1. background - Springer Static Content Server
advertisement

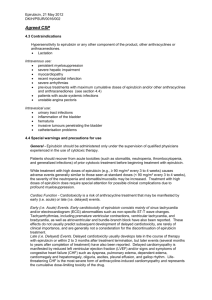
Title: 5-Fluorouracil, Epirubicin and Cyclophosphamide versus concurrent Epirubicin and Paclitaxel in node positive early breast cancer patients: a randomized, phase III trial of Gruppo Oncologico Nord-Ovest – Mammella Intergruppo Group (GONO-MIG5) STUDY COORDINATOR Dr.ssa Lucia Del Mastro Oncologia Medica A San Martino-IST Genova Steering Committee Lucia Del Mastro Paolo Bruzzi Marco Venturini PierFranco Conte E-mail: lucia.delmastro@hsanmartino.it Tel.0105558909 1 1. BACKGROUND Paclitaxel is known to have efficacy in patients with advanced breast cancer i,ii but its role is still to be established in the adjuvant setting. The GONO-MIG5 trial was designed to compare a standard anthracycline-containing chemotherapy regimen, i.e. 5fluorouracil, epirubicin, ciclophosphamide (FEC), given for 6 cycles to a new regimen containing both epirubicin and paclitaxel (EP), given concurrently, for 4 cycles in early breast cancer patients. This latter regimen was chosen on the basis of the results obtained in metastatic breast cancer patients, where the combination of doxorubicin and paclitaxel was associated with more than 90% of objective responseiii. Only four cycles of the new regimen were planned since the expected toxicity, particularly the cardiotoxicity, was high, and a short treatment duration was hoped to be the best strategy to obtain a favourable balance between the toxicity and the expected high efficacy. 2. STUDY POPULATION 2.1 Study patients Patients with node positive early breast cancer, candidate to receive adjuvant anthracyclinecontaining chemotherapy, will be enrolled in the study. 2.2 Inclusion Criteria: Women with histologically confirmed breast cancer who had undergone radical mastectomy or breast-conserving surgery in addition to full ipsilateral axillary lymph node dissection Lymph node-positive disease with less than 10 involved axillary lymph nodes Surgery performed not more than 5 weeks before randomization ECOG performance status 0 Absolute neutrophil count ≥ 2,000/mm³ 2 WBC ≥ 3,000/mm³ Platelet count ≥ 100,000/mm³ Bilirubin ≤ 1.5 times upper limit of normal (ULN) AST and ALT ≤ 1.5 times ULN Postoperative regional radiotherapy limited to the remaining breast admitted for patients who received breast-conserving surgery Written informed consent 2.3 Exclusion Criteria: Prior or concurrent ipsilateral or contralateral invasive breast carcinoma within the last 10 years Metastatic disease, including metastasis in the ipsilateral supraclavicular lymph nodes Prior chemotherapy or prior cytotoxic regimens or prior hormonal therapy Pregnant or nursing Other serious medical illness requiring medication, uncontrolled infections Other malignancy except adequately treated, cone-biopsied in situ carcinoma of the cervix or basal cell or squamous cell carcinoma of the skin Recent myocardial infarction, congestive heart failure, or serious arrhythmia 3. STUDY DESIGN The study is an open-label, phase III, randomized clinical trial. Patients will be randomly assigned 1:1 to receive one of two arms: ARM A Fluorouracil 600 mg/mq iv d1 Epirubicin 60 mg/mq iv d1 Cyclophosphamide 600 mg/mq iv d1 Every 3 weeks for six cycles 3 ARM B Paclitaxel 175 mg/mq iv d1 Epirubicin 90 mg/mq ev d1 Every 3 weeks for four cycles. Patients should not receive primary prophylaxis with G-CSF. G-CSF can be given by subcutaneous injection in case of absolute neutrophil count < 500/µL. Tamoxifen at 20 mg/day for 5 years is admitted for all postmenopausal patients, regardless the hormonal receptor status and to premenopausal patients whose tumors were positive for the estrogen and/or progesterone receptor. Tamoxifen will be started at the same time of chemotherapy. Postoperative regional radiotherapy limited to the remaining breast will be given to patients who received breast-conserving surgery. 