Maxillofac Implants. 2009;24 Suppl:237-59. Bone augmentation procedures in implant dentistry. Chiapasco M, Casentini P, Zaniboni M. 102 Clin Oral Implants Res. 2006 Oct;17 Suppl 2:136-59. Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Chiapasco M, Zaniboni M, Boisco M Principles of Implant Dentistry Assignment 4 38 Year 2, March 2012 Student ID 1151830