Document 6826638
advertisement

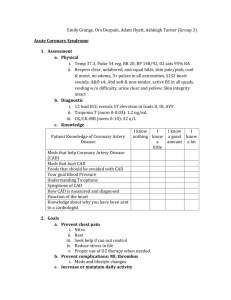
This is a 43-year-old female patient that was admitted to the ER on 8/31/13 for chest pain and shortness of breath. Patient stated that it began 3 days ago. According to the patient, the pain is located in the sternum and it is a constant, aching pain. She was unable to identify any precipitating or alleviating factors. The chest discomfort is not necessarily brought on by exertion or emotional stress. She has noticed some shortness of breath with exertion, which has been worse for the past few days. She has no orthopnea but noticed swelling in both of her lower extremities. She denies any palpitations, dizzy spells, or syncope episodes. The patient states that the most recent chest pain was prior to her presentation to the emergency room and lasted for at least 3 hours. Her initial EKG in the ER was normal sinus rhythm without any acute changes. A chest x-ray showed prominent pulmonary vasculature consistent with pulmonary edema, and cardiac enzymes came back negative. Her blood pressure was significantly elevated on presentation to the ER. She stated that she hadn’t been taking her medications once she ran out. The patient was initially started on BiPAP. Her condition was quickly reversed with IV Diuretics and her home antihypertensive medication. On September 3rd, she received a CT Thorax which revealed her heart to be moderately enlarged and the pulmonary outflow tract to be enlarged as well. The findings are suspicious of Pulmonary Hypertension. An outpouching over the heart was also noticed. The patient is currently awaiting for her scheduled abdominal ultrasound at some point today (9/3/13). The patient now understands why she was hospitalized (verbal understanding). Patient teaching was specific to coronary artery disease. Patient Teaching: o Pathophysiology- According to Mayo Clinic, the coronary arteries are major blood vessels that supply the heart with oxygen, blood, and nutrients. When the coronary arteries become damaged or diseased, there is a reduced flow of oxygen, blood, and nutrients and we call this coronary artery disease. o Causes- Arteriosclerosis is one way of reducing the oxygen and nutrient flow; in o arteriosclerosis, the arterial wall thickens, has reduced elasticity, and calcifies. Atherosclerosis, the condition in which plaque builds up inside one’s arteries, is the most common cause of reduced blood flow to the myocardium. Usually coronary arteries can dilate and increase the force of contraction to increase the blood flow and cardiac output but in Coronary Artery Disease, the plaque causes difficulty for the arteries to dilate and brings forth calcification. Contributing Factors- older age, male gender, family history, smoking, high blood pressure, diabetes, high cholesterol, obesity, physical inactivity, high stress, and even radiation therapy. o Symptoms- The reduced flow of oxygen brings about symptoms such as chest pain, shortness of breath, and even heart attack. o Diagnosis- An ECG can show you if a heart attack is under way, while the Echocardiogram will show you if all parts of the heart are working properly and /or any damage to any part of the heart. A CT scan will most often be done to look at your arteries closer. Another option is to have an angiogram, for which a dye is injected into the arteries of your heart to see the blood flow through the o o o o o o heart. Vitals and cardiac enzymes are other ways of showing signs of coronary artery disease/heart disease in general. Medications- Review of meds in next section. Nutrition-Patient needs to follow a cardiac diet low in fats, cholesterol, and salt. Avoid canned foods and fast foods especially. Rehabilitation- Patient should learn to take her own blood pressure and know the acceptable ranges for blood pressure. In addition, she should know what values are acceptable for cholesterol and get hers checked as recommended. Lastly, she needs to keep her diabetes under control; so, check blood sugar daily. Additional Treatments- Patient needs to make lifestyle changes. She should eat healthier, exercise more, lose excess weight, and reduce her stress. Community Resources- American Heart Association has rehab programs designed to help patients understand their heart problems better as well as help patients increase his/her physical activity, manage/reduce their cardiac symptoms, and prevent further heart problems. Discharge Instructions-Patient will verbalize understanding of taking medications as directed. If a medication is suspected not to