Appendix `E` Rotation-specific goals and objectives of the program
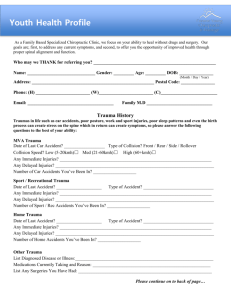
advertisement

Appendix E: Rotation-Specific Goals and Objectives of the Program PEDIAT RIC EMERGENCY MEDICINE GOALS & OBJECTIVES MEDICAL EXPERT: 1. Rapid recognition of the acutely ill or traumatized child, newborn or adolescent 2. Develop triage skills 3. Prioritize care of children in the ED 4. Appropriate and cost effective utilization of laboratory tests and various imaging techniques and their correct clinical interpretation 5. Develop expertise in common ED technical procedures and gain understanding of their indications, contraindications, and potential complications 6. Formulate and implement a short-term management plan for each child and effectively communicate this to the patient, family, medical and nursing staff 7. Supervise and delegate responsibility to junior trainees and other members of the health care team. 8. Develop competency in technical skills related to the specialty of pediatric emergency medicine. COMMUNICATOR: 1. Establish an appropriate physician/patient relationship with pediatric patients. 2. Communicate effectively with patients, families, and health-care consultants. 3. Use telephone communication effectively to assess and communicate with patients, health-care givers, other physicians and community agencies. 4. Demonstrate ability to deliver bad news with compassion and sensitivity. 5. Demonstrate ability to handle upset or abusive patients and/or caretakers. 6. Show an understanding of family dynamics, and factors that cause family dysfunction. 7. Demonstrate sensitivity to the cultural, ethnic and religious backgrounds of patients. 8. Develop techniques to effectively teach a variety of learners at different levels. 9. Be able to discuss relevant issues around interventions. COLLABORATOR: 1. Communicate and coordinate short and long term therapeutic decisions regarding patients presenting to the Emergency Department with the health care team. 2. Develop an understanding of the EMS system, effective telephone communication, and logistics of patient transfer to and from SickKids 3. Demonstrate ability to work effectively as part of a health care team. MANAGER: 1. Master the appropriate use of consultations and the patients’ disposition, education, and follow up 2. Demonstrate appropriate documentation of patient management and disposition. 3. Demonstrate ability to manage time efficiently. 4. Demonstrate ability to identify medico-legal risks and take steps to address them. 5. Master the ability to manage a busy Emergency Department with minimal staff intervention, with optimal prioritization and patient flow. 6. Follow up results of positive cultures or radiology reports with patient and family. HEALTH ADVOCATE: 1. Demonstrate an understanding of the determinants of health affecting patients and their families. 2. Demonstrate ability to act as an advocate for the individual patient and affected populations. 3. Demonstrate knowledge of the principles of health policy development. 4. Demonstrate knowledge of routine preventive health initiatives. 5. Demonstrate an understanding of the principles of identification and reporting of child abuse. 6. Demonstrate an awareness of legal, ethical, and professional obligations to protect children from suspicious circumstances. SCHOLAR: 1. Demonstrate ability to critically evaluate the literature as it pertains to pediatric emergency care. 2. Demonstrate inquisitiveness around clinical cases. 3. Demonstrate ability to apply the principles of evidence-based medicine. 4. Supervision and bedside teaching of junior trainees PROFESSIONAL: 1. Demonstrate 2. Demonstrate 3. Demonstrate 4. Demonstrate 5. Demonstrate 6. Demonstrate honesty and integrity. compassion and empathy. respect for others and diversity. reliability, responsibility and conscientiousness. an understanding of ethical practice and applies this to one's work. self-awareness/knowledge. O RTH O PEDICS GOALS & OBJECTIVES 1. 2. 3. 4. 5. 6. Develop history and physical exam skills required for the evaluation of musculoskeletal disorders. Learn use of the diagnostic imaging modalities available for the evaluation of orthopedic disorders. Develop skill in the evaluation and management of musculoskeletal trauma. Develop skill in the diagnosis and treatment of inflammatory and infectious disorders of the musculoskeletal system. Learn principles of acute and chronic pain management in patients with musculoskeletal disorders. Develop an understanding of referral and disposition practices. MEDICAL EXPERT: 1. Develop ability to correctly perform a history and physical in patients with musculoskeletal disorders. 2. Demonstrate ability to correctly order and interpret radiographs in patients with orthopedic injuries. 3. Demonstrate understanding of the anatomy, mechanism of injury, presentations, complications, management and prognosis of common musculoskeletal injuries. 4. Demonstrate knowledge of standard orthopedic nomenclature. 5. Demonstrate knowledge of appropriate aftercare and rehabilitation of orthopedic injuries. 6. Demonstrate knowledge of the differences in pediatric from adult skeletal anatomy and indicate how those differences are manifest in clinical and radiographic presentations. 7. Demonstrate ability to apply orthopedic devices, including compressive dressings, splints and brace immobilizers. 8. Demonstrate skill in performance of the following procedures: fracture/dislocation immobilization and reduction, classification and management of open fractures, arthrocentesis. 9. Demonstrate knowledge of joint injuries, evaluation and grading of joint injuries, treatment of joint injuries and prognosis. 10. Describe the presentations, complications, diagnosis and management of compartment syndromes. 11. Demonstrate ability to prioritize and manage the treatment of orthopedic injuries in multiple trauma patients. 12. Describe how to evaluate and preserve amputated limb parts. 13. Discuss evaluation and treatment of soft tissue injuries such as strains and crush injuries. 14. Demonstrate ability to recognize and treat soft tissue infections involving muscle, fascia, and tendons. 15. Discuss the dosages, indications, contraindications and side effects of standard analgesic and sedative agents used to treat patients with acute orthopedic trauma and demonstrate skills in their use. 16. List the indications for emergency surgery in the treatment of fractures and dislocations. 