Case Study #1: Tommy
advertisement
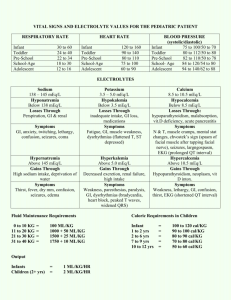
Running head: CASE STUDY #1: TOMMY 1 Case Study #1: Tommy Marissa Hampton and Gabriela Olivas University of Texas Medical Branch at Galveston School of Nursing NNP 1 GNRS 5631 Leigh Ann Cates MSN, RN, NNP-BC, RRT-NPS & Dr. Debra Armentrout January 30, 2014 CASE STUDY #1: TOMMY 2 Case Study #1: Tommy DOL #1: Baby Tommy, a 4000 gm, 39 2/7 week LGA male, was admitted last night. Mom is a 28 year old, G3 P2 married white female with a history of NIDDM diet controlled. Spontaneous rupture of membranes (SROM) occurred ~ 10 hours prior to delivery with clear fluid. Over the last 2 hours of labor the FHR monitor has displayed late decels and fetal bradycardia. It was decided to deliver by emergent C-section for continued fetal distress. Tommy required vigorous resuscitation in the delivery room, including chest compressions and 2 rounds of placed. At 2 hours of age he had a possible seizure, so he was placed on Phenobarbital (loading) dose of 20 mg/kg IV. This AM, he is stable on vent settings of: FiO2 35%, IMV 30, PIP 26, PEEP 5, IT 0.3 with stable ABGs. Cardiovascular status is stable, and he has both a UAC/UVC and OG tube in place. He is under a radiant warmer. Urine output (UOP) for the past 8 hours since admission = 12 ml and total IVF intake = 26 ml (D10W @ 65 ml/kg/day). He has not stooled. AM labs: Hct 26; Na 130, K 4.5, Cl 114, C02 18, BUN 7, Cr 0.9, Glucose 70, Ca 8.0, Bili T/D 5.8/0.7. 1. What factors do you need to consider when planning your fluid management for the next 24 hours? “Initial Fluid restriction is recommended as HIE infants are predisposed to a fluid overload state from renal failure secondary to acute tubular necrosis(ATN) and syndrome of inappropriate antidiuretic hormone (SIADH) (Gomella, Cunningham & Eyal, 2013).” For the next 24 hours, we will continue to fluid restrict the infant at 65 ml/kg/day. Blood products: Our first lab result indicated a hematocrit level of 26 mg/dL, therefore a transfusion of packed red blood cells (PRBCs) is needed in order to maintain the hematocrit levels and the oxygen carrying capacity for the infant. To replenish our hematocrit, to a goal of 30-35 %, we will need to transfuse 10 mL/kg over 3 hours, therefore, a total of 40 mL of PRBCs over 3 hours (Gomella et al, 2013). During blood transfusion, infant will need to take nothing by mouth (NPO). Intravenous fluid: The infant has an umbilical artery catheter (UAC) and will require ½ Normal saline +0.25 units of Heparin/ml to run at 0.5 ml/hour, for a total of 12 mL/day in first 24 hours. This provides ~ 3 ml/kg/day of fluid Parenteral Nutrition: The infant has a double lumen umbilical venous catheter and will require two separate drips. The primary lumen will be our nutrition line and infuse TPN D10 + 2%AA + 0.25 units of heparin/ml, to run at 10 mL/hr. This provides ~ 50ml/kg/d. Our second lumen of our UVC will be a carrier fluid and infuse Normal Saline + 0.25 units of Heparin/ml at a keep open rate of 0.5 ml/hr. Total fluid volume for 24 hours would be 12 ml/day, estimated at 3 ml/kg/day. “Heparin should be added to parenteral nutrition (0.5-1 unit.mL) to maintain catheter patency (Gomella et al., 2013)”. Enteral Nutrition: The infant will be NPO for the first 24 hours. Enteral feeds will not contribute to the total fluid volume. After the first 24 hours, electrolytes can be added to balance and reflect laboratory deficits. “Daily sodium requirements is 2-4 mEq/kg/day per monitoring of serum (target values, 135- 140 mEq/L) (Gomella et al, 2013).” Increased levels of Acetate may also be titrated into UAC fluids to correct CO2 deficits. CASE STUDY #1: TOMMY 2. 3 Within the next 24 hours, if urine output stabilizes, we may consider changing clear fluids to total parenteral nutrition (TPN) and increasing GIR to promote growth and maintain serum glucose values > 60 mg/dL (Gomella et al, 2013). Our goal would be to increase our GIR by 1-2 a day. Once urine output is established, the total fluid volume of 60 ml/kg/day may increase by 10-20 ml/kg/day to keep hydrated, per infants needs(Gomella et al, 2013). Begin antibiotics until 48 hour blood culture results are final: o Ampicillin 50 mg/kg/day IV q 8 hours (Lexicom, 2013) o Gentamicin 4.5 mg/kg/day IV q 36 hours (Lexicom, 2013) Identify any labs that concern you, rationale for your concern, and your plan to correct