psychological support in the long term transplant patient
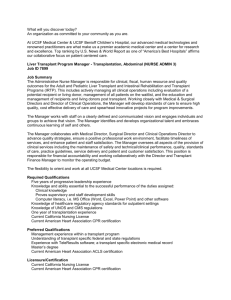
advertisement

P113 PREVALENCE OF PSYCHOLOGICAL ILLNESS IN LONG-TERM RENAL TRANSPLANT PATIENTS Frame, S¹, Andre, T¹, Suleman, S¹, Goldsmith, D¹, Cronin, A² ¹Guy’s & St Thomas’ NHS Foundation Trust, NIHR Biomedical Research Centre, ²MRC Centre for Transplantation, King’s College, London INTRODUCTION: The high prevalence of psychological illness, in particular anxiety and depression, in patients with kidney disease is well documented, suggesting it is a common problem among these patients. However the prevalence of psychological illness in long-term transplant patients is less clear. The National Institute for Health and Clinical Excellence has published a report indicating depression is two-three times more common in adults with a chronic physical health problem than in healthy people (NICE 2009). Many complications may occur following transplantation and the mortality of transplanted patients remains high compared to age-matched non-CKD general populations. As a result long-term transplant patients may be susceptible to psychological illness. There is a major drive nationally to improve the care of patients with long-term conditions and improve outcomes. Recommendations aiming to achieve this have been set out. In order to meet these recommendations in May 2010 we established a multi-professional Annual Review Renal Transplant Clinic that focuses on longer-term healthcare management and offers screening for a variety of health conditions associated with transplantation. Our clinic provides in-depth clinical consultations that allow time for patients to discuss their general physical and psychological health, and quality of life. In addition, prior to consultation all patients attending the clinic are requested to complete a Hospital Anxiety and Depression Self-Assessment Scale (HADS) questionnaire (Zigmond & Snaith 1983). This questionnaire assesses the role of emotional factors in clinical practice and sets out criteria for referral to a specialist psychologist. METHODS: We undertook in-depth clinical consultations and assessed the HADS score on 335 long-term (> 8 years post transplant) patients attending our Annual Review Renal Transplant Clinic over a period of 32 months from May 2010-December 2012. We offered referral to a specialist renal psychologist to all patients who met HADS score criteria for this. RESULTS: In our series of 335 patients, 16% (n=54) reported being seen previously by a counsellor, psychologist or psychiatrist. 100% (n=335) completed the HADS questionnaire. On the basis of HADS scores we identified 29 (9%) patients who met the criteria for referral to our renal psychology service. Increased symptom burden was reported in this group. Of these 29 patients, 6 (21%) were subsequently referred to our local mental healthcare team. A broad range of conditions ranging from anxiety (n=6), depression (n=12), sexual & relationship difficulties (n=4), bereavement disorder (n=2), obsessive compulsive disorder (OCD) (n=1), work related stress (n=3), and psychosis (n=1) have since been formally diagnosed. CONCLUSION: There is an increased prevalence of psychological illness, particularly anxiety and depression, in long-term transplant patients. This indicates there is a need to assess the contribution of mood disorder, especially anxiety and depression in this group. In our experience the HAD self-assessment scale is a simple yet reliable tool for identifying individuals attending the Annual Review Renal Transplant Clinic who require further psychological assessment and support. Further work to identify and understand the reasons underpinning the increased prevalence of psychological illness in long-term transplant patients is required. Symptom burden may be a contributory factor.