1. de la C-mara C, Arrieta R, Gonz-lez A, Iglesias E, Ome
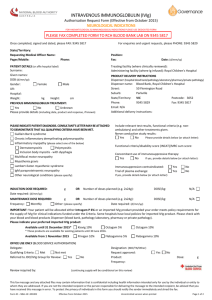
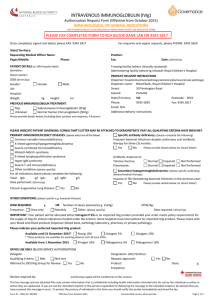
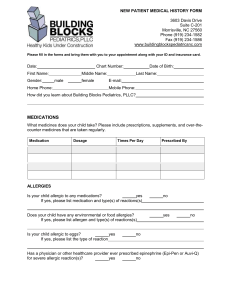
advertisement
http://www.ncbi.nlm.nih.gov/pubmed/7473429?dopt=Abstract http://www.fertilitymemphis.com/intro_IVIG_study.asp http://www.usmamed.com/02fertility/news_IVIG.htm http://www.earlypregnancy.org/EPBM/EPBM%20IV/Vol.%20IV,%20Num%202/EPBM11 33.htm http://www.obgyn.net/firstcontroversies/prague1999daya4.htm http://www.blackwell-synergy.com/links/doi/10.1111/j.8755-8920.2001.450309.x/abs/ http://www.recurrentmiscarriages.com/out_frame.php?PHPSESSID=3f04c448439d2807 874090655e34d56a&ID=77 http://www.recurrentmiscarriages.com/out_frame.php?PHPSESSID=3f04c448439d2807 874090655e34d56a&ID=239 http://www.recurrentmiscarriages.com/out_frame.php?PHPSESSID=3f04c448439d2807 874090655e34d56a&ID=330 http://repro-med.net/papers/2ndabor.php http://www.earlypregnancy.org/EPBM/EPBM%20IV/Vol.%20IV,%20Num%202/EPBM12 88.htm 1. de la C-mara C, Arrieta R, Gonz-lez A, Iglesias E, Ome-aca F. High dose intravenous immunoglobulin as the sole prenatal treatment for severe Rh immunization. N Engl J Med 1988;318:519-520. 2. Smith CIE, Hammarstrom L. Intravenous immunoglobulin in pregnancy. Obstet Gynecol 1985;66:39s. 3. Scott JR, Branch W, Kochenour NK, Ward K. Intravenous immunoglobulin treatment of pregnant patients with recurrent pregnancy loss caused by antiphospholipid antibodies and Rh immunization. Am J Obstet Gynecol 1988;159:1055-1056. 5. Bustillo M. Goodman C.: Assisted reproductive technologies and immune infertility. Am. J. Reprod. Immunol., 35:205-289, 1996. 6. Matzner W. Presentation at Pacific Coast Infertility Meeting, 1998. 4. Parke A, Maier D, Wilson D, Andreoli J, Ballow M. Intravenous gammaglobulin, antiphospholipid antibodies, and pregnancy. Ann Int Med 1989;110:495-496. 5. Rose V, Gordon Ll. Idiopathic thrombocytopenic purpura in pregnancy. Successful management with immunoglobulin infusion. JAMA 1985;254:2626-2628. 6. Bussell JB, Pham LC, Aledort L, Nachman R. Maintenance treatment of adults with refractory immune thrombocytopenic purpura using repeated intravenous infusions of gamma globulin. Blood 1988;72:121127. 7. Mannhalter JW, Ahmad R, Wolf HM, Eibl MM. Effect of polymeric Edge on human monocyte functions. Int Arch Allergy Appl Immunol 1987;82:159-167. 8. Sultan Y, Maisonneuve P, Kazatchkine MD, Nydegger UE. Anti-idiotypic suppression of autoantibodies to factor VIII b high dose intravenous gammaglobulin. Lancet 1984;i:765-768. 9. Sher G, Feinman M, Zouves C, Kuttner G, Maassarani G, Salem R, Matzner W, Ching W, Chong P. High fecundity rates following in vitro fertilization and embryo transfer (IVF/ET) in antiphospholipid antibody (APA) seropositve women treated with heparin and aspirin. Human Reproduction 1994;11. 10. Tsubakio T, Kurato Y, Katageri S, et al. Alteration in T cell subset and immunoglobulin synthesis in vitro during high dose gammaglobulin therapy in patients with idiopathic thrombocytopenic purpura. Clin Exp Immunol 1983;53:697-702. 11. Wapner RJ, Cowchock SF, Shapiro SS. Successful treatment in two women with antiphospholipid antibodies and refractory pregnancy losses with intravenous immunoglobulin infusions. Am J Obstet Gynecol 1989;161:1271-1272. 12. Kwak JYH, Gilman-Sachs A, Beaman KD, Beer AE. Reproductive outcome in women with recurrent spontaneous abortions of alloimmune and autoimmune etiologies; pre vs. post conception treatment. Am J Ostet Gynecol 1992;166:1975-1987. 13. Kwak JYH, Gilman-Sachs A, Beaman KD, Beer AE. Autoantibodies in women with primary recurrent spontaneous abortion of unknown etiology. J. Reprod Immunol 1992;22:15-31. > -------------------------------------------------> > 3) Early Pregnancy 2000 Apr;4(2):154-64 > > Immunoglobulin G infusion treatment for women with recurrent > spontaneous abortions and elevated CD56+ natural killer cells. > > Kwak JY, Kwak FM, Gilman-Sachs A, Beaman KD, Cho DD, Beer AE. > > Reproductive Medicine, Department of Obstetrics and Gynecology, Finch > University of Health Sciences/The Chicago Medical School, North > Chicago, IL 60064, USA. kwakj@m... > > We aimed to investigate the clinical effect of intravenous > immunoglobulin G (IVIg) treatment in recurrent aborters with elevated > peripheral blood CD56+ NK cell levels while on lymphocyte > immunization, anticoagulation and prednisone treatment, with respect > to subsequent live birth and reproductive outcome. Thirty-three women > with recurrent abortions achieved alloimmune recognition after > lymphocyte immunizations. All had autoimmune abnormalities