work, patient should contact her primary doctor. Do not stop medications at any point without speaking to the doctor first. If any sort of allergic reaction to a medication is suspected, call the doctor. Patient should learn how to check her own blood pressure and blood sugar and get in the habit of monitoring both daily; she should learn what the accepted ranges are. Patient should also get her cholesterol levels checked by her doctor as recommended. Patient should ask her doctor about joining a cardiac rehab program and arrange meetings to assist her make lifestyle changes as well as prevent further issues. Patient should ask about follow up appointments and schedule those as well. Patient will state her understanding of contacting a caregiver if she feels light headed, her heart is pounding, or if she simply has any questions or concerns regarding her health status and/or medications. Patient must call 911 immediately if she feels sweaty, short of breath, and a heavy pain in her chest that radiates to her back, shoulders, arms, jaw, or neck. A handout has been given to the patient with all this information. Core measures- Patient received an EKG and a chest x-ray at the ER the day of admission (8/31/13). In addition, cardiac enzymes were looked at and came back negative (8/31/13). Patient also received IV diuretics and antihypertensive meds immediately (8/31/13). Nitroglycerin has been given as needed- last dated was 9/3/13. Patient will be discharged with orders to continue her home medications. Patient quit smoking 10 years ago, so smoking cessation teaching was not needed. Medications for Discharge Aspirin: antiplatelet (prevents aggregation of platelets) -Patient Teaching: o Take medication as prescribed (correct dosage) with a full glass of water and remain in an upright position for 15-30 minutes after administration. o Patient should report any tinnitus, unusual bleeding of the gums, bruising, black, tarry stools, or a fever lasting more than 3 days. o Patient should avoid alcohol when taking this medication to avoid stomach irritation. o Patient should avoid effervescent tablets or buffered-aspirin preparations. o Discard any tablet with an acetic (vinegar-like) odor. o Lastly, patient should inform health care professional of aspirin use if she is to receive surgery. -Side Effects: dyspepsia, nausea, anemia, tinnitus, GI bleeding, allergic reactions, anaphylaxis, and laryngeal edema. Lisinopril: antihypertensive/ace inhibitor (manages hypertension) -Patient Teaching: o Patient must take medication as prescribed-at the same time each day, even if they are feeling well. o Do not stop taking med unless told to do so by a healthcare professional. o Do not double dose. However, if you miss a dose, take it as soon as you remember unless it is time for the next dose. o Patient should avoid salt substitutes containing potassium or foods containing high levels of potassium or sodium. o Change positions slowly to avoid orthostatic hypotension. o Consult a healthcare professional before taking any OTC cough, cold, allergy, or herbal products. o Lisinopril can cause dizziness so avoid driving and other activities that require alertness. o Inform a healthcare professional of the use of Lisinopril before surgery. o Notify a healthcare provider if a rash, mouth sores, sore throat, fever, swelling of the hands, feet, face, eyes, lips, or tongue, irregular heartbeat, chest pain, dry cough, or if difficulty swallowing or breathing occurs. o Notify healthcare provider if a persistent dry cough occurs and becomes bothersome. o Emphasize importance of follow-up exams to evaluate medication effectiveness. o Advise patient to check BP weekly at least and report significant changes to provider. -Side Effects: dizziness, cough, hypotension, chest pain, impaired renal function, hyperkalemia, and angioedema. Metformin: antidiabetic (manages type 2 diabetes) -Patient Teaching: o Patient needs to take medication as directed at the same time each day. o Do not double dose. o Take missed dose as soon as remembered, unless it’s time for the next dose. o Teach patient Metformin does not cure diabetes but helps control it. o Teach patient signs of hypoglycemia and hyperglycemia. If hypoglycemia occurs, patient should drink a glass of orange juice or 2-3 teaspoons of sugar, honey, or corn syrup dissolved in water and notify the healthcare provider. o Teach patient how to properly test blood sugar levels and urine ketones. o Explain to the patient the risk of lactic acidosis, teach them of its symptoms (chills, diarrhea, dizziness, low