17. List indications for inpatient management of musculoskeletal disorders. COMMUNICATOR: 1. Be able to converse effectively and with sensitivity with orthopedics patients and their families. 2. Be able to discuss informed consent and other relevant issues around emergency room procedures. 3. Demonstrate knowledge of the health care consent act. 4. Demonstrate sensitivity to the backgrounds of patients. 5. Demonstrate ability to deliver bad news effectively with compassion and sensitivity. COLLABORATOR: 1. Communicate and coordinate with the health care team both short and long term therapeutic decisions regarding orthopedics patients. 2. Detail the proper and appropriate transfer of patients from one health care setting to another including listing of issues of patient transfer, transfer of medical documents and medical legal concerns. 3. Demonstrate ability to coordinate appropriate aftercare and rehabilitation of the orthopedics patient. 4. Demonstrate ability to work effectively as part of a health care team both in and around the outpatient and emergency room environments. MANAGER: 1. Coordinate care for patients, including the appropriate utilization of consultant specialists and community resources. 2. Demonstrate proper documentation involving management of medical patients. 3. Demonstrate ability to manage time efficiently. 4. Demonstrate ability to identify medico-legal risks and take steps to address them. HEALTH ADVOCATE: 1. Demonstrate an understanding of the determinants of health affecting patients and their families. 2. Demonstrate ability to act as an advocate for the individual patient and affected populations. 3. Demonstrate knowledge of health policy development. 4. Demonstrate knowledge of routine preventive health initiatives. SCHOLAR 1. Demonstrate ability to critically evaluate the literature as it pertains to orthopedics. 2. Demonstrate inquisitiveness around clinical cases. 3. Demonstrate ability to apply the principles of evidence-based medicine. PROFESSIONAL: 1. Adhere to the code of ethics of the Canadian Medical Association and the institution. 2. Treat patients and colleagues with respect. 3. Demonstrate ability to self-evaluate, including insight into strengths and weaknesses. 4. Demonstrate commitment to life-long learning. 5. Demonstrate willingness to accept responsibility for one’s actions and for patient care. OPERATIONAL CONSIDERATIONS The resident should contact Dr Narayanan a few weeks before the start of the rotation to discuss the goals and objectives. Responsibilities will include consultations to the Emergency Department, participation in orthopedic outpatient clinics (eg. fracture and follow-up clinics), casting details, and limited OR time emphasizing learning ED related skills. On call duties: First call to the ED for consultations during weekdays. 1 in 4 call for ED consults, including 2 weekend shifts per block EDUCATION & ROUNDS The resident will participate in teaching rounds on the service. We ask for residents to be excused for divisional teaching rounds on Thursdays from 10-4. EVALUATION ITER evaluations on POWER will be done by the responsible staff surgeons on the team in consult with senior trainees. The surgeons should also discuss the ITER with the resident. If a deficiency is identified, this should be brought to the residents’ attention as soon as possible. PLASTIC SURGERY GOALS: 1. 2. 3. 4. 8. 7. 7. 8. 9. 10. Understand the pathophysiology of wound healing. Learn effective wound evaluation and management skills. Learn wound closure techniques appropriate for outpatient, traumatic wounds. Learn appropriate methods for control of pain in patients with traumatic wounds. Learn appropriate follow-up techniques and management of the complications of traumatic wounds. Learn the evaluation and management of facial trauma. Learn the evaluation and management of hand trauma. Learn the evaluation and management of the burn patient. Learn the evaluation and management of the patient with cold injuries. Learn the evaluation and management of the patient with a chemical burn. OBJECTIVES: MEDICAL EXPERT 1. Demonstrate ability to perform appropriate history and physical exams in patients with traumatic wounds. 2. Demonstrate an understanding of wound pathophysiology, including cellular response, static and dynamic wound tensions, growth factors and tensile strength. 3. Demonstrate an understanding of the predictors of wound sepsis. 4. Demonstrate effective wound cleansing skills. 5. Describe the appropriate use, limitations and potential complications of wound cleansing solutions. 6. Describe the appropriate use, limitations and potential complications of antimicrobials in the management of traumatic wounds. 7. Demonstrate skill in various wound closure techniques including intradermal suture, facial closure, interrupted skin sutures, running skin sutures, vertical and horizontal mattress sutures, half-buried horizontal mattress sutures, tape closure, staples, and the use of glue. 8. Demonstrate appropriate use of delayed closure techniques. 9. Demonstrate appropriate management of special wound types, including skin ulcers, human bites, animal bites, snake bites, plantar puncture wounds, dermal abrasions and tar burns. 10. Demonstrate skill in the management of complex lacerations. List potential complications of complex lacerations. 11. Demonstrate ability to diagnose and treat soft tissue foreign bodies. 12. Discuss evaluation and treatment of soft tissue injuries such as penetrating soft tissue injuries. 13. Demonstrate skill in the provision of analgesia and anesthesia to patients with traumatic wounds including use of local infiltration, topical administration and conscious sedation. 14. Demonstrate ability to apply wound dressings. 15. Describe indications for specialty referral of traumatic wounds. 16. Demonstrate ability to evaluate and manage disorders of the mandible, including fractures, dislocations, and infections. 17. Demonstrate ability to evaluate and manage trauma to the head, neck, face and teeth. 18. Describe the following facial fractures and discuss their diagnosis and treatment: LeForte I, II and II, zygoma, mandible, nose, orbit and tripod fractures. 19. Identify the sensory distribution of the ulnar, median and radial nerve and demonstrate the technique of 2-point discrimination. 20. Describe the testing of the muscles and tendons of the wrist and hand. 21. Describe Boutonniere and Swan Neck deformities. 