and > received preconception anticoagulation and prednisone treatment. At > the time of positive pregnancy testing, 18 women with normal NK cell > levels (<12%) and 6 with elevated NK cell levels (>12%) continued > anticoagulation and prednisone treatment, and 9 with elevated NK cell > level initiated additional IVIg treatment. The live birth rates of > women with elevated NK cell level (>12%) who initiated post> conception IVIg treatment in addition to anticoagulation and > prednisone (100.0%), women with normal NK cell levels (<12%) who > continued anticoagulation and prednisone (83.3%) and women with > elevated NK cell level (>12%) who continued anticoagulation and > prednisone (33.3%) are significantly different (P=0.0065). Prevalence > of intrauterine growth retardation and preterm delivery among 3 study > groups were not different. In conclusion, post-conception IVIg > treatment significantly improves reproductive outcome in women with > elevated CD56+ NK cells with pregnancy who received preconception > lymphocyte immunization, anticoagulation and prednisone treatment. > > PMID: 11723544 [PubMed - indexed for MEDLINE] > > -----------------------------------------> > 4) Am J Reprod Immunol 2001 Oct;46(4):268-73 > > Further experience with intravenous immunoglobulin in women with > recurrent miscarriage and a poor prognosis. > > Carp HJ, Toder V, Gazit E, Ahiron R, Torchinski A, Mashiach S, > Shoenfeld Y. > > Department of Obstetrics and Gynecology, Sheba Medical Center, Tel > Hashomer, Israel. carp@n... > > PROBLEM: Women with three or more unexplained miscarriages have a 60% > chance of a subsequent live birth. Intravenous immunoglobulin (IVIG) > has not been conclusively shown to improve this prognosis. This study > assessed the effect of IVIG in patients expected to have a poor > outcome if untreated, i.e. women with five or more abortions, who > have aborted after paternal leukocyte immunization or who continue to > abort despite expressing anti-paternal complement dependent antibody. > METHODS: Seventy-six women received IVIG in a dose of 400 mg/kg body > weight, in one day (total 30-45 g) in the follicular phase of a cycle > in which pregnancy was planned. A booster dose was administered when > pregnancy was diagnosed. Their results were compared to an untreated > control group of 74 women. RESULTS: Thirty-five (49%) pregnancies in > treated women have resulted in live births or passed their previous > stages of abortion compared to 23 (31%) in control patients (P = > 0.04). CONCLUSIONS: These figures indicate that IVIG may prevent > further miscarriages in this poor prognosis population. These figures > are especially significant considering the doubt concerning the > efficacy of IVIG in patients with three miscarriages and therefore a > relatively good prognosis. > > Publication Types: > > Clinical Trial > ------------------------> 5) > > 1: Scand J Rheumatol Suppl 1998;107:97-102 > > Utilization of intravenous immunoglobulin therapy to treat recurrent > pregnancy loss in the antiphospholipid syndrome: a review. > > Harris EN, Pierangeli SS. > > Academic Affairs, Morehouse School of Medicine, Atlanta, GA 30310> 1495, USA. > > Although experience is still limited, intravenous immunoglobulin > therapy for recurrent pregnancy loss in the Antiphospholipid Syndrome > (APS) may represent a significant advance. APS was widely recognized > only fifteen years ago. Pregnancy loss and thrombosis are the > prominent clinical features. Initially, prednisone was used for > treatment of pregnancy loss, but matemal and fetal complications > stimulated searches for alternative therapy. Subcutaneous heparin and > low dose aspirin was next utilized, but although efficacious, there > is still a 30% failure rate, and intrauterine growth retardation, > prematurity, and pre-eclampsia are relatively frequent. In the late > 1980's, there were a number of case reports of successful pregnancy > outcomes after treatment with intravenous immunoglobulin (IVIg) but > regimens differed. Series from two centers have confirmed these > initial findings and treatment regimens have become more consistent. > Both centers have reported success with doses of 400 mg/kg/day for 5 > days or 1 g/kg/day for two days each month initiated during the first > or early second trimester. Success rates of 70-100% have been > reported, and complications such as pre-eclampsia, intrauterine > growth retardation, and premature births appear reduced, when > compared to prednisone and low dose aspirin or heparin and low dose > aspirin. Several patients who were treated with IVIg also received > heparin, making