these. A hematocrit level of 26 is concerning. Acceptable hematocrit levels are dependent upon the infants medical status and usually range between 35-40% (Gomella et al, 2013). A low hematocrit level may be indicative of hemorrhage. “Increased or decreased of central hematocrit from accepted normal values suggest changes in intravascular volume as it related to total body weight (Gomella et al, 2013). ” In order to continue to oxygenate and perfuse well, the infant is in need of a blood transfusion. The infant needs to be type and screened and blood should be matched to prevent a blood transfusion reaction. The infant should receive 10 ml/ kg over 2- 4 hours, and should remain NPO for the duration of the transfusion. A sodium level of 130 mEq/L is indicative of hyponatremia. Hyponatremia occurs at serum levels less than 135 mEq/L. Hyponatriemia may be due to increased extracellular water, third spacing or an increased serum loss (Gomella et al, 2013).Without excessive water loss, SIADH occurs commonly with birth asphyxia, therefor causing dilutional hyponatremia (Gomella et al, 2013). Hyponatremia can be corrected by adding electrolytes into our IVF then increasing gradually as compared to serum levels. “Daily sodium requirements is 2-4 mEq/kg/day per monitoring of serum (target values, 135140 mEq/L) (Gomella et al, 2013).” On DOL 2, sodium should be added to our IVF beginning with 1-2 mEq/ 100ml of fluid. A low serum CO2 is indicative of academia. Acidosis may be present from perinatal asphyxia during birth. The low CO2 levels are corrected by adding acetate to our UAC fluid. Likewise, we must add acetate with sodium, both for sodium replacement and correction of acidosis. A serum calcium level of 8.0 is cautionary. Lower levels of calcium indicate hypocalcemia and can lead to tetany, jitteriness, prolonged QT interval and seizures (Powerpoint, 2013). Low calcium levels may be related to perinatal asphysxia initially from delivery due to fetal bradycardia and late decelerations. Additionally, vigorous resuscitation in delivery room may cause subcutaneous fat necrosis. Technically, a serum level less than 7.0 serum is considered hypocalcemina. In this case monitoring serum calcium levels is appropriate. T Bili- Hyperbilirubinemia- “High indirect serum bilirubin levels during the first 24 hours of life are never physiologic (Gomella et al, 2013).” The total bilirubin count includes direct and indirect bilirubin. Likely causes of an elevated level within this time frame include sepsis, occult hemorrhage or hepatic insult. These possibilities are likely given our lower hematocrit level, maternal rupture of membranes for 10 hours, and perinatal asphyxia. The infants jaundice risk level should be plotted according to age in hours against serum bilirubin level, in order to determine if phototherapy is necessary. To rule out sepsis, mother’s complete labs should be obtained along with the infant’s baseline blood work of complete blood count (CBC) and blood culture. CASE STUDY #1: TOMMY 4 D bili-“ Conjugated hyperbilirubinemia is never normal or physiologic. Conjugated hyperbilirubinemia in the first 24 hours of life is abnormal and can indicate and infection (Gomella et al, 2013).”pg 393. “In infants with conjugated bilirubin levels > 0.5 mg/dL and <2 mg/dL, an infection must be ruled out (Gomella et al, 2013)”. The elevated direct bilirubin level is concerning due to the mothers rupture of membranes of about 10 hours. In order to rule out infection, the infant needs to have a baseline complete blood count (CBC) and blood culture before considering prophylactic antibiotics. Maternal labs should be obtained. If infection is ruled out, perinatal hypoxia may be the contributing factor, causing hepatic insult (Gomella et al, 2013), and therefore rising direct bilirubin levels. 3. When and what do you want for your next labs? Initially we would have ordered: CBC with differential, blood culture, serum electolytes, BUN/Cr, cardiac enzymes, liver enzymes, a coagulation panel, and a baseline blood gas, bedside glucose. After stabilization, with concern for our initial labs, we would order: o Electrolytes level in 6-8 hours. o Glucose checks every 6 hours o Follow up blood gases with time to be determined according to blood gas reading. o AM Basic metabolic panel- to include liver enzymes, T/D Bili, Electrolytes, and BUN/Creatinine levels in the morning (AM). o CBC with differential in AM o Phenobarbital levels after ____ dose o Gentamicin trough with 3rd dose, if continued beyond 48 hours At 24 hours of age, Tommy remains on the vent with no changes except for fluctuating O2 requirements (range: 35%-50%). Wt. 4100gm. VS: HR 160, RR 40, T 98.4, BP 40/26, mean ~ 32. Total UOP = 20 ml since admission. IVF intake = 60 ml/kg/day. AM labs: Na 127, K 4.2, Cl 110, C02 18, BUN 10, Cr 0.5, Gluc 100, Ca 8.2, Bili T/D 6.2/0.8. 