22. Give the signs of tenosynovitis and discuss the complications and treatment. 23. Identify the signs, complications and treatment of the following: paronychia, felon, herpetic felon/Whitlow, septic arthritis, deep palmar space abscess. 24. Discuss evaluation and treatment of soft tissue injuries such as strains, penetrating soft tissue injuries, crush injuries, and high pressure injection injuries. 25. Demonstrate the ability to perform a digital nerve block. 26. Demonstrate the correct care of the burn victim, including the ability to calculate surface area burned for various age groups. 27. Demonstrate the method for determining the correct maintenance fluid regimen for the burned patient. 28. State the admission criteria for the burned patient, including criteria for admission to the burn unit. 29. For the patient presenting with cold injury differentiate between frost nip and frost bite. 30. Outline the components of evaluation and treatment of patients with frostbite. 31. State the chemical mechanism of injury and the treatment for hydrochloric and sulfuric acids, hydrofluoric acid and alkali burns, and white phosphorus burns. 32. List the differences between alkali and acid burns. 33. State the common injuries/conditions associated with electrical injuries and list the potential complications. COMMUNICATOR 1. Be able to converse effectively and with sensitivity with plastic surgery patients and their families. 2. Demonstrate knowledge of the health care consent act. 3. Demonstrate sensitivity to the backgrounds of patients. 4. Demonstrate ability to deliver bad news effectively with compassion and sensitivity. COLLABORATOR 1. Communicate and coordinate with the health care team both short and long term therapeutic decisions regarding plastic surgery patients. 2. Detail the proper and appropriate transfer of patients from one health care setting to another including listing of issues of patient transfer, transfer of medical documents and medico-legal concerns. 3. Demonstrate ability to coordinate appropriate aftercare and rehabilitation of the plastic surgery patient. 4. Demonstrate an understanding of the roles of various participants in outpatient care. MANAGER 1. Coordinate care for patients, including the appropriate utilization of consultant specialists and community resources. 2. Demonstrate proper documentation involving management of medical patients. 3. Demonstrate ability to manage time efficiently. 4. Demonstrate ability to identify medico-legal risks and take steps to address them. HEALTH ADVOCATE 1. Demonstrate an understanding of the determinants of health affecting patients and their families. 2. Demonstrate ability to act as an advocate for the individual patient and affected populations. 3. Demonstrate knowledge of health policy development. 4. Demonstrate knowledge of routine preventive health initiatives. SCHOLAR 1. Demonstrate ability to critically evaluate the literature as it pertains to plastic surgery. 2. Demonstrate inquisitiveness around clinical cases. 3. Demonstrate ability to apply the principles of evidence-based medicine. PROFESSIONAL 1. Adhere to the code of ethics of the Canadian Medical Association and the institution. 2. Treat patients and colleagues with respect. 3. Demonstrate ability to self-evaluate, including insight into strengths and weaknesses. 4. Demonstrate commitment to life-long learning. 5. Demonstrate willingness to accept responsibility for one’s actions and for patient care. OPERATIONAL CONSIDERATIONS The resident should contact the service chief a week ahead to discuss the goals and objectives. The responsibilities will include consultations to the Emergency Department, participation in selected outpatient clinics and burn care, as well as limited OR time (laceration repairs). The resident will contact the chief Plastics resident (or scheduling coordinator) to be added to the call schedule and listed as “On call for ED Consults” with Locating. On call duties: First call to the ED for consultations during weekdays. 1 in 4 call until midnight for ED consults, including 2 weekend shifts per block We ask that the residents be excused for our divisional teaching rounds each Thursday from 10-4 pm. EDUCATION AND ROUNDS The resident will participate in teaching rounds on the service. EVALUATION This will be done by the responsible staff surgeons on the team. The surgeons should also discuss the ITER with the resident. If a deficiency is identified, this should be brought to the resident’s attention as soon as possible. PEDIATRIC INTENSIVE CARE GOALS 1. 2. 3. 4. 5. 6. 7. Develop the ability to rapidly recognize, evaluate, stabilize, and develop a differential diagnosis and disposition plan for critically ill children. Learn basic pediatric respiratory, cardiovascular, hepatic, renal, hematologic and neurologic physiology. Learn the indications for and complications of common invasive procedures performed in the ICU. Develop the knowledge and skills needed to perform diagnostic and therapeutic interventions in critically ill children. Develop an understanding of the importance of invasive physiologic monitoring (respiratory, hemodynamic, neurological) and how this is used to titrate therapies to desired physiologic endpoints. Learn the rational use of laboratory, radiographic and other diagnostic tests in the management of critically ill children. Learn the social, emotional, and physical implication of severe childhood illness on the family unit. OBJECTIVES MEDICAL EXPERT: 1. Demonstrate ability to rapidly perform history and physical examination in critically ill children. 2. Demonstrate ability to summarize and synthesize information in a concise and coherent format. 3. Demonstrate ability to assess children for the presence of severe illness and the appropriateness of ICU admission and preoperative screening. 4. Demonstrate ability to advise colleagues on pediatric resuscitation and critical care. 5. Demonstrate ability to perform the following procedures: endotracheal intubation, nasotracheal intubation, tube thoracostomy, central line placement, arterial line placement, and lumbar puncture. 6. Describe techniques of needle pericardiocentesis and surgical/needle cricothyroidotomy. 7. Demonstrate ability to use and interpret data from ECG monitors, 12 lead ECGs, cardiac and hemodynamic monitors, arterial blood gases, pulse oximetry, end tidal CO2 monitors, ventilators and ICP monitors in children. 