File
advertisement

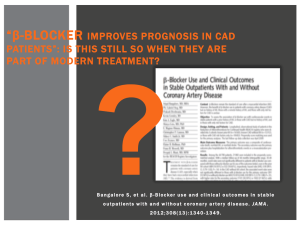
Emily Grange, Ora Despain, Adam Hyatt, Ashleigh Turner (Group 3) Acute Coronary Syndrome 1. Assessment a. Physical i. Temp 37.3, Pulse 54 reg, RR 20, BP 148/92, 02 sats 95% RA ii. Respers clear, unlabored, and equal bilat; skin pale/pink, cool & moist, no edema, 3+ pulses in all extremities, S1S2 heart sounds; A&O x4; Abd soft & non-tender, active BS in all quads, voiding w/o difficulty, urine clear and yellow; Skin integrity intact b. Diagnostic i. 12 lead ECG reveals ST elevation in leads II, III, AVF ii. Troponin T (norm 0-0.03): 1.2 ng/mL iii. CK/CK-MB (norm 0-10): 32 u/L c. Knowledge I know I I know I Patient Knowledge of Coronary Artery nothing know a good know Disease a amount a lot little Meds that help Coronary Artery Disease (CAD) Meds that hurt CAD Foods that should be avoided with CAD Your goal Blood Pressure Understanding Tx options Symptoms of CAD How CAD is measured and diagnosed Function of the heart Knowledge about why you have been sent to a cardiologist 2. Goals a. Prevent chest pain i. Nitro ii. Rest iii. Seek help if can not control iv. Reduce stress in life v. Proper use of O2 therapy when needed. b. Prevent complications: MI, thrombus i. Meds and lifestyle changes c. Increase or maintain daily activity i. DASH Diet ii. Loose weight iii. Identify techniques to enhance activity intolerance. iv. Pt will participate in desired activities and ADLs. v. Improve self-esteem. d. Properly use prescribed medication. i. Understand side effects, report any unusual side effects, or signs of allergic reaction. ii. Do not stop abruptly. iii. Monitor weight and BP. e. Gain knowledge about condition, risk factors, treatments, and potential outcomes. i. Stop smoking ii. Lower BP iii. Recognized worsening condition, call if you believe you are having a MI. iv. Pt will increase their perfusion and demonstrate behaviors to improve circulation. f. Maintain perfusion to the heart, prevent ischemic attacks. Increase cardiac output, decrease the heart’s demand for O2. i. Medications lowering lipids, lower BP, use prescribed blood thinners and anticoagulants. ii. Decrease the workload on the heart. g. Maintain normal lab values. i. CK-MB 0-3.9% ii. Mg 1.6-2.4 mEq/L, K 3.5- 5.2 mEq/L iii. Total cholesterol <200 mg/dL iv. HDL >= 35 or >= 60 mg/dL if high risk. v. LDL 65-180 mg/dL vi. Triglycerides <150 mg/dL vii. CRP 0- 1.0mg/L or less than 10mg/L viii. D dimer <= 250 ng/mL ix. Troponin <0.04 3. Outline a. Disease Process: Acute Coronary Syndrome is an emergency situation in which ischemia of the myocardium sets in causing acute chest pain. If ACS goes untreated it may eventually lead to a myocardial tissue death otherwise known as a heart attack. ACS is a spectrum syndrome that may range anywhere from angina (chest pain) to a full blown STEMI (heart attack with ST segment elevation noticed on an EKG). When blood flow through a coronary artery is slowed due to plaque build up, the heart muscle cannot obtain the amount of oxygen it needs to function. As cells are deprived of oxygen they begin to die off causing chest pain. This slowed rate of blood flow and lack of oxygen delivery is known as ischemia. This situation is Acute Coronary Syndrome. Should the artery become completely blocked and oxygen delivery no longer exists, a heart attack would occur. The complete blockage of the artery is known as an infarction which is why the technical term for a heart attack is a Myocardial Infarction. b. Medications i. Lisinopril 1. Dosage: initial dosage will be 10mg once daily then advance to 20-40mg once daily with a max dose of 80mg/day. 2. Frequency: daily 3. Instruction: take your blood pressure before taking medication, take at night before bed to avoid dizziness, change position slowly. 4. Reason for use: inhibits vasoconstriction to keep blood pressure down. ii. Atenolol 1. Dosage: Initial dose of 50mg/day orally then increased to 100mg/day. 2. Frequency: daily 3. Instruction: Take your BP and HR before taking drug, change position slowly, take at bed time. 4. Reason for use: blocks beta receptors to decrease blood pressure and heart rate. iii. Glyburide 1. Dosage: 2.5-5.0mg/day titrated down by no more than 2.5mg/week. 2. Frequency: daily 3. Instruction: take med at same time every day. If you miss a dose, take asap. Do NOT take if you cannot eat shortly after. 4. Reason for use: stimulates insulin release to lower blood sugar. iv. Prilosec 1. Dosage: 20mg/day 2. Frequency: daily for 4 weeks. 3. Instruction: notify physician of persistent abdominal pain. 4. Reason for use: decreases acid reflux by preventing the build up of acid in the stomach. v. Simvastatin 1. Dosage: initial dose of 40mg/day in the evening. 540mg/day. 2. Frequency: Daily in the evening. 3. Instruction: have liver enzymes monitored closely. 4. Reason for use: Lowers cholesterol including LDL and triglycerides. Also helps to raise HDL. Helps to prevent the progression of coronary atherosclerosis. c. Lifestyle changes necessary: remaining physically active (when angina presents rest and then continue ADL or activity when gone and gradually increase activity over time), smoking cessation, diet modification (hyperlipidemia, HTN, and DMII) ensure understands needs to choose low sodium, low fat, and understands carb exchange for diabetes. d. skills necessary for self-care: no mental deficits or sensory deficits noted in case study. patient can dress without assistance and may need assistance getting from bed to bathroom while on nitro. Patient understands medication effects and takes appropriate measures to not let adverse effects cause problems (like lightheadedness - giving time to equalize prior to standing) e. When to notify the provider: notify the provider if pain increases or persists with rest and medication, if any adverse medication effects are hindering quality of life (can re-evaluate regimen if needed), have emergency plan in place if cardiac arrest was to occur, if any signs of bleeding (unexplained bruising, persistent bloody nose, petechiae, uncontrolled bleeding) 4. Specify how you will teach your patient: a. Brochures b. Videos c. Whiteboard d. Demonstration e. Question and Answer f. Explanation g. Teach back using spinner 5. Determine how you will assess the patient’s learning: a. Level of patient learning will be demonstrated through using the teach back method with the spinner provided as well as the patients future admissions to the hospital, fewer future admissions indicates sufficient knowledge and compliance with treatment regimen.