it uncertain whether heparin may also need to be > added to IVIg. Intravenous immunoglobulin is safe, but expensive. > Despite its expense, if IVIG is shown to markedly decrease matemal > and fetal morbidity, it may be the logical treatment of choice to > prevent pregnancy loss in APS. > > Publication Types: > > Review > Review, Tutorial > > PMID: 9759143 [PubMed - indexed for MEDLINE] > > -----------> > 6) > > Fertil Steril 2000 Mar;73(3):536-40 > > > > Successful treatment of immunologic abortion with low-dose > intravenous immunoglobulin. > > Stricker RB, Steinleitner A, Bookoff CN, Weckstein LN, Winger EE. > > California Pacific Medical Center, San Francisco, California 94108, > USA. rstricker@u... > > OBJECTIVE: To evaluate the efficacy of low-dose intravenous > immunoglobulin (IVIG) treatment in older women with immunologic > abnormalities and recurrent spontaneous abortion (RSA), a condition > referred to as immunologic abortion. DESIGN: Prospective clinical > trial. SETTING: Outpatient referral practice. PATIENT(s): Fortyseven > women were enrolled in the study. The mean age of the women was 37 > years (range, 28-45 years), and the mean number of prior miscarriages > was 3.7. Immunologic abnormalities included antiphospholipid > antibodies (32%), antithyroid antibodies (53%), antinuclear > antibodies (28%), antiovarian antibodies (2%), increased natural > killer cells (40%), increased immunoglobulin (Ig)M level (28%), and > increased CD4/CD8 T-cell ratio (15%). One patient had IgA deficiency, > and three women had endometriosis. Thirty-one of the 47 patients > (66%) had more than one immunologic abnormality. INTERVENTION(s): > Treatment with IVIG at a dose of 0.2 g/kg within 2 weeks of attempted > conception. Once conception was achieved, IVIG treatment was > continued on a monthly basis at the same dose through 26-30 weeks of > gestation. MAIN OUTCOME MEASURE(s): Successful pregnancy or recurrent > abortion.Result(s): Of the 47 women, 36 received initial IVIG > treatment, and 24 subsequently became pregnant. Of these women, 20 > continued IVIG treatment through 26-30 weeks of gestation, and 19 > (95%) had a successful term pregnancy. Four women discontinued IVIG > therapy after 10-12 weeks of gestation, and 3 (75%) had a successful > pregnancy outcome. Of the 11 women who refused IVIG therapy, 7 became > pregnant, and all 7 miscarried. The difference in pregnancy success > rate between the IVIG-treated and untreated groups was significant > (P=.001). Three women had adverse reactions during the low-dose IVIG > infusion, and these reactions resolved when the IVIG brand was > changed. Fetal abnormalities were not observed. CONCLUSION(s): Low> dose IVIG therapy is beneficial for older women with immunologic > abortion. The optimum duration of IVIG treatment in these women > requires further study. > > Publication Types: > Clinical Trial > > PMID: 10689009 [PubMed - indexed for MEDLINE] > ------------------------------> > 7) > > Intravenous Immunoglobulin G (IVIG) Is Associated with Markedly > Improved IVF Outcome in Patients with Elevated Peripheral Natural > Killer Cell Activity (NKa+) and Prior Unexplained IVF Failure. > 1, 2, G Sher, 1JD Fisch, 1, 2G Maassarani, 1L Danner. 1Sher Institute > for Reproductive Medicine, Las Vegas NV, 2Dept. of Ob/Gyn, University > of Nevada School of Medicine, Reno NV. > > Objective: We previously reported increased IVF pregnancy rates among > Antiphospholipid Antibody (APA) positive patients in whom > immunomodulation with Heparin alone was unsuccessful. We also > reported an association of APAs among infertile women with elevated > Natural Killer cell activity (NKa+). This study evaluated the effect > of IVIG therapy on IVF outcomes in a group of NKa+ patients with > prior unexplained IVF failures. > > Design: Retrospective cohort. > > Materials and Methods: Between January and December, 2001, 20 > infertile NKa+ women <40 years of age, with an otherwise normal > uterine cavity (Group A, n=24) underwent 24 fresh IVF cycles using > their own eggs and standard stimulation protocols with the addition > of IVIG (40 g) prior to egg retrieval and a second infusion after > confirming conception. In all cycles the patient had at least 2 Grade > A embryos (7 or more cells and <20 fragmentation on day 3 of culture) > available for transfer. All patients had elevated peripheral blood NK > cell activity as measured by a K562 cell assay with more than 10% > killing considered abnormal. In addition, all patients had a least > one prior failed ART attempt (mean 1.8). Group A was compared to a > matched cohort of 22 historical