8. Demonstrate ability to diagnose and treat shock, sepsis, fluid and electrolyte abnormalities, cardiac failure, cardiac dysrhythmias, renal failure, hepatic failure, status epilepticus, and toxicologic emergencies. 9. Demonstrate understanding of the etiologies, diagnosis, and treatment of respiratory distress syndrome and multisystem organ failure. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 20. 21. 22. 23. Demonstrate appropriate prioritization of diagnostic and therapeutic interventions in ill children. Demonstrate an understanding of appropriate resource utilization. Demonstrate appropriate judgment in the prioritization of ill patients and resource allocation for patients potentially requiring critical care. Demonstrate an understanding of the appropriate role of consultants in managing ill children. Order appropriate fluids, blood, blood products and blood substitutes necessary for the resuscitation of children. Describe the dosages, indications and contraindications of pharmacologic interventions for shock, cardiac failure, dysrhythmias, sepsis, trauma, toxins, respiratory failure, hepatic failure, renal failure, and neurological illnesses. Demonstrate ability to deal with complications of volume resuscitation and pharmacologic interventions. Select appropriate antibiotics for the pediatric patient with severe infection. Manage a patient on a ventilator including ventilator types, appropriate use of ventilation techniques, indications for extubation as well as weaning and extubation techniques. Demonstrate an understanding of CPAP and BiPAP modes of positive airway pressure. Demonstrate ability to rapidly assess and treat emergencies including but not limited to: dysrhythmias, cardiac arrest, pneumothorax, tension pneumothorax, dislodged endotracheal tubes, occluded endotracheal tubes, anaphylaxis, pulmonary embolism, hemorrhage, increased ICP. Develop an understanding of the multidisciplinary team in the management of the seriously ill child, including the roles of nursing staff, perfusionists, respiratory therapists, dietitians, occupational therapists, physiotherapists and consulting staff. Demonstrate ability to manage the airway of a sick child, including bag-valve mask ventilation, and indications and complications of definitive airway techniques. Demonstrate ability to deliver safe conscious sedation and deep sedation to children Demonstrate an understanding of the ethical and legal principles applicable to the care of critically ill children. Rotation Specific Skills: Endotracheal intubation: oral and nasal Cricothyroidotomy Adjunct airway management – LMA, BVM Ventilator management Thoracocentesis Tube thoracostomy Peripheral intravenous insertion Arterial line insertion Central venous line insertion Intraosseous infusions Sedation/analgesic management COMMUNICATOR: 1. Be able to converse effectively and with sensitivity with critically ill patients and their families. 2. Be able to discuss relevant issues around critical care procedures. 3. Demonstrate ability to deliver bad news effectively with compassion and sensitivity. COLLABORATOR: 1. Demonstrate the ability to appropriately advise physicians consulting the PICU. 2. Aid in arranging safe, appropriate and timely transportation of a critically ill patient, including determining the need for land or air transport or invasive procedures prior to transport. 3. Demonstrate an understanding of the appropriate use of consultants in critically ill patients. 4. Develop an understanding of the multidisciplinary team in the management of the ICU patient, including the roles of nursing staff, respiratory therapists, dietitians, occupational therapists, physiotherapists and consulting staff. MANAGER: 1. Demonstrate an appreciation for the administrative priorities of a critical care unit (eg. closed vs. open). 2. Demonstrate an understanding of appropriate resource utilization. 3. Demonstrate an understanding of the ethical and legal principles applicable to the care of critically ill patients. 4. Demonstrate ability to identify medico-legal risks and take steps to address them. HEALTH ADVOCATE: 1. Demonstrate ability to act as an advocate for the individual patient. 2. Demonstrate an understanding of "Do not resuscitate" orders, advance directives, living wills, competency, power of attorney and brain death criteria. 3. Demonstrate an understanding of when and how to withdraw care, and the process regarding organ donation and/or retrieval. SCHOLAR 1. Demonstrate ability to critically evaluate the literature as it pertains to critical care. PROFESSIONAL: 1. Demonstrate weaknesses ability to self-evaluate, including insight into strengths and OPERATIONAL CONSIDERATIONS The resident will function under the supervision of the ICU resident/staff. Responsibilities will include consults to the ED with initial stabilization and day to day ICU patient care. Overnight call is approximately 1 in 4 nights. EDUCATION & ROUNDS Will participate in teaching rounds on the service. EVALUATIONS Will be done by the responsible ICU staff physician. If a problem is identified, it should be brought to the resident’s attention as soon as possible. ANESTH ESIA GOALS 1. 2. 3. 4. To become competent in orotracheal and nasotracheal intubations Learn standard monitors and non-invasive monitoring techniques Develop familiarity with pharmacological agents used in anesthesia Learn relevant pre-operative historical and physical exam considerations including evaluation of airway difficulty 5. To become competent in recognizing the need for intubation as part of the emergency resuscitation process 6. To become familiar with the indications for use of the various oxygen delivery devices 7. To become knowledgeable about systemic sedation, and it’s potential complications OBJECTIVES MEDICAL EXPERT 1. Demonstrate knowledge of the anatomy of the upper airway. 2. Know the characteristics of a pediatric airway 3. List the indications for invasive airway management 4. Demonstrate appropriate judgment regarding the need for airway intervention 5. Recognize and manage an obstructed airway 6. Demonstrate correct use of the bag-valve-mask device, and nasal and oral airways 7. List the contraindications and complications of various airway management techniques including oral and nasal airway insertion, bag-valve-mask ventilation, nasal intubation, oral intubation, cricothyrotomy and tracheostomy 8. Demonstrate skill in nasotracheal and endotracheal intubation as well as management of complications 9. Demonstrate skill in the use of anesthetics and neuromuscular blocking agents including conscious sedation and rapid sequence intubation. 