4. STUDY OBJECTIVES 4.1 Primary objective To assess overall survival 4.2 Secondary objectives - To assess the toxicity of treatment - To assess event free survival 5. EFFICACY EVALUATIONS 4 The primary study end point is overall survival (OS), as estimated from the date of randomization to the date of death from any cause. Secondary endpoints include event-free survival (EFS) and toxicity. EFS is computed from the date of randomization to the date of local recurrence, distant metastases, second primary cancer, or death from any cause, whichever came first. All adverse events and laboratory parameters will be graded according to the World Health Organization Criteriaiv. 6. STUDY PROCEDURES At baseline The following assessments and procedures should be performed before randomization; • written informed consent • menopausal status and for all women of childbearing potential, serum pregnancy test • medical history • date of diagnosis, type and characteristics of the primary tumor (histology, grade and stage, hormonal status and ErbB2) • electrocardiography • concomitant medications • physical examination, ECOG PS, height in cm, weight in kg • hematology and blood chemistry • Clinical and instrumental evaluation to exclude secondarism (Bone scan and radiographic imaging i.e. chest radiograph, liver ultrasound or computer tomography) The following assessments and procedures should be performed before every cycle: • physical examination, ECOG PS, weight in kg • Record of toxicity • hematology At the end of chemotherapy: 5 • physical examination, ECOG PS, weight in kg • Record of toxicity • hematology Assessments during the follow-up • Clinical visit every 3 months between 1 and 3 years • Clinical visit every 6 months between 4 and 5 years • Clinical visit each year between 5 and 10 years • Annually hematology and mammography 7. CRITERIA FOR TREATMENT INTERRUPTION OR DISCONTINUATION Toxicity will be graded according to WHO criteriaiv. 7.1 Haematological Toxicity Events prior to cycle WBC (white blood cells) Platelets WBC ≤ 2 x 109/L Platelets ≥ 90 x 109/L Chemotherapy Hold until Pt ≥ 100 x 109/L WBC between 2 and 3 x 109/L Platelets between 50 and 90 x and WBC ≥ 3 x 109/L 109/L WBC ≤ 2 x 109/L Myelosuppression > 2 weeks Platelets between 50 and 90 x 109/L Delay until recovery then Platelets ≤ 50 x 109/L decrease dose by 25% Discontinue chemotherapy 6 7.2 Non haematological toxicity Adverse events Action Non haematological, grade 1 Continue therapy Non haematological, grade 2 Hold Therapy until resolution of symptoms Non haematological, grade 3 or 4 (except for Hold Paclitaxel therapy until recovery of alopecia) symptoms then decrease dose by 25% Non haematological, grade 3 or 4 after 25% dose Consider dose reduction by 50% or reduction discontinue therapy 7. 4 Treatment discontinuation Treatment should be discontinued if: -unacceptable toxicity -investigators’s decision due to an AE or other reason -consent withdrawn -progression of disease Patients who interrupt treatment should continue follow-up post-treatment. 8. STUDY DRUGS ARM A Epirubicin (E) will be administered by short intravenous (IV) infusion at a dose of 60 mg/m² on D1 of each cycle, Cyclophosphamide (C) will be administered by short IV infusion at a dose of 600 mg/m2 on D1 of each cycle. Fluoruracil (F) will be administered by short IV infusion at a dose of 600 mg/m2 on D1 of each cycle. 7 Cycles were repeated every 3 weeks for a total of 6 cycles. Before each cycle, patients received dexamethasone (12 mg) and ondansetron (8 mg) or tropisetron (5 mg) or granisetron (3 mg). ARM B Paclitaxel (P) will be administered by 3-hours intravenous (IV) infusion at a dose of 175 mg/m² on D1 of each cycle, Epirubicin (E) will be administered by short intravenous (IV) infusion at a dose of 90 mg/m² on D1 of each cycle, Cycles were repeated every 3 weeks for a total of 4 cycles. Before each cycle, patients received dexamethasone (20 mg), orphenadrine (40 mg), ranitidine (50 mg). 9. STATISTICAL CONSIDERATIONS It is assumed that the minimal therapeutic effect worth detecting in this study, considering the increased toxicities and economic costs associated with the use of paclitaxel in the adjuvant therapy, has to be a 20% relative reduction in the hazard of death. In order to detect this reduction with an 80% power, at the significance level of 5% (2-sided), it is estimated that 640 events has to be observed. 