4. In a few sentences discuss the pathophysiology for the abnormal labs. Dilutional hyponatremia due to decreased sodium level of 127 mEq/dL, increased weight gain of 100 grams in first 24 hours of life and increased oxygen requirements. Dilutional hyponatremia occurs with extracellular fluid, where there is a positive water balance (Gomella et al, 2013). “”ECF is very increased, resulting in edema and weight gain (Gomella et al, 2013). Causes may include renal and hepatic failure. Hyperbilirubinemia as related to increasing total bilirubin level. The infant’s red blood cells have rapidly lysed and turned over according to the lower hematocrit level. A “decreased central hematocrit from accepted normal values suggest changes in intravascular volume as it related to total body weight (Gomella et al, 2013). ” Secondly, the infant experienced a difficult delivery. Bruising and hepatic injury may be possibile. The by product of red blood cell destruction is unconjugated bilirubin, which is metabolized by the liver, to a form, conjugated bilirubin that can then be excreted by the body. Although term gestation, the infants liver is still relatively immature and therefore inefficient with metabloism. Hyperbilirubinemia in the newborn ”is caused by an increase in enterohepatic circulation, a decrease in clearance of bilirubin or an increase in production (Gomella et al, 2013).” An increase in direct bilirubin level is considered abnormal within the first 24 hours of age (Gomella et al, 2013). Increased levels of conjugated bilirubin (direct bilirubin) may also be due enterohepatic circulation. CASE STUDY #1: TOMMY 5 Hypotension due to lower than average mean blood pressures for gestational age. For term infants, mean blood pressure ranges should be at least near or at gestational age, up to 30 points higher (Gomella et al, 2013). Hypotension is evident in myocardial dysfunction as related to perinatal asphyxia (Gomella et al, 2013). 5. What will you do to correct these labs, if anything? In efforts to stimulate the kidneys, give one Normal saline bolus of 10ml/kg over 1 hour. “A fluid challenge can be given in an infant without evidence of heart failure… An increase in urine output greater than 1 ml/kg/hr indicates prerenal failure. No response indicated intrinsic renal failure (Gomella et al, 2013).” Additionally, infants with acute renal failure my present with dilutional hyponatremia (Gomella et al, 2013). Consider IV Lasix bolus of 1mg/kg/dose x 1 to correct fluid overload. However, “Furosemide-induced diuresis results in enhanced excretion of sodium, chloride, potassium, calcium… bicarbonate and possibly phosphate (Gomella et al, 2013).” As Lasix would be desired to prohibit edema, further loss of sodium may be detrimental to the patient by worsening hyponatriemia and inducing seizure activity. Continue to monitor serum calcium levels throughout the next few days. We anticipate a drop in calcium levels after the first 24 hours of life, but will continue to monitor as long as patient is asymptomatic and serum calcium is not less than 6.5 mEq/ dL. Begin phototherapy for TBili of 6.2 at 24 hours of life. The use of phototherapy lights helps transformed unconjugated bilirubin into bilirubin “photoproducts” which allows for excretion (Gomella et al, 2013). With phototherapy we will maximize the infants skin exposure, ensure the irradiance level is above 30 and have the infant wear protective eye shields. Begin low dose dopamine at 5 mcg/kg/min to initially stimulate renal perfusion. May titrate drip according to mean blood pressures in attempt to also avoid hypotension. 