10. Demonstrate ability to insert a laryngeal mask airway 11. State the dosages, mechanism of action, indications, contraindications and potential complications of inhalation anesthetic agents, intravenous analgesic and anesthetic agents, induction agents and neuromuscular blocking agents 12. Demonstrate ability to use standard non invasive monitoring techniques including heart monitors, blood pressure monitors, oxygen saturation monitor, end tidal CO2 monitors 13. Demonstrate ability to manage a patient on a ventilator and discuss the advantage and disadvantages of different ventilation techniques 14. Coordinate the ongoing assessment and management of the intubated patient. 15. Demonstrate ability to administer local anesthetics and be familiar with agents, dosing, side effects, and techniques to monitor pain 16. Perform procedural sedation under faculty supervision and then independently. 17. Rotation Specific Skills: • Bag-valve-mask ventilation • Oral airway insertion • Nasal airway insertion • • • • • Nasal intubation Oral intubation (with rapid sequence induction) Intravenous insertion Management of monitors including: Oxygen saturation monitor end tidal CO2 monitor heart monitor blood pressure monitor arterial lines Ventilator utilization COMMUNICATOR 1. Be able to converse effectively and with sensitivity with seriously ill patients and their families. 2. Be able to discuss relevant issues around surgical procedures. 3. Demonstrate knowledge of the health care consent act. 4. Demonstrate sensitivity to the backgrounds of patients. COLLABORATOR 1. Demonstrate ability to work effectively as part of a health care team. 2. Demonstrate an understanding of the roles of various participants in the operative and critical care management of the patient. MANAGER 1. 2. 3. 4. Demonstrate Demonstrate Demonstrate Demonstrate ability to effectively and efficiently use anaesthesia resources. proper documentation around management of critically ill patients. ability to manage time efficiently. ability to identify medico-legal risks and take steps to address them. HEALTH ADVOCATE 1. Demonstrate an understanding of the determinants of health affecting patients and their families. 2. Demonstrate ability to act as an advocate for the individual patient and affected populations. 3. Demonstrate knowledge of health policy development. 4. Demonstrate an understanding of "Do not resuscitate" orders, advance directives, living wills, competency, power of attorney and brain death criteria. SCHOLAR 1. Demonstrate ability to critically evaluate the literature as it pertains to airway management and the practice of anesthesia. 2. Demonstrate inquisitiveness around clinical cases. 3. Demonstrate ability to apply the principles of evidence-based medicine. PROFESSIONAL 1. Adhere to the code of ethics of the CMA and the institution 2. 3. 4. 5. Treat patients and colleagues with respect. Demonstrate ability to self-evaluate, including insight into strengths and weaknesses Demonstrate commitment to life-long learning Demonstrate willingness to accept responsibility for one’s actions and for patient care. OPERATIONAL CONSIDERATIONS The resident will spend a large portion of time in the operating room doing the above procedures under staff instruction and supervision. Emphasis will be placed on managing fast-turnover cases (e.g. tonsillectomies, myringotomies) to ensure adequate technical experience. The resident will also participate in the anesthesia consults to the ED, not only in resuscitation cases but also in regional anesthesia and sedation cases. EDUCATION & ROUNDS The resident will participate in teaching rounds on the service EVALUATION Will be done by the staff and anesthetists and the ITER will be discussed. If a deficiency is identified, it should be brought to the resident’s attention early, so that remedial steps may be taken. TO XICO LO GY GOALS 1. Recognize likely intoxication in child/adolescent. 2. Develop competence in management of child with ingestion of unknown poison, specific ingestion, multiple ingestion and substance abuse, and accidental versus intentional poisoning. 3. Learn the need for various methods of termination of toxic exposure, hastening the elimination of poison and specific antidote therapy. 4. Recognize need for continued ED observation versus hospitalization versus ICU care. OBJECTIVES MEDICAL EXPERT: 1. Discuss the various forms of decontamination and their indications, including activated charcoal, whole bowel irrigation, gastric emptying, other extraordinary measures. 2. Discuss the management of the patient presenting with an unknown ingestion. 3. Discuss the management of specific ingestions, including acetaminophen, aspirin, tricyclic antidepressants, toxic alcohols, organophosphates, anticonvulsants, batteries, hydrocarbons, corrosives, lithium, digoxin, calcium channel blockers, antidiabetic medications, iron, sympathomimetics. 4. Describe specific toxidromes associated with various medications or toxins. 5. 6. Describe antidotes and other specific therapies available for various ingestions. Utilize poison information centres in an appropriate manner for consultation. COMMUNICATOR: 1. Discuss relevant issues around interventions with team. 2. Discuss patient care and communicate interventions with the consulting health care provider. 3. Act as first on-call for toxicology referrals from poison centre nurses. 4. Act as first on-call for in-hospital consultations to toxicology. COLLABORATOR: 1. Demonstrate ability to work effectively as part of a health care team both in and around the outpatient environment. 2. Demonstrate an understanding of the roles of various participants in the poison information centre. MANAGER: 1. Demonstrate proper documentation involving management of patients. 2. Demonstrate ability to identify medico-legal risks and take steps to address them. SCHOLAR 1. Demonstrate ability to critically evaluate the literature as it pertains to toxicology. 2. Actively participate in teaching seminars on common poisonings with toxicology staff. 3. Demonstrate inquisitiveness around clinical cases. 