500 patients per arm over a 5-year period has to be enrolled and the final analysis will be conducted after additional 6 years of follow up (11 years after the first randomization). All analyses will be conducted according to the intention-to-treat principle, in that all patients randomly assigned to a treatment arm will be considered as belonging to the arm to which they had been assigned at randomization. Overall survival and event-free survival will be obtained from Kaplan-Meier analyses, and the primary comparison between the two study arms will be performed with the log-rank test. A multivariate Cox proportional hazard analysis that used covariates that could influence the timeto-event endpoints (i.e. age, receptor status, nodal status, grading, surgical treatment and menopausal status) will be performed for overall survival and event free survival. A 12-month 8 Kaplan-Meier landmark analysis will be performed to assess the effect of chemotherapy-induced amenorrhea on survival and event free survival, respectively, for the combined treatment groups of premenopausal women and for subgroups of patients on the basis of their hormonal receptors status. Premenopausal status will be defined by the occurrence of a menstrual period within 6 weeks before random assignment. Perimenopausal status will be defined by the occurrence of a menstrual period more than 6 weeks but no more than 12 months before random assignment. Chemotherapy-induced amenorrhea will be defined by the absence of menstrual activity for at least 6 months during chemotherapy or within 12 months after the end of chemotherapy. 10. ADVERSE EVENT REPORTING When toxicity occurs, it should be graded according to WHO criteriaiv. Definition of an adverse event Patients will be instructed by the investigator to report the occurrence of any adverse event. An adverse event is any undesirable event associated with the use of a drug, whether or not considered drug related, and includes any side effect, injury, toxicity, or sensitivity reactions. It also includes any undesirable clinical or laboratory change, which does not commonly occur in the patient, and may: o results in study withdrawal o is associated with a serious adverse event o is associated with clinical signs or symptoms o is considered by the investigator to be of clinical significance. 10.1 Definition of Serious Adverse Event A serious adverse event (SAE) is any event that is fatal, life-threatening, requires or prolongs hospitalization, results in persistent or significant disability or incapacity, a congenital anomaly or birth defect, an important medical event. 9 “Life-threatening" means that the patient was at immediate risk of death from event as it occurred. It does not include an event that, had it occurred in a more serious form, might have been life threatening (i.e. asymptomatic febrile neutropenia). Requires in patient hospitalization or prolongation of existing hospitalization" should be defined as hospital admission required for treatment of the adverse event or occurred as a consequence of the event. Hospital admission for scheduled elective surgery would not be a serious adverse event. “Important medical events” are those which may not resulted in death or be immediately life-threatening or result in patient hospitalization, but may jeopardize patients and may require intervention to prevent one of the other serious outcomes listed above. Examples of such events are intensive treatment in an emergency room or at home for allergic bronchospasm; blood dyscrasias or convulsions that do not result in hospitalization; development of drug dependency. A second malignancy or drug overdosage or abuse may be considered serious by this criterion. All adverse events which do not meet any of the criteria for serious should be regarded as nonserious adverse events. Events NOT considered to be SAEs are hospitalizations for: routine treatment or monitoring of the studied indication, not associated with any deterioration in condition treatment, which was electiveor pre-planned, for a pre-existing condition that did not worsen admission to a hospital or other institution for general care, not associated with any deterioration in condition treatment on emergency, outpatient basis for an event not fulfilling any of the definitions of serious given above and not resulting in hospital admission All serious adverse events