NKa+ controls (Group B) who were > offered IVIG treatment between October 1998 and December 2001, but > who declined therapy. Differences in rates between groups were > analyzed using Chi Squared tests. Significance was set at p<0.05. > > Results: The overall on-going pregnancy rate among the two groups was > 35% (16/46). In Group A the pregnancy rate was 63% (15/24), which was > significantly higher, than for Group B (1/22; 4%) (p<0.001). There > were no other significant differences between the 2 groups in terms > of age, diagnosis, number of embryos transferred or number of > previous ART failures. > > Conclusions: IVIG treatment was associated with improved IVF outcome > in NKa+ patients with prior unexplained IVF failure. Among NKa+ > patients treated with IVIG, 63% conceived an on-going gestation, > while only 1 pregnancy (4%) occurred among the 22 NKa+ patients who > declined IVIG treatment. While these findings are retrospective and > should not be used to draw definitive conclusions, these data support > the ideas that immunologic factors can negatively impact IVF outcome > and that selective immunotherapy with IVIG can mitigate those > effects. A randomized controlled trial is currently under way atv > SIRM to directly and definitively assess the effect of IVIG therapy > on IVF outcome in NKa+ patients. > > > > ---------------------> > 8) > > > > Am J Reprod Immunol 1998 Feb;39(2):82-8 > > > > Prevention of unexplained recurrent spontaneous abortion using > intravenous immunoglobulin: a prospective, randomized, double> blinded, placebo-controlled trial. > > Stephenson MD, Dreher K, Houlihan E, Wu V. > > Department of Obstetrics and Gynaecology, Faculty of Medicine, > University of British Columbia, Vancouver, Canada. > > PROBLEM: The efficacy of intravenous immunoglobulin (IVIG) for > treatment of unexplained recurrent spontaneous abortion was assessed > in a prospective, randomized, double-blinded, and placebocontrolled > study. METHOD OF STUDY: The study took place in a provincial > recurrent pregnancy loss clinic, located in a tertiary/quaternary > care academic center. The study subjects were women with a history of > two or more documented consecutive spontaneous pregnancy losses under > 20 weeks of gestation, excluding any associated with aneuploidy by > karyotype analysis, and with no evidence of genetic, endocrine, > infectious, anatomic, or autoimmune factors associated with a history > of recurrent spontaneous abortion. The subjects were randomized to > receive either intravenous immunoglobulin (Gamimune N) as treatment > or normal saline as placebo. Randomization was stratified for > primary, secondary, and unclassified unexplained recurrent > spontaneous abortion. Success was defined as an ongoing pregnancy > beyond 20 weeks of gestation. RESULTS: Sixty-two subjects enrolled in > the trial. There were 37 index pregnancies and 6 cross-over > pregnancies. There was no clinically significant difference between > the treatment arm and the placebo arm in terms of subsequent > pregnancy success. There seemed to be a higher success rate with the > stratified analysis of couples with secondary unexplained recurrent > spontaneous abortion, but the trial did not have sufficient power to > confirm this. CONCLUSIONS: Based on this trial and three similar > trials in the literature, a multicentered trial is needed to > determine conclusively whether IVIG is effective in the treatment of > unexplained recurrent spontaneous abortion. > > Publication Types: > Clinical Trial > Randomized Controlled Trial > > PMID: 9506206 [PubMed - indexed for MEDLINE] > ----------------------------> > 9) > > American Journal Of Reproductive Immunology > Volume 49 Issue 1 Page 21 - January 2003 > > Effect of Intravenous Immunoglobulin Treatment on the Th1/Th2 Balance > in Women with Recurrent Spontaneous Abortions > > Olga Graphou, Athanasia Chioti, Ageliki Pantazi, Christina Tsekoura, > Virginia Kontopoulou, Eleftheria Georgiadou, Christos Balafoutas, > Stavros Koussoulakos, Loukas H. Margaritis, and Marighoula Varla> Leftherioti > > > PROBLEM: The way by which intravenous immunoglobulin (IvIg) acts to > prevent immunlogically mediated recurrent spontaneous abortions (RSA) > has not been clarified. In the present study, a possible effect of > IvIg on the T helper cell (Th1/Th2) balance was investigated in > abortions of either alloimmune or autoimmune abnormalities. > > METHOD OF STUDY: The study included 21 women treated with IvIg before > conception because of a history of RSA characterized by alloimmune > abnormalities (n = 15) or associated with anti-phospholipid > antibodies (APA) (n = 6). Peripheral blood samples, collected before > and 5 days after the first IvIg infusion, were stimulated, and Th1 > and Th2 cells were detected by flow-cytometric analysis using a > combination of monoclonal antibodies against T-cell surface markers > and intracellular interferon (IFN)- and interleukin (IL)-4. The > percentage of IFN--producing (Th1) and IL-4-producing (Th2) cells and > the Th1/Th2 ratio were compared between pre- and post-infusion > samples. > > RESULTS: A decrease of Th1 percentage in 66.6% of the cases and a > concurrent Th2 percentage increase (47.61%) resulted in a decrease in > the Th1/Th2 ratio in most of the cases (76.1%) (p < 0.01). Similar > results were found in Group A (Th1/Th2 decreased in 60% of the cases, > p < 0.05), while in Group B the effect of IvIg was not clear (Th1/Th2 > increased in three and decreased in another three cases). > > CONCLUSION: Our finding suggests that IvIg administration in women > with alloimmune RSA enhances Th2 polarization. This is not always the > case with APA-associated abortions. > > ------------------------> > 10) > > American Journal Of Reproductive Immunology > Volume 49 Issue 2 Page 84 - February 2003 > > Intravenous Immunoglobulin Treatment in Women with Recurrent > Abortions: Increased Cytokine Levels and Reduced Th1/ Th2 Lymphocyte > Ratio in Peripheral Blood > > Hideto Yamada, Mamoru Morikawa, Itsuko Furuta, Emi H. Kato, Shigeki > Shimada, Kazuya Iwabuchi, and Hisanori Minakami > > PROBLEM: The aim of this study was to investigate changes in > peripheral blood Th1/Th2 cytokine levels and lymphocyte ratios after > massive intravenous immunoglobulin (MIVIg) treatment for women with > recurrent spontaneous abortion (RSA) of unexplained etiology. > > METHOD OF STUDY: Serum Th1 (IFN-, TNF-) and Th2 cytokine (IL-4, IL> 10) levels were assessed by ELISA methods (n = 9) and peripheral > blood Th1/Th2 lymphocyte ratios (n = 4) by flow cytometry before and > after MIVIg treatments in women with four or more consecutive RSA. > > RESULTS: Pre-treatment serum IFN- (0.06 ± 0.09 pg/mL, mean ± SD), TNF> (0.21 ± 0.45 pg/mL), IL-4 (0.70 ± 1.16 pg/mL), and IL-10 (1.12 ± > 1.67 pg/mL) increased to 0.17 ± 0.16 pg/mL, 0.77 ± 0.28 pg/mL, 1.82 ± > 0.89 pg/mL, and 3.44 ± 0.48 pg/mL, respectively, after MIVIg > treatments (P < 0.05). CD4-positive IFN-/IL-4 lymphocyte ratios (17.3 > ± 9.1) were reduced to 11.5 ± 7.1 after treatment (P < 0.05). > > CONCLUSIONS: Massive intravenous immunoglobulin treatments increased > peripheral blood cytokine levels and decreased Th1/Th2 lymphocyte > ratios; thus, MIVIg treatments modify the peripheral Th1/Th2 balance. > > ----------------------------------------------- > > Articles with full text links: > > ---------------------------------> > 11) Immunoglobulin G Infusion Treatment For Women With Recurrent > Spontaneous Abortions And Elevated CD56+ Natural Killer Cells > > http://www.earlypregnancy.org/EPBM/EPBM%20IV/Vol.%20IV,%20Num% > 202/EPBM1288.htm > > 12) The Selective Use of Heparin/Aspirin Therapy, alone or in > Combination with Intravenous Immunoglobulin G, in the Management of > Antiphospholipid Antibody-Positive Women Undergoing In Vitro > Fertilization > > http://www.rialab.com/docum/select.pdf > > 13) The Use of Combined Heparin/Apirin and Immunoglobulin G Therapy > in the Treatment of In Vitro Fertilization Patients With Antithyroid > Antibodies. > > http://www.rialab.com/docum/use.pdf > > 14). A Rational Basis for the Use of Combined Heparin/Aspirin and > IVIG Immunotherapy in the Treatment of Recurrent IVF Failure > Associated with Antiphospholipid Antibodies > > http://www.rialab.com/docum/ration.pdf > > 15) Intravenous Immunoglobulin for Recurrent Pregnancy Loss (a > prospective randomized, placebo-controlled clinical trial) > http://www.inciid.org/article.php?cat=miscarriage&id=19 > > 16) Intravenous Immunoglobulin (IVIG) Therapy for Immunologic Abortion > (Clinical and Applied Immunology Reviews 2 (2002) 187-199, PDF 93K) > > http://www.rialab.com/docum/cair_ivig.pdf > > ---------------------------> > > > 17) Ginekol Pol. 2003 May;74(5):350-5 > [Application of intravenous immunoglobulin therapy (IVIG) in pregnant > patients with recurrent spontaneous abortions] > > [Article in Polish] > > Sipak-Szmigiel O, Ronin-Walknowska E, Miklaszwicz A. > > Kliniki Patologii Ciazy i Porodu Pomorskiej Akademii Medycznej, > Szczecinie. > > OBJECTIVE: Clinical outcome of pregnancy in patients with recurrent > pregnancy losses treated with IVIG during their current pregnancy. > MATERIAL AND METHODS: The study group consisted of 10 pregnant women > with 