4. Demonstrate ability to apply the principles of evidence-based medicine. PROFESSIONAL: 1. Demonstrate weaknesses ability to self-evaluate, including insight into strengths and OPERATIONAL CONSIDERATIONS Regular seminars are arranged for trainees by Toxicology staff dealing with common poisoning situations and their management. The residents will be an integral part of this discussion. Furthermore, the residents will take first call for poison centre referrals by the poison centre nurses. Cases will be reviewed with the staff Toxicologist on call. Additionally the resident will be first call for any in-hospital (HSC) consultations on Friday afternoon. EDUCATION & ROUNDS The resident will participate in teaching rounds EVALUATIONS Will be done by the rotation supervisor, Dr. Margaret Thompson, with feedback provided by other staff toxicologists when available and the ITER will be discussed with the resident. If a deficiency is identified, it should be brought to the resident’s attention as soon as possible. PEDIATRIC TRAUMA GOALS 1. Learn basic principles of care of the pediatric trauma victim. 2. Develop an organized approach to the assessment, resuscitation, stabilization and provision of definitive care for the pediatric trauma victim. 3. Learn use of the diagnostic imaging modalities available for evaluation of the trauma victim. 4. Develop procedural skills needed in the evaluation and management of trauma patients. 5. Learn to recognize immediate life-threatening injuries and understand the crash protocol. 6. Learn to recognize limb threatening injuries and establish mechanisms to prevent loss. 7. Learn principles of burn management. 8. Develop an understanding of the recovery and rehabilitation phase of the seriously injured pediatric patient. 9. Learn to establish treatment priorities in complex patients under stressful conditions. OBJECTIVES MEDICAL EXPERT 1. Demonstrate ability to rapidly and thoroughly assess victims of major and minor trauma. 2. Demonstrate ability to recognize immediate life-threatening injuries and establish priorities in the initial management of victims of life-threatening trauma. 3. Demonstrate ability to manage the airway of pediatric trauma victims. 4. List different airway interventions and discuss the advantages, disadvantages and complications of each method. 5. Demonstrate ability to manage fluid resuscitation of trauma victims. 6. Discuss the definitive care of the trauma victim, including operative, post-operative and rehabilitative phases of care. 7. Demonstrate ability to perform the following procedures: oral and nasogastric intubation, venous cutdown, insertion of large bore peripheral and central venous lines, arterial lines, needle and tube thoracostomy, local wound exploration, peritoneal lavage, vessel ligation, repair of simple and complex lacerations, splinting of extremity fractures, and reduction and immobilization of joint dislocations, cricothyroidotomy, resuscitative thoracotomy, pericardiotomy and extensor tendon repair. 8. Demonstrate ability to interpret plain radiographs on trauma patients, including chest, cervical, thoracic and lumbar spine, pelvis and extremity films. 9. Demonstrate ability to use and interpret imaging modalities in the evaluation of trauma patients, including CT, angiogram, cystogram and urethrogram, and ultrasound. 10. Demonstrate the ability to assess and treat facial trauma. 11. Demonstrate the ability to evaluate and manage blunt neck injuries. 12. Demonstrate the ability to assess blunt chest trauma and develop treatment priorities in the stable and unstable patient. 13. List findings suggestive of traumatic aortic injury as well as defining the advantages, disadvantages and contraindications of angiography, echocardiography, transesophageal echocardiography, CT and MRI in the definition of the injury. 14. List the risks for and signs and symptoms of diaphragmatic injury. 15. Assess the abdomen of the blunt trauma patient including indications for immediate laparotomy. 16. Compare and contrast the use of diagnostic peritoneal lavage, ultrasound and CT scan for the evaluation of abdominal trauma. 17. Demonstrate proficiency in assessing retroperitoneal injuries including the indications for intravenous pyelogram and angiography. 18. Define the anatomy of the neck and classification of penetrating trauma by zone and define the diagnostic and therapeutic interventions required for each region. 19. Demonstrate ability to assess penetrating injuries to the chest and define indications for chest tube placement and open thoracotomy. 20. Compare and contrast types of injuries sustained in gunshot and stab wounds. 21. Describe management of penetrating injuries to the heart and major vessels. 22. Demonstrate ability to assess and treat the patient with penetrating abdominal trauma including indications for immediate laparotomy, CT scan and observation. 23. Define the management of penetrating trauma to the back and flank including indications and contraindications for wound exploration, radiographic imaging and surgical exploration. 24. Demonstrate ability to assess urologic injury in the trauma patient, including indications for IVP, CT, urethrogram and cystogram. 25. Demonstrate ability to calculate the Glasgow Coma Score and discuss its role in the evaluation and treatment of head injured patients. 26. Demonstrate ability to use spine immobilization techniques in trauma victims. 27. Assess a head CT for pathology. 28. Discuss the evaluation and management of spinal cord injuries. 29. Demonstrate the ability to diagnose and treat pelvic fractures. 30. Demonstrate ability to diagnose and manage tendon injuries. 31. Demonstrate ability to manage amputation injuries and discuss the potential for reimplantation. 32. Diagnose and manage extremity fractures, dislocations and subluxations. 33. Manage soft tissue injuries including lacerations, avulsions and high-pressure injection injuries. 34. Discuss the diagnosis and management of compartment syndromes. 35. Discuss factors unique to the evaluation and management of trauma in pregnancy. 36. Demonstrate the ability to manage the acutely burned patient, including minor and major injuries. 37. Demonstrate the ability to diagnose and treat smoke inhalation. 38. Demonstrate appropriate use of analgesics and sedatives in trauma patients. 39. Demonstrate appropriate use of antibiotics in trauma patients. 40. Discuss importance of mechanism of injury in the evaluation and treatment of the trauma victim. COMMUNICATOR: 1. Demonstrate the ability to effectively and sensitively communicate with seriously injured patients and their families. 