occurring during the study treatment period or within 30 days following the last drug administration must be reported according to the procedure described below. Any late SAE (occurring after this 30 days period) possibly or probably related to the study treatment should 10 follow the same reporting procedure. Progression of a patient's underlying condition leading to one of the above should not be reported as a serious adverse event. The following definitions will be used to asses causality: None: The clinical adverse event is definitely unrelated to the study drug (e.g., does not follow a reasonable temporal sequence from study drug administration, present prior to receveing study medication, etc.). Remote: The study is not likely to have had reasonable association with the observed experience; however, relationship cannot be definitely excluded. Possible: The connection with study drug administration appears feasible, but cannot be concluded with certainty (e.g., follows a reasonable temporal sequence from drug administration, may be related to known characteristics of the patient’s clinical state or other modes of therapy administered to the patient, etc.). Probable: The clinical adverse event appears related to the study drug with a high degree of certainty (e.g., follows a reasonable temporal sequence from drug administration and abates upon discontinuation of the drug, cannot be reasonably explained by known characteristics of the patient’s clinical state or other modes of therapy administered to the patient, etc.). If the adverse event is serious, it must be reported within 1 working day by fax on the provided SAE form, to Local Ethic Committee. Withdrawal from the study and therapeutic measures shall be at the discretion of the investigator. A full explanation for the discontinuation from the study will be made on the appropriate case report form. All adverse events, regardless of severity, will be followed up by the investigator until satisfactory resolution. The investigator and persons in charge of patient care should institute any supplementary investigations of major adverse events based on their clinical judgment of the likely causative factors. This may include seeking a further opinion from a specialist in the field of the adverse event. All other minor adverse reactions will be collected on the CRF during the study. 11 These responsibilities are accepted by the investigator once he/she signed the investigator agreement. 11. ETHICAL ASPECTS The study will be conducted in accordance with good clinical practice (GCP), all applicable subject privacy requirements and the guidind principles of the declaration of Helsinki. 12. DATA REGISTRATION Registration will take place after the patient has provided written informed consent and eligibility has been verified. The patient registration will be done through a centralized database of the Centre Promoter / Coordinator accessible via phone or fax (010/354103) Patients will be assigned to a treatment arm according to stratified random lists that will be balanced in blocks of various sizes in random sequence. The management of patient data will be performed in accordance with all applicable subject privacy requirements. 13. ADMINISTRATIVE ASPECTS This study is partially supported by a grant from Brystol Myers Squibb. 14. STUDY DURATION Planned enrollment start date: November 1996 Planned enrollment end date: October 2001 REFERENCES 12 i . Holmes FA, Walters RS, Theriault R, et al: Phase II trial of taxol, an active drug in the treatment of metastatic breast cancer. J Natl Cancer Inst 83:1797-1805, 1991 ii . Gianni L, Munzone E, Capri G, et al: Paclitaxel in metastatic breast cancer: a trial of two doses by a 3-hour infusion in patients with disease recurrence after prior therapy with anthracyclines. J Natl Cancer Inst 87:1169-1175, 1995 iii . Gianni L, Munzone E, Capri G, et al: Paclitaxel by 3-hour infusion in combination with bolus doxorubicin in women with untreated metastatic breast cancer: high antitumor efficacy and cardiac effects in a dose-finding and sequence-finding study. J Clin Oncol 11:2688-2699, 1995 iv . Miller AB, Hoogstraten B, Staquet M, et al: Reporting results of cancer treatment. Cancer 7:207214, 1981 13