6. What are your differential diagnoses at this point? Term LGA 39 2/7 week male, DOL # 2 Perinatal Asphyxia Respiratory distress Dilutional hyponatremia Hyperbilirubinemia Suspected Hepatic injury Suspected Renal failure Hypotension Suspected sepsis 7. What further labs or diagnostic studies would you like to order to confirm your diagnoses? Chest x ray Renal ultrasound Liver ultrasound Electroencephalogram (EEG) Head ultrasound Magnetic resonance imaging (MRI) 8. Outline your management plan for Tommy, with rationales Routine chest x ray to assess infants lung fields and increasing Fio2 needs. Chest x ray will help identify respiratory distress, ETT position, worsening respiratory status. CASE STUDY #1: TOMMY Routine renal ultrasound with Doppler to determine kidney function, structure, congenital anomalies and presence of obstruction/malformation, such as a thrombus is evident (Gomella et al, 2013). Routine head ultrasound to assess for intravascular hemorrhage (IVH) due to drop in hematocrit level to 26 and perinatal asphyxia event. MRI in AM. Infants with perinatal asphyxia are at risk for neurodevelopment dysfunction. The MRI may be ”more accurate at demarcating areas of brain injury due to the presence of cerebral edema in the first 48-72 hours (Gomella et al, 2013.” EEG today. Fluid restrict to keep at 65 ml/kg/day. Infant’s renal function is not adequate due to low urine output and weight gain within the first 24 hours. Restricting the infant’s fluid intake will prevent overhydration, electrolyte imbalances and stress to multiple organs. “The avoidance of volume overload helps avert cerebral edema (Gomella et al, 2013).” Continue current UAC/ UVC fluids. Will consider altering electrolyte levels if no improvement with urine output Strict intake and output to monitor intake of fluid and urine output. Keep NPO due to infants current critical status, fluctuating respiratory needs and poor renal function. Oral gastric tube to gravity. Start low dose dopamine at 5 mcg/kg/min to stimulate renal perfusion, may titrate to keep mean blood pressure to 40-50. Low dose dopamine produces renal vasodilation, while moderate dose dopamine has a positive inotropic effect on the myocardium (Gomella et al, 2013). Either dosing administration will be beneficial to the patient. Insert urinary catheter to assess urine volume. With low urine output and adequate hydration, it is important to rule out obstruction. Placing a urinary catheter with positive urine return will allow for approximate urine collection and while ruling out obstruction. Collect and send urinalysis, urine sodium, urine osmolality, urine- specific gravity (Gomella et al, 2013). Collection of these labs will help determine the cause of renal insult and differentiate between syndrome of inappropriate antidiuretic hormone, prerenal or intrinsic renal disease. In am collect: o CBC: Continue to monitor for sepsis due to mothers ROM of 10 hours. o LFTs: Continue to monitor hyperbilirubinemia and to determine if single bank phototherapy is suffient o BUN/Cr: Continue to monitor renal function to determine if worsen organ damage. Continue with scheduled blood gases to manage respiratory status If blood sugar remains stable(>60 mg/dL) then change glucose checks to every 12 hours. Continue to follow blood culture growth. This will be the determining factor in continuing antibiotics. On DOL #4 Tommy remains on the vent: IMV 35, PIP 24, PEEP 5, FiO2 60%, IT 0.3. PE reveals palpable kidneys, blood tinged urine and CXR 9-ribs expansion. UOP was <1.0 ml/kg/hr for the past 24 hours. Wt = 4500 gm. VS: HR 170, RR 40, T 98.6, BP mean 36. AM labs: Hct 35, Plts 45, Na 147, K 6.7, Cl 100, CO2 16, BUN 40, Cr 2.2, Gluc 120, Ca 9.6, T/D Bili 5.9/1.0. 9. 6 What are your differential diagnoses for Tommy today? CASE STUDY #1: TOMMY 7 Former 39 2/7 week male, DOL #5 HIE Respiratory distress Hyperkalemia Syndrome of Inappropriate Antidiuretic hormone Suspected acute tubular necrosis Thrombocytopenia Hepatic injury Suspected renal vein or artery thrombosis 10. What factors do you need to consider when planning today’s fluid management? Infant still has urine output less than 1 ml/kg/hr, signs of edema and palpable kidneys which indicate intrinsic renal failure. Infant should remain on strict I&Os and fluid restriction Weigh infant every 12 hours. Continue low dose dopamine of 5 mcg/kg/min to increase renal perfusion. Fluid restrict infant to 80 ml/kg/day. Fluid advancement has been slow due to poor urine output and edema, infant needs to be fluid restricted while “only replacing insensible losses plus urine output (Gomella et al, 2103).” May increase UAC fluids to full acetate + heparin infusion, due to continued low