3-5 spontaneous abortions. Any genetic, anatomical or infectious > abnormalities were excluded as well as antiphospholipid antibody > syndrome and negative lymphocytotoxic test. The treatment consisted > of passive immunotherapy by means of intravenous administration of > immunoglobulin (IVIG) at a dose of 0.4 g/kg b.w. Therapy was > commenced at week 5-6 of gestation, infusions were repeated every 3-4 > weeks until 28th week of gestation in 5-, 3- and 1-day protocols. In > 2 patients that therapy followed active immunotherapy with paternal > lymphocytes. RESULTS: Eight (80%) patients bore healthy babies (3 > preterm); in 2 cases embryos died at 6-7 week of gestation. > CONCLUSIONS: The results confirm the efficacy of IVIG in pregnant > patients with recurrent spontaneous abortions in whom likelihood of > immunological pattern of pregnancy failures is high. > > PMID: 12931461 [PubMed - indexed for MEDLINE] > --------------------> 18) Am J Reprod Immunol. 2003 Feb;49(2):84-9. > > Intravenous immunoglobulin treatment in women with recurrent > abortions: increased cytokine levels and reduced Th1/Th2 lymphocyte > ratio in peripheral blood. > > Yamada H, Morikawa M, Furuta I, Kato EH, Shimada S, Iwabuchi K, > Minakami H. > > Department of Obstetrics and Gynecology, Hokkaido University Graduate > School of Medicine, Sapporo, Japan. yhideto@m... > > PROBLEM: The aim of this study was to investigate changes in > peripheral blood Th1/Th2 cytokine levels and lymphocyte ratios after > massive intravenous immunoglobulin (MIVIg) treatment for women with > recurrent spontaneous abortion (RSA) of unexplained etiology. METHOD > OF STUDY: Serum Th1 (IFN-gamma, TNF-alpha) and Th2 cytokine (IL-4, IL> 10) levels were assessed by ELISA methods (n = 9) and peripheral > blood Th1/Th2 lymphocyte ratios (n = 4) by flow cytometry before and > after MIVIg treatments in women with four or more consecutive RSA. > RESULTS: Pre-treatment serum IFN-gamma (0.06 +/- 0.09 pg/mL, mean +/> SD), TNF-alpha (0.21 +/- 0.45 pg/mL), IL-4 (0.70 +/- 1.16 pg/mL), and > IL-10 (1.12 +/- 1.67 pg/mL) increased to 0.17 +/- 0.16 pg/mL, 0.77 +/> 0.28 pg/mL, 1.82 +/- 0.89 pg/mL, and 3.44 +/- 0.48 pg/mL, > respectively, after MIVIg treatments (P < 0.05). CD4-positive IFN> gamma/IL-4 lymphocyte ratios (17.3 +/- 9.1) were reduced to 11.5 +/> 7.1 after treatment (P < 0.05). CONCLUSIONS: Massive intravenous > immunoglobulin treatments increased peripheral blood cytokine levels > and decreased Th1/Th2 lymphocyte ratios; thus, MIVIg treatments > modify the peripheral Th1/Th2 balance. > > PMID: 12765346 [PubMed - indexed for MEDLINE] > ------------------> 19) Am J Reprod Immunol. 2003 Jan;49(1):21-9. > > > > > Effect of intravenous immunoglobulin treatment on the Th1/Th2 balance > in women with recurrent spontaneous abortions. > > Graphou O, Chioti A, Pantazi A, Tsukoura C, Kontopoulou V, Guorgiadou > E, Balafoutas C, Koussoulakos S, Margaritis LH, Varla-Leftherioti M. > > Department of Biology, Section of Cell Biology and Biophysics, > National & Kapodistrian University of Athens, Athens, Greece. > > PROBLEM: The way by which intravenous immunoglobulin (IvIg) acts to > prevent immunlogically mediated recurrent spontaneous abortions (RSA) > has not been clarified. In the present study, a possible effect of > IvIg on the T helper cell (Th1/Th2) balance was investigated in > abortions of either alloimmune or autoimmune abnormalities. METHOD OF > STUDY: The study included 21 women treated with IvIg before > conception because of a history of RSA characterized by alloimmune > abnormalities (n = 15) or associated with anti-phospholipid > antibodies (APA) (n = 6). Peripheral blood samples, collected before > and 5 days after the first IvIg infusion, were stimulated, and Th1 > and Th2 cells were detected by flow-cytometric analysis using a > combination of monoclonal antibodies against T-cell surface markers > and intracellular interferon (IFN)-gamma and interleukin (IL)-4. The > percentage of IFN-gamma-producing (Th1) and IL-4-producing (Th2) > cells and the Th1/Th2 ratio were compared between pre- and post> infusion samples. RESULTS: A decrease of Th1 percentage in 66.6% of > the cases and a concurrent Th2 percentage increase (47.61%) resulted > in a decrease in the Th1/Th2 ratio in most of the cases (76.1%) (p < > 0.01). Similar results were found in Group A (Th1/Th2 decreased in > 60% of the cases, p < 0.05), while in Group B the effect of IvIg was > not clear (Th1/Th2 increased in three and decreased in another three > cases). CONCLUSION: Our finding suggests that IvIg administration in > women with alloimmune RSA enhances Th2 polarization. This is not > always the case with APA-associated abortions. > > PMID: 12733591 [PubMed - indexed for MEDLINE] > ------------------------> 20) Am J Reprod Immunol. 