BP, muscle pain, sleepiness, slow heartbeat or pulse, dyspnea, and/or weakness), and to report any symptoms immediately. o Notify a healthcare provider before taking any other medications or alcohol. o Explain to the patient that he/she may experience a metallic taste from metformin and that it will resolve. o Report any occurrence of diarrhea, n/v, stomach pain or fullness to a healthcare provider. o Advise patient to carry sugar packets and/or candy and id describing disease and medication regimen at all times. o Explain the importance of follow up exams and testing of blood sugars, glycosylated hemoglobin, renal function, and hematologic parameters. Side Effects: abdominal bloating, diarrhea, n/v, unpleasant metallic taste, hypoglycemia, lactic acidosis. Metoprolol-antihypertensive/beta blocker (for hypertension, angina pectoris, prevention of MI) Patient Teaching: o Patient needs to take medication as directed at the same time each day. o Do not double dose. o Take missed dose as soon as remembered, unless it’s time for the next dose. o Abrupt withdrawal may precipitate life threatening arrhythmias, hypertension, or MI. o Change positions slowly to avoid orthostatic hypotension. o Metoprolol can cause dizziness so avoid driving and other activities that require alertness. o Advise patient to check pulse and BP biweekly and report significant changes to provider. o Caution patient that this med may cause an increased sensitivity to cold. o Notify healthcare provider if planning to take any other Rx, OTC meds, vitamins, or herbal products with this medication. o Avoid excessive amounts of coffee, tea, and cola. o Diabetics should closely monitor blood glucose levels. Med does not block sweating as a sign of hypoglycemia. o Notify healthcare provider if slow pulse, difficulty breathing, wheezing, cold hands/feet, dizziness, light-headedness, confusion, depression, rash, fever, sore throat, unusual bleeding, or bruising occurs. o Advise patient to carry id describing disease process and medication regimen at all times. Side Effects: fatigue, weakness, memory loss, mental status changes, blurred vision, wheezing, hypotension, bradycardia, heart failure, pulmonary edema, erectile dysfunction, drug induced hepatitis, dry mouth, increased liver enzymes, hyperglycemia, hypoglycemia, arthralgia, back pain, druginduced lupus syndrome. Crestor-lipid lowering agent/ statin (lowers total cholesterol, LDL cholesterol, and triglycerides and slightly increases HDL cholesterol. It also slows the progression of coronary atherosclerosis.) Patient Teaching: o Patient needs to take medication as directed. o Do not skip doses or double dose. o Take missed dose as soon as remembered, unless it’s within 12 hours of the next dose. o Use medication in conjunction with diet restrictions, exercise, and smoking cessation. o Notify healthcare provider if unexplained muscle pain, tenderness, or weakness occurs, esp if accompanied by fever or malaise. o Advise patient to take magnesium or aluminum containing antacids if needed at least two hours after taking medication. o Notify healthcare provider if planning to take any other Rx, OTC meds, vitamins, or herbal products with this medication. o Emphasize the importance of follow up exams to determine effectiveness and to monitor side effects. o Notify healthcare provider of Crestor use before surgery. Side Effects: weakness, abdominal pain, constipation, rash, drug induced hepatitis, high liver function tests, and rhabdomyolysis. Home Assessment- Patient lives in a one story house with her daughter and the environment is safe. Patient is able to care for herself, and her daughter is available and willing to help her if she needs it. Patient relies on financial assistance to pay for her medications and has a means of transportation to pick up her medications. Follow-Up- Patient is planning to follow up with a Cardiologist and has yet to schedule an appointment. Patient does not require home health services or any medical devices to use at home. Dietary consult is needed to help patient follow a more healthy diet low in fats, salt, and cholesterol. Summary- Patient has been seen for chest pain and shortness of breath. Patient education revolved around Coronary Artery Disease for this patient. Medication compliance was strictly emphasized to keep her health well. Patient also needs to look into cardiac rehab and follow with a dietician to help guide her eat healthier foods. This will help prevent the patient’s coronary arteries from worsening and being readmitted for further related issues.