metabolic CO2 level. Plan for platelet transfusion today Due to the suspected acute renal failure we would reduce protein in fluids (Armentrout, 2010). Additionally, we would restrict potassium intake(Gomella et al, 2013) 11. Write your fluid orders for today, with rationales. Keep total fluid volume at 80 ml/kg/day Blood products: Transfuse 10 mL/kg of platelets, leukocyte-reduced, irradiated over 2 hours. Therefore, total infusion of 40 ml over 2 hours. Increased platelet destruction resulting in thrombocytopenia may directly be related to birth asphyxia (Gomella et al, 2013). Treatment is aimed at increasing levels. “The platelet count should increase to >100,000/uL. Platelet count should be repeated within one hour (Gomella et al, 2013)”. Total fluid volume is 10 ml/kg/day. Intravenous fluids: Infuse UAC fluids of 7.7sodium acetate +0.25 units of heparin/ ml at 0.5 ml/hr. A change to full acetate fluid is necessary to promote CO2 retention, in order to prevent metabolic acidosis. Total fluid intake is about 2.6 ml/kg/day Parenteral Nutrition: In our first lumen UVC: Infuse TPN D15 +3% AA +0.25 units of heparin/ml to run at 11.25 ml/hour. Intralipids @ 2 g/kg/day will run at .83 ml/hr. Our initial GIR on DOL1 was 4.5. Now on DOL4, we would want to steadly increase of GIR to provide enough nutrition and glucose to keep our infant euglycemic. Due to our volume restriction and need for platelet transfusion, our total fluid allotted for TPN is roughly 60 ml/kg/day. In order to both increase our GIR appropriately (by 1 mg/kg/day) and to volume restrict, the dextrose concentration should be increased to 15 percent( Armentrout article, 2012). 15 percent dextrose yields 26 kcal/kg/day. A lower percentage of protein is used to preserve kidney function, specifically prevent tubular damage. 2% AA yields 4.8 kcal/kg/day. Intralipid infusion yields roughly 3 ml/kg/day and 18 kcal/kg/day. Our second lumen will infuse ¼ Ns + 0.25 units of heparin/100 ml to run at 0.5 ml/hr. ¼ NS is being utilized due to increasing sodium levels of up to 147 mg/dL. ¼ NS provides less sodium than other saline infusions. The increasing sodium level predisposes our infant to lethargy, irritability, apnea, seizures and coma (Powerpoint,2013) CASE STUDY #1: TOMMY 8 Enteral nutrition: Keep infant NPO due to worsening respiratory and renal status. 12. Identify any labs that concern you, the rationale for your concern, and your plan to correct these. A platelet level of 45 indicates thrombocytopenia. Causes on thrombocytopenia may occur from intrauterine hypoxia, sepsis, thrombosis related to central catheter placement, maternal diabetes or acidosis (Gomella et al, 2013). Given maternal history, the infant was predisposed to all of these factors. Untreated thrombocytopnenia may cause excessive bleeding, progressing to disseminated intravascular coagulation (DIC). Transfusion of platelets of 10 ml/kg over 2 hours is appropriate. Increasing serum sodium levels may predispose the infant to irritability, apnea and seizure activity (powerpoint, 2013). Increased extracellular fluid with hypernatremia may be a result of adequate fluid intake with dysfunctioning kidneys due to hypoxic injury. Treatment of hypernatriemia with increased extracellular fluid involved maintaining fluid intake, while restricting sodium until serum levels are within normal limits(Gomella et al, 2013). Hyperkalemia becomes symptomatic once potassium levels reach 7-8 mEq/L. “Cardiac conduction is the most immediate concern and electrocardiographic monitoring is essential until treatment corrects serum levels (Gomella et al, 2013).”Frequent causes of hyperkalemia include renal failure and blood transfusions. Currently potassium will be with held from TPN administration. Consistentlt lower CO2 level still indicates a level of metabolic acidosis. In efforts to correct, the UAC fluid was advanced to full acetate as replacement therapy. BUN and creatinine levels over 20mg/ dL and .6-1 mg/dL indicate renal insufficiency and or renal disease (Gomella et al, 2013). All nephrotoxic medication should be adjusted. Low dose dopamine may be started to increase renal perfusion along with diuretic therapy. Fluid restriction is necessary. Although the total bilirubin level is decreasing, the direct bilirubin level has remained elevated. An elevated direct bilirubin may suggest hepatic injury from prenatal asphyxia. Cholestatsis must also be ruled out. Single bank phototherapy was initiated in efforts to decrease circulation bilirubin. Tommy is now DOL #8. Weight is 3800gm. He is stable in an open crib, on NC@1 LPM, FiO2 50%. He is currently on D10W with 3 gm/kg of protein, 3 gm/kg of Intralipids Na 2 mEq/kg, K 2 mEq/kg and Ca 2mg/kg at 120 cc/kg/day. PE: alert, responsive, no murmur, lungs clear, abdomen soft with + BS, passing guiac – stools. UOP = 7 ml/kg/hr. AM Labs: Hct 34, retic 5.2, Na 133, K 4.2, Cl 99, CO2 16, BUN 7, Cr 0.5, Ca 8.2, Gluc 85, Bili T/D 2.5/0.5. The plan today is to initiate enteral feeds. 