2002 Nov;48(5):312-8. > T and B lymphocyte subsets in patients with unexplained recurrent > spontaneous abortion: IVIG versus placebo treatment. > > Jablonowska B, Palfi M, Matthiesen L, Selbing A, Kjellberg S, > Ernerudh J. > > Division of Obstetrics and Gynecology, Department of Health and > Environment, University Hospital, Linkoping, Sweden. > barbara.jablonowska@l... > > PROBLEM: To investigate circulating lymphocyte subsets in women with > recurrent spontaneous abortion (RSA) in relation to pregnancy outcome > and to treatment with intravenous immunoglobulin (IVIG). METHOD OF > STUDY: Forty-one women with a history of unexplained RSA were > examined during first trimester of pregnancy before IVIG or placebo > treatment and after pregnancy. The results were compared with five > healthy, non-pregnant women and five women in the first trimester of > normal pregnancy. Circulating lymphocyte subsets with focus on Tcell > subpopulations were determined by flow cytometry. RESULTS: The > proportions of human leukocyte antigen (HLA)-DR positive T cells > (CD3+ HLA-DR+), T-killer/effector cells (CD8+ S6F1+) and B cells > (CD19+) were increased, whereas the proportion of T> suppressor/inducer cells (CD4+ CD45RA+) was decreased during first > trimester pregnancy of RSA women compared with pregnant normal > controls. T and B lymphocyte subsets did not correlate with pregnancy > outcome on either IVIG or placebo group. CONCLUSIONS: In RSA > patients, the immune system seems to be activated in contrast to the > suppression noted in normal pregnancy. > ----------------------------------> 21) Eur J Obstet Gynecol Reprod Biol. 2003 Jul 1;109(1):21-6. > > Live birth rate varies with gestational history and etiology in women > experiencing recurrent spontaneous abortion. > > Morikawa M, Yamada H, Kato EH, Shimada S, Sakuragi N, Fujimoto S, > Minakami H. > > Department of Obstetrics and Gynecology, Hokkaido University Graduate > School of Medicine, Kita-ku N15 W7, Sapporo 060 8638, Japan. > > OBJECTIVES: The aims of this study were to assess pregnancy outcome > in relation to etiologic factors of recurrent spontaneous abortion > (RSA). STUDY DESIGN: The pregnancies from consecutive 216 RSA women > were assessed for live birth rates (LBR) according to etiology. The > LBR in 110 pregnancies from RSA women with unexplained etiology was > investigated according to various therapies. An attempt to karyotype > the abortuses was made. RESULTS: Excluding pregnancies ending in > abortion with abnormal karyotype, the LBR in primary recurrent > spontaneous aborters (68.8%) who experienced three or more abortions > was significantly lower than that in primary repeated aborters > (82.4%) who experienced two abortions. The LBR ranged from 50 to 100% > according to the etiology. In RSA women with unexplained etiology, > the LBR in those undergoing massive intravenous immunoglobulin > (MIVIg) therapy (100%) was significantly higher than those with low > dose aspirin (57.1%) and luteal support therapy (67.3%). CONCLUSIONS: > Excluding pregnancies ending in abortion with abnormal karyotype, we > found that LBR varied with abortion history and etiologic factors of > RSA. > > PMID: 12818438 [PubMed - indexed for MEDLINE] > ------------------> 22) Early Pregnancy. 2000 Apr;4(2):90-8. > > > > > Increased pregnancy rates after IVF/ET with intravenous > immunoglobulin treatment in women with elevated circulating C56+ > cells. > > Coulam CB, Goodman C. > > The Center for Human Reproduction, 750 N. Orleans St., Chicago, IL > 60610, USA. > > Intravenous (IV) immunoglobulin (Ig) has been previously shown to > increase pregnancy rates after previously failed in vitro > fertilization (IVF) embryo (ET) attempts in women who are efficient > embryo producers (fertilize at least 50% of oocytes retrieved and > generate at least 3 embryos/cycle). Women experiencing implantation > failure have a higher frequency of elevated percentage of circulating > CD56+ (natural killer) cells (>12%) than fertile women (3-12%). To > evaluate the effects of IVIg on pregnancy rates in women with > elevated percentage of circulating CD56+ cells, 32 women who had > previously failed IVF/ET (>12 embryos transferred without pregnancy) > were studied. Pregnancy and live birth rates with and without IVIg > were compared in the same woman. All 32 women had previously failed > to conceive after at least 12 ET, were efficient embryo producers and > had