2. Demonstrate the ability to communicate effectively with members of the trauma team. COLLABORATOR: 1. Learn to work within the team approach to trauma. 2. Discuss the role of pre-hospital systems in the management of trauma patients. 3. Demonstrate ability to direct a trauma team during complex resuscitations. 4. Demonstrate ability to coordinate multiple consultants involved in the care of trauma patients. 5. Demonstrate ability to arrange appropriate consultation and disposition of trauma patients. MANAGER: 1. Learn principles of disaster management. 2. Learn a systems approach to trauma management at the local and provincial levels. 3. Discuss principles of disaster management. HEALTH ADVOCATE: 1. Understand the determinants of health and risk factors for injury. 2. Understand the rationale and organization of local and national injury prevention initiatives. 3. Demonstrate the ability to counsel patients on injury prevention measures. SCHOLAR 1. Demonstrate the ability to critically appraise the literature on trauma issues. PROFESSIONAL: 1. Demonstrate weaknesses. ability to self-evaluate, including insight into strengths and OPERATIONAL CONSIDERATIONS The resident will function on the trauma team at St. Michael’s Hospital which is a Regional Trauma Referral Centre. He/she will function in a simulated “trauma team leader” role by the end of the rotation, under the supervision of senior surgical residents/residents/staff members. He/she will also carry out the above procedures under supervision. The OR time should be limited to relevant and instructive cases. EDUCATION & ROUNDS The resident will participate in teaching rounds on service EVALUATIONS Will be done by the staff surgeons and the ITER will be discussed with the resident. If a deficiency is identified, it should be brought to the resident’s attention as soon as possible. ADULT EMERGENCY MEDI CINE GOALS & OBJECTIVES MEDICAL EXPERT 1. Gain experience in management of common medical and surgical adult emergencies 2. Demonstrate compassionate and patient-centered care 3. Describe the relevant anatomy, pathophysiology, natural history, investigative modalities and management of acute disorders of body systems. 4. Interpret data obtained during the assessment of a patient so that justifiable conclusions are made. 5. Construct a differential for the presentation, itemizing the more common potential etiologies. 6. Develop a rational, relevant, practical and comprehensive management plan including the need for further diagnostic studies. 7. Demonstrate the skills of efficient assessment, management and decision making in an environment of large patient volumes and rapidly changing priorities. This includes the skill to do multiple tasks simultaneously and change focus appropriately. 8. Participate in major medical and surgical resuscitations, using delegation and supervision when appropriate. 9. Appropriately follow-up blood work, x-ray and EKG reports in patients. 10. List areas of high risk and management options to minimize these risks. 11. Recognise legal and ethical issues pertaining to the care of a patient, such as the assessment of mental competency, and outline the physician's role. 12. Show the ability to identify ethical issues in clinical practice 13. Show the ability to develop a coordinated and effective approach to the medical, social, psychological and legal aspects of human violence, including child, domestic and elder abuse. 14. Rotation specific objectives: a. intoxications, substance abuse b. common obstetrical complications & gynecological problems c. trauma d. acute psychiatric problems 15. Demonstrate proficient and appropriate use of examination and procedural skills, both diagnostic and therapeutic. a. Suturing b. Casting c. Fracture and joint reductions d. Slit lamp examination e. Pelvic examination Communicator 1. Communicate effectively with patients, health-care givers, physicians, and other health-care consultants. 2. Show ability to convey bad news to patients and their families in a flexible, understanding and balanced manner. 3. Use the telephone effectively to assess and communicate with patients, health-care givers, other physicians and community agencies. 4. Show an understanding of family dynamics, and factors that cause family dysfunction. Collaborator 1. Show willingness to receive and act on feedback from colleagues, other health care workers, patients and their families or care-givers. 2. Maintain a team environment that respects the skills of other health-care professionals and informal care-givers. 3. Show an understanding of team dynamics and the problems that may occur in an interdisciplinary team. 4. Recognize professional limitations and accept the need to use the skills of other consultants and health care practitioners to provide better care. 5. Identify other health care practitioners (including consultants) and available health care resources that can be used to plan the care of an older person. 6. Perform a competent consultation on referred patients to inform, educate and advise the referring physician and solve the problems while respecting the skills of the referring physician. Manager 1. Balance proper use of investigations and treatment for individual patients with a social obligation to control health care costs by avoiding redundant investigations and treatments. 2. Have a coordinated approach to the recognition, resuscitation and stabilization of patient problems presenting to the emergency department. 3. Develop leadership and consultant skills including the effective management of a health care team. 4. Develop appropriate documentation skills - both written and verbal. 5. Show appropriate record-keeping skills, including documentation of appropriate history and physical as well as pertinent negative and positive clinical findings. Health Advocate 1. When death seems inevitable, allow this to occur with dignity and comfort. 2. Recognize the determinants of health for individual patients, the emergency department population, and the general population. 3. Demonstrate the ability to act as an advocate for each patient to administrative, professional, and supporting bodies. Scholar 1. Incorporate validated research findings into clinical practice. 2. Refine and improve the knowledge skills and attitudes of prior training. 