13. Write your fluid management plan and rationale. Enternal Nutrition: Begin enteral feeds of Enfamil 20 cal with Iron at 20 ml/kg//day (9.5 ml q 3 hours). Parenteral Nutrition: Infuse Intralipids 3gm/kg/day(15cc/kg/day) at ml/hr; TPN D11.5 W (105 cc/ml/day) with 3.5 gm/kg, Na Acetate 3 mEq/kg, K Chloride 2 mEq/kg, Ca 2 mEq/kg to infuse at 16.6 ml/hr. CASE STUDY #1: TOMMY 9 We need to put iv rate for IL… and did we mean to put dextrose at 11.5? just bc it says d 10 above.. can we change it? Due to the infants age in days, we can assume that our UAC line as well as fluids have been discontinued. The Centers for Disease Control and Prevention (CDC) recommend that UACs remain in use for no more than 5 days (Gomella et al, 2013, pg.241). CDC currently recommends the use of UVCs to be limited to 14 days (Utomo, 2012). What type of central line access must be taken into account when writing our fluid management plans because of carrier fluids accounting for total fluid intake. Start enteral feeds of Enfamil 20 cal with Iron at 20 ml/kg/day (9.5 ml q 3 hours). for a total caloric intake of 13.3 kCal/kg/day of feeds. Currently, Tommy total fluid intake is 120 cc/kg/day. By DOL 8, this implies he was fluid restricted; he also has the increased urine output of 7ml/kg/hr. We could increase his total fluids to 140cc/kg/day. His parenteral fluids could remain the same 105 cc/kg/day, but we are just adding the extra 20 ml/kg/day of feeds. This way the sodium mEq will be greater in the same solution and assist with increasing the patient’s sodium and decreasing urine output from 7 ml/kg/hour. Tommy’s intralipids are at 3gm/kg/day provide, which provide Tommy with 27 kCal/kg/day of lipids. His protein can be increased to 3.5 gm/kg/day,which provides Tommy with 14 kCal/kg/day of protein. The dextrose caloric intake from the TPN D11.5W is 41.8 kCal/kg/day of dextrose. We want to increase our GIR by approximately 1 mg/kg.min. Infusion rates can be increased by 0.5-1 mg/kg/min each day (Gomella et al, pg.124). The GIR from the previous fluids was 7.3 mg/kg/min. With our TPN D11.5 W, our new GIR is 8.4mg/kg/min. 14. Identify any labs that concern you, the rationale for your concern, and your plan to correct these. Normal serum sodium levels are 135-145mEq/L (Martin, Fanaroff & Walsh, 2011a). Tommy’s sodium level is 133 and his urine output is increased. We could do a spot check of urine sodium to determine whether urine sodium losses are high (Gomella, pg.441). If the sodium spot check is > 20mEq/L, it can be related to acute/chronic renal failure (Gomella, 441). With adjusted IVFs, it is important to follow up in the morning with a set of electrolytes, paying particular attention to sodium level. Although the sodium is 133, true hyponatremia is defined as a serum sodium less than 130mmol/L (Martin, Fanaroff & Walsh, 2011a). In order to try and correct this, we would add more sodium to the TPN, so we would add Na 3 mEq/kg. Previously with the 2 mEq/kg, the patient was getting a total of 2.1 mEq/kg/day of sodium. By increasing the sodium to 3 mEq/kg, the patient now will receive 3.15 mEq/kg/day of sodium. CO2 16 is a concern because it alerts us that the patient is acidotic. An easy way to correct this would be to add acetate to the TPN. The sodium could be bound to acetate, and the potassium can be bound to chloride in the TPN. We would order electrolytes in the morning to monitor lab valus and see if the change in the TPN was effective at correcting the acidosis. CASE STUDY #1: TOMMY 10 DOL #12. Tommy remains stable in an open crib on NC@ 1/4LPM , 30% FiO2. He is tolerating feeds of 60 cc/kg/day; TPN of D12.5 W, 3.5 gm/kg protein, 3 gm/kg Intralipids, Na 3 mEq/kg, K 2 mEq/kg, Ca 2 .7 mEq/kg with total fluids (TF) = 160 ml/kg/day. PE remains unremarkable. Wt today = 3950 gm; UOP = 200ml for the past 24 hours, stools X 2 (guiac -). AM labs: Hct 35, Na 135, K 4.0, Cl 108, CO2 16, BUN 8, Cr 0.4, Ca 7.8, Gluc 118, Bili T/D 1.0/0.2. 