Sexual Reproduction in Humans.
advertisement

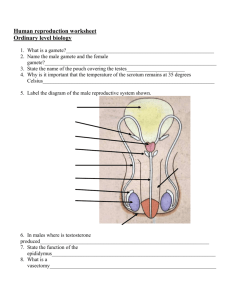
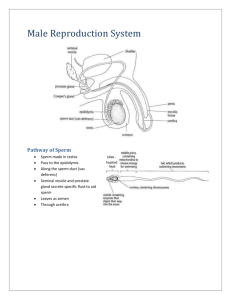
Sexual Reproduction in Humans Insemination – semen being released into the vagina just outside the cervix Ejaculation – the release of sperm from the penis Acrosome – digestive enzymes in head of the sperm which digest an opening through membrane of the egg Androgens – male hormones that cause the primary and secondary male sex characteristics Fertilisation – nucleus of the egg fusing with the nucleus of the sperm Gestation – the amount of time the foetus spends in the uterus Birth control – deliberate prevention of pregnancy Male reproductive system Testes – Makes the sperm Epididymis – Matures the sperm Sperm ducts – Carries sperm from testes to urethra Seminal vesicle – Forms seminal fluid Prostate gland – Forms seminal fluid Cowpers gland – Neutralises urethra for passage of sperm Penis – Organ of copulation Scrotum sac – Responsible for holding sperm at 35 degrees for meiosis to occur Hormones in the male reproductive system: 1. F.S.H. (follicle stimulating hormone) causes the sperm producing cells in the testes to produce sperm 2. L.H. (lutenising hormone) stimulates the testes to produce testosterone Primary male sex characteristics Growth of penis and descent into scrotum Development of other male reproductive parts Secondary male sex characteristics Growth of underarm, face, and body hair Widening of shoulders Growth spurt Male infertility Definition –Inability to produce offspring Cause – low sperm count, possibly due to alcohol, cigarettes or drug abuse Corrective measures – Change in lifestyle and diet Female reproductive system Ovary- produces and matures eggs Ovary ligament- holds ovary in place Funnel- collects egg after ovulation Fallopian tube- site of fertilisation Uterus- site of pregnancy Lining of uterus- maintains pregnancy Cervix- opening to uterus Vagina- birth canal Menstrual cycle 1-28 day Days 1-5 menstruation occurs Lining of womb breaks down Meiosis occurs in ovary to produce a new egg surrounded by graafian follicle Day’s 6-14 graafian follicle produces oestrogen Endomentrium thickens No further eggs mature in ovary High levels cause pituitary to release L.H. Day 14 ovulation occurs (L.H. produced by pituitary) Passes into fallopian tube (if sperm is present fertilisation may occur, egg is only viable for 48 hours Causes graafian follicle to become corpus leutum Days 14- 28 corpus leutum produces progesterone Prevents contractions of the uterine lining Thickens and maintains the lining Prevents further L.H. and F.S.H. being secreted Hormones in the female reproductive system: 1. F.S.H. (follicle stimulating hormone) causes meiosis in ovary and production of the graafian follicle 2. Oestrogen causes maturing of follicle/ thickens lining & inhibits F.S.H 3. L.H. causes ovulation/ triggers production of corpus leutum/ causes progesterone production 4. Progesterone maintains endometrium/ prevents uterine contractions/ inhibits L.H. & F.S.H Female infertility Definition inability to produce offspring Causes failure to ovulate e.g. maybe a hormonal disorder, stress or a tumour Corrective measures hormonal treatment or surgery on the ovary Foetal growth Events from fertilisation to implantation of embryo Takes up to 6-9 days Fertilised egg contains 46 chromosomes. The zygote divides rapidly by mitosis – 16 cells produces morula (2/3 days) At day 5/6 the morula keeps dividing to produce a large hollow ball called the blastocyst. It is moved down the fallopian tube (wafted by cilia and contractions of uterus) When it reaches the endometrium the outer layer of cells of blastocyst forms the trophoblast It later forms membranes around the embryo Implantation occurs, trophoblast cells & endometrium cells begin to form placenta (trophoblast forms tiny extentions that grow into the prepared wall) Early development of the embryo After implantation the blastocyst obtains its nutrition by absorption through the trophoblast cells from endometrium Development of the embryo cell sees the formation of the 3 germ layers Ectoderm- skin, nails, nervous system Mesoderm- bone, blood vessels & kidneys Endoderm- inner lining of intestines, lungs, & liver By week 8 all the major organs are formed (now called a foetus) By week 12 the eyes are low & widely spaced, cartilage is replaced by bone, sex organs are distinguishable, baby teeth begin to grow By week 12 the baby is fully formed and no new organs will develop. All features will be defined & the baby continues to grow The placenta Development: It develops from the embryonic & uterine tissues The trophoblast forms villi which embed into the lining of the endometrium By week 12 the placenta is fully formed & takes over production of oestrogen & progesterone The umbilical cord connects the placenta to the embryo Functions: Transfer of food, gases, and excretory products between embryo and mother Prevents the transfer of pathogens, blood cells, and hormones Secretes the hormones progesterone and oestrogen Keeps the 2 bloods separate as their blood groups could be different and the mother’s blood pressure is too strong for the baby Stages of birth Stage 1: Foetus rotates towards the cervix Oxytocin stimulates contractions of the uterus and the cervix dilates Amniotic fluid bursts Contractions begin Stage 2: Frequent contractions Foetus is pushed out head first Stage 3: The placenta and the foetal membrane are expelled Lactation Secretion of milk by mammary glands Stimulated by prolactin from the pituitary gland Biological benefits- correct nutrients, antibodies, bonding and helps the mother regain shape I.V.F Fertilisation outside the body Female is given fertility drugs to stimulate eggs to develop Eggs are removed from the ovary and mixed with sperm in a glass dish A number of the fertilised eggs are replaced back in the uterus for implantation Birth control/ contraception Deliberate prevention of pregnancy Four methods - Natural (rythm method) - Mechanical (condom/ diaphragm - Chemical (birth control pill/ spermicides) - Surgical 9tube ligation/ vasectomy)