3. Have the skills needed to appraise medical texts, including critical evaluations of proposed treatments for medical conditions, and to conduct a bibliographic search independently. Professional 1. Show awareness of strengths and limitations. Make plans to deal with limitations, self evaluation and insight. 2. Protect information provided by or about patients, keeping it confidential, and divulge it only with the patient's permission except when otherwise required by law. 3. Practice in a fashion that is above reproach, and does not take physical, emotional or financial advantage of the patient. The resident will inform the patient and the supervising physician when personal morality or religious belief prevents the recommendation or performance of therapy. OPERATIONAL CONSIDERATIONS The resident will see patients under staff supervision at St. Michael’s Hospital (Emergency Department). EDUCATION AND ROUNDS The resident will participate on teaching rounds on service EVALUATIONS This will be filled out by various ED attendings and the ITER will be discussed with the resident. If a problem is identified, this should be discussed with the trainee as soon as possible. PREH O SPITAL CARE GOALS & OBJECTIVES MEDICAL EXPERT 1. Learn principals of pre hospital triage and emergency medical care delivery 2. Be competent to perform indirect (off-line) medical control and quality assurance. 3. Appropriately handle simulated pre-hospital care calls as a base hospital physician. COMMUNICATOR 1. Demonstrate ability to use all elements of the EMS communication system. COLLABORATOR 1. Learn the educational requirements and skill levels of various EMS providers. 2. Participate as an observer or team member in ground and air medical transport systems. 3. List the roles and responsibilities of the base hospital physician and medical director in the EMS system. 4. Discuss the differences in education and skill level of various EMS providers. Describe the competencies/skills of the BLS provider. List the added skills of the land paramedic, flight paramedic, and state which skills are delegated medical acts. 5. List the drugs carried by the land and flight paramedics. List those drugs which the flight paramedics may administer in addition to those which they carry. MANAGER 1. Learn common organizational structures of emergency medical services. 2. Learn principles of EMS system operations. 3. Learn basic principles of disaster management. 4. Learn medicolegal principles relating to EMS 5. Describe the EMS system in Metro Toronto. 6. Actively participate in the Metro EMS program. 7. Actively participate in EMS system management. 8. Describe the provincial and national legislation and standards for EMS systems. 9. Discuss medicolegal liability issues relating to EMS. 10. Participate in EMS continuous quality improvement including tape and chart review. 11. Discuss development of EMS pre hospital care protocols. 12. List the standing orders in both the land and air programmes. 13. Discuss basic concepts of disaster management. 14. Discuss the role of dispatch in the system. 15. Demonstrate understanding of appropriate utilization practices for ground and air medical services. 16. Discuss the process of disaster notification, response, and medical care on a local, provincial and national level. 17. Discuss the importance of and methods for medical control in EMS systems. HEALTH ADVOCATE 1. Demonstrate an understanding of the determinants of health affecting patients and their families. 2. Demonstrate ability to act as an advocate for the individual patient and affected populations. 3. Describe common environmental, toxicologic, and biological hazards encountered in the pre hospital care setting as well as injury prevention techniques. SCHOLAR 1. Demonstrate ability to critically evaluate the literature as it pertains to airway management and anaesthesia. 2. Demonstrate inquisitiveness around clinical cases. 3. Demonstrate ability to apply the principles of evidence-based medicine. 4. Learn basic principles of EMS research. 5. Demonstrate ability to provide initial and continuing education to all levels of EMS personnel 6. Demonstrate familiarity with research methodologies relating to EMS and disaster management. PROFESSIONAL 1. Adhere to the code of ethics of the CMA and the institution 2. Treat patients and colleagues with respect. 3. Demonstrate ability to self-evaluate, including insight into strengths and weaknesses 4. Demonstrate commitment to life-long learning OPERATIONAL CONSIDERATIONS See EMS binder for rotation information. EDUCATION AND ROUNDS The resident will participate on teaching rounds on service EVALUATIONS Feedback will be sought and the ITER will be completed by Dr Lalani ADDENDUM All Residents must complete: ATLS and APLS. course per year. Funding will be provided for one All Residents should meet with the various subspecialty rotation supervisors prior to the start of the rotation. Specific goals and objectives should be discussed and presented in writing on that occasion. This will maximize the opportunity for the various departments to ascertain that these goals are met. This should be followed by another meeting 7-10 days into the rotation to review progress and to remedy any deficiencies. All Residents should keep a log of procedures performed, along with a date and the supervisor's name. This is important not only for documentation that the various learning objectives have been met, but also for the RCPSC and ABP PEM Certification Exams. Attendance at the various national and international meetings within the PEM section is strongly encouraged. EVALUATIO N 1. In-training evaluation reports (ITERs) will be filled out on POWER each month by the designated mentor. Observed history and examination skills (mini CEX) MUST be completed once per month during first year, in order to pass the residentship. 2. Each resident will meet with the program director at least every 6 months discussion will include PEM and off-service rotations, research progress, teaching activities, professional conduct, and other academic activities. Individual learning objectives and career planning will also be discussed. Individuals interested in a third year will have the opportunity to discuss funding options. 3. Examinations: o o OSCE examination (2 hours) every 6 months MCQ and SAQ exam (1 hour) every 6 months 4. SITE Exam: American Board of Pediatrics in-training written examination (3 hours) every year for those interested in doing a third year and qualifying for the ABP PEM exam.