persistently elevated plasma concentrations of CD56+ cells. Each > woman received IVIg 500mg/kg prior to ET. If serum hCG concentrations > were positive for pregnancy, IVIg was continued at 500mg/kg/mo until > 28 weeks gestation. Pregnancy rates with and without IVIg were 56% > and 9% (P<0.0001). The rate of live birth was 38% with IVIg and 0% > without IVIg (P<0.0001). IVIg enhances pregnancy and live birth rates > in women with elevated circulating CD56+ cells who have a history of > implantation failure. Despite technologic advances leading to > enhancement of fertilization rates after in vitro fertilization (IVF) > (1, 2) implantation rates after embryo transfer (ET) have not > increased significantly (3) over the last 20 years (4). Implantation > rates after IVF/ET are influenced by the quality of the embryos and > receptivity of the endometrium (3-9). Endometrial receptivity > involves both hormonal (10-13) and immunologic (14-29) factors. Among > the immunologic factors that play a crucial role in successful > implantation are natural killer (NK) cells (14-18). NK cells present > within the decidua that express CD56(but lack CD 16) have been > associated with successful implantation (14-18). A deficiency of > decidual CD56+ CD16- cells (18) and an increase in circulating CD56+ > cells (25, 26) have been observed in women experiencing implantation > failure. Women experiencing implantation failure after IVF and > multiple ET have been successfully treated with intravenous (IV) > immunoglobulin (Ig) (27). IVIg reduces activation of NK cells and NK > killing activity both in vitro (29) and in vivo (30-31). This > reduction in activation of NK cells is essential for normal > implantation to occur (14). To further define the role of IVIg for > treatment of implantation failure, pregnancy and live birth rates > were compared before and after IVIg treatment in women undergoing > IVF/ET who had elevated levels of circulating CD56+ cells. > > PMID: 11723539 [PubMed - indexed for MEDLINE] > -----------------------> 23) : Am J Reprod Immunol. 2000 Aug;44(2):121-4. > > > > > Clinical experience with IVIg Rx in patients with prior failed IVF > pregnancies: report of 30 consecutive patients. > > Scher J, Salazar C. > > b.scher@w... > > PROBLEM: This study reviews one practitioner's experience with > intravenous immunoglobulin (IVIg) therapy in the in-vitro > fertilization (IVF) cycles of 30 patients with previous IVF failures. > METHOD OF STUDY: Thirty patients had undergone 82 prior assisted > reproductive technology (ART) cycles (mean 3.9 +/- 2 failed ART > cycles, median 3.0, range 1-8) yielding one term birth, one loss at > 22.5 weeks, and five chemical pregnancies. These patients underwent > comprehensive clinical and laboratory evaluation, including > immunologic workup, and were accepted for IVIg therapy in their next > IVF cycle. RESULTS: A total of 40 cycles were treated. Twenty-four > (60%) of the IVIg-treated IVF cycles showed a positive human > chorionic gonadotropin test. Comparing the IVIg cycles to the > untreated ART cycles, there were no differences in the number of > embryos transferred, fertilized embryos, or eggs. Eighty-six percent > of the cases with confirmed implantation delivered; there was one > chemical pregnancy, one 20-week spontaneous fetal death, and one > trisomy. Five (24%) of the 21 pregnant patients delivered at 30-36 > weeks. The remaining 13 delivered at term. Only three (11%) had no > positive immune test. CONCLUSION: In what may be a selected > population of IVF patients (with high incidence of abnormal immune > testing), early IVIg therapy may be associated with the improved > success of IVF, and the high rate of live birth. > > PMID: 10994640 [PubMed - indexed for MEDLINE] > **************** > > 23) Ginekol Pol. 2003 Oct;74(10):1107-11. > > [Immunotherapy as an effective treatment of recurrent spontaneous > abortion--own experience] > > [Article in Polish] > > Jerzak M, Rechberger T, Baranowski W, Semczuk M. > > Kliniki Poloznictwa i Patologii Ciazy AM w Lublinie. > > OBJECTIVES: Recent data emphasize relationship between > antiphospholipid antibodies (APA) and increased natural killer cell > activity in women with recurrent spontaneous abortion (RSA). > Therefore, it has been proposed that final common mechanism involved > in the pathogenesis of RSA is associated with auto- and alloimmunity. > DESIGN: The aim of this study was to present our data concerning > diagnosis and treatment of women with RSA. MATERIALS AND METHODS: > Sixty nonpregnant women with the history of RSA were studied, among > them 41 were screened at the