15. hours? What is your fluid/feeding management plan with rationales for the next 24 Fluid/Feeding Plan: Increase feeds to 39.5 ml q 3 hours (80 cc/kg/day). Intralipids of 3 gm/kg (15cc/kg.day), TPN of D12.5 W (65 cc/ml/day) with 3.5 gm/kg protein, Na Acetate 3 mEq/kg, K Chloride 2 mEq/kg, Ca 2.7 mEq/kg to infuse at 13.1 ml/hr. Rationales: We would increase Tommy’s feeds to 80 cc/kg/day (39.5 ml q 3 hours), since he is tolerating his feeds. While we have increased his feeds to 80 cc/kg/day, we would not discontinue his intralipids until we increase his enteral feeds to 100 ml/kg/day (Cates, n.d.). With our fluids at 65 cc//kg/day, this yields a GIR of 6.9 mg/kg/min. The normal glucose requirement is 6-8 mg/kg/min, and although intake can be slowly increased to 10-12 mg/kg/min; it is not necessary to increase the GIR at this point due to our AM Glucose level being in within normal parameters (Gomella et al, 2013). Because the patient is on oxygen, we would leave the patient on 160 ml/kg/day. Although the patient is not on a high amount of oxygen, it is beneficial to watch the patient’s respiratory status and prevent increase work of breathing due to increase fluid intake. The current intralipids 3 gm/kg/day = 15 ml/kg/day. By discontinuing this, and increasing our feeds by 20cc/kg/day, we still have to decrease our TPN by 5ml/kg/day to maintain our fluids at 160ml/kg/day. It is necessary to keep our caloric intake of 100-120 kcal/kg/d for growth; this caloric intake yields a weight gain of 15-30 g/d (Gomella et al, 2013 pg.99). By keeping the TPN D12.5, our GIR is 5.6 mg/kg/min, our dextrose caloric intake would be 28.1 kCal/kg/day. Our amino acids at 3.5gm/kg provides 14 kCal/kg/day of protein. Our feeds of 80cc/ml/day provide 53.3Kcal/kg/day of feeds. Tommy’s intralipids are at 3gm/kg/day provide, which provide Tommy with 27 kCal/kg/day of lipids. This would give the patient 122.4 kcal/kg/d, which is adequate for desired weight gain. 16. Address this AM’s labs, cite any that may concern you, the rationale for your concern, and your plan. CO2 is 16, this tells us that Tommy is acidotic. In order to correct this, we can add 3 mEq/kg Sodium Acetate to the TPN, instead of the 3 mEq/kg Sodium Chloride. In the morning, we can get a set of electrolytes to see if acidosis has been corrected.The chloride level is slightly elevated; however, once we substitute the sodium chloride for sodium acetate, the chloride level should decrease slightly. This too will be monitored in the morning when the electrolytes are drawn. Tommy’s glucose is 118; we are increasing his GIR by 1 mg/kg/min to 7.9mg/kg/min, so we can increase our caloric intake. We will follow up electrolytes in the morning to monitor his glucose level. CASE STUDY #1: TOMMY 11 , DOL #20. Tommy is now 42 1/7 wks, current wt = 4100 kg. He is currently on 20 cal formula and EBM when available for TF 160 ml/kg/day. Wt gain has been very steady over the past 2 weeks. He is still unable to nipple all of his feeds as his oral motor coordination appears delayed. Current management plan: Meds: None Weekly labs: Na 136, K 4.2, Cl 104, Ca 7.8, glucose 120, Hct 26/retic 7.8. What changes, if any, do you recommend for Tommy’s nutritional regimen? 17. 18. If Tommy is receiving more EBM then formula, we may consider adding a multivitamin; however, if Tommy is feeding mostly formula, supplementation is not needed because the formula is fortified with Iron. Increase the feeds/TF to 180ml/kg/day (92 ml every 3 hours). Due to the fact that Tommy is having a hard time nippling, it would not be beneficial to have him po ad lib because he would not be able to po the amount needed to gain weight. Once he improves his nippling, po ad lib could be an option. Address lab results. Any changes? 19. Calcium is slightly low, but it still remains in acceptable range. If the infant is asymptomatic and has a total serum calcium level of more than 6.5 mg/dL or an ionized calcium level of more than 0.8-0.9 mmol/L, close observation alone is appropriate (Cates, n.d.). Calcium supplementation should be provided if the total serum calcium level is less than 6.5 mg/dL or if the ionized level is less than 0.8-0.9 mmol/L (Cates, n.d.). Patient has a hematocrit of 26, and although his retic count is a little elevated. The patient is not on any oxygen or having episodes of apnea or bradycardia; we would just continue to monitor at this time. Address current meds. Any changes? None. DOL #25. Tommy is now 42 6/7 wks. Wt today = 4250 gm. He is nippling all of his feeds of Enfamil 20cal w/iron for TF 160-180 ml/kg/day. He is stable on room air. You are making plans for his discharge to home and he will be rooming in with his parents prior to discharge. 20. What are your plans for discharge re: feeds, meds, supplements? Feeds: Patient will continue to feed Enfamil 20cal with iron. Patient will feed a minimum of 85 ml (160 ml/kg/day) every 3 hours, or 113 ml every 4 hours of Enfamil 20 cal. OR should we do po ad lib? Medications: None. Supplements: The patient is on an iron fortified formula, so there is no need for supplementation. Iron-fortified formula has become the formula of choice for term infants because its use has contributed to a decreased rate of anemia, and it is also fortified with oligosaccharides, nucleotides and probiotics (Gomella et al, 2013, pg105). CASE STUDY #1: TOMMY 21. 12 Other plans: MRI prior to discharge, Hepatitis B immunization, audiology screen, developmental screen, CCHD screen Patient can also have circumcision done, if requested by parents. Patient should have Hepatitis B immunization, audiology screen, developmental screen, CCHD screen, and total serum bilirubin prior to discharge. What global discharge teaching needs to be addressed prior to discharge? Parents should be instructed on the following: 22. Infant CPR Well baby care How to mix, store, and heat the formula When to call the pediatrician Signs of infection or dehydration Car seat safety Importance of practicing good hand hygiene How often the infant should eat and signs of feeding intolerance Avoiding contact with sick people and crowded places Do not allow the infant to be around anyone who smokes or in a smoking environment. Circumcision care, if applicable Importance of follow up appointments and keeping immunizations up to date What follow up appointments should be made prior to discharge? 23. Patient should follow up with pediatrician within 2-3 days. Neurology appointment ECI referral What discharge instructions need to be given to his parents about the needs of their growing newborn? nutritional Parents should be informed that growth rates during the neonatal period are more rapid then any other time (Blackburn, 2013). Parents should be informed that most healthy newborns show an average weight gain of 15-30 g/d (Gomella et al, 2013). Their baby should be eating every 3- 4 hours, with each feed not taking > 30-40 minutes is important for the risk of increased energy expenditure leading to weight loss.. Introduction of solid foods in generally recommended at 4-6 months (Blackburn, 2013). . CASE STUDY #1: TOMMY 13 References Armentrout, D. (2010). Acute renal failure in the neonate. [PowerPoint slides]. Retrieved from https://eclass.utmb.edu/bbcswebdav/pid-198840-dt-content-rid 2229223_1/courses/2142_UTMBG_GNRS_5631_SEC001/ModuleContent/Modu le%202/module2part1.html Blackburn, S. T. (2013). Gastrointestinal and hepatic systems and perinatal nutrition. Maternal, fetal, & neonatal physiology: a clinical perspective (4th ed., pp. 393442). Maryland Heights, MO: Elsevier Saunders. Cates, L.A. (n.d.). Fluid and ectrolyte calculations. [PowerPoint slides]/ Retrieved from https://eclass.utmb.edu/bbcswebdav/pid-198841-dt-content-rid 2229224_1 /courses/2142_UTMBG_GNRS_5631_SEC001/ModuleContent/Module%202/mo dule2part2.html Fernández, K. S., & de Alarcón, P. (2013). Neonatal thrombocytopenia. NeoReviews, 14(2), e74-e82. Martin, R. J., Fanaroff, A. A., & Walsh, M. C. (2011a). Fluid,electrolytes, and acid-base homeostasis. Fanaroff and Martin's neonatal-perinatal medicine: diseases of the fetus and infant (9th ed., pp. 669-684). Philadelphia: Saunders/Elsevier. Martin, R. J., Fanaroff, A. A., & Walsh, M. C. (2011b). The kidney and urinary tract. Fanaroff and Martin's neonatal-perinatal medicine: diseases of the fetus and infant (9th ed., pp. 1681-1702). Philadelphia: Saunders/Elsevier. (Martin, Fanaroff & Walsh, 2011) Utomo, M. T. (2012). Catheter Duration and the Risk of Sepsis in Premature Babies with Umbilical Vein Catheters. Indonesian Journal of Tropical and Infectious Disease, CASE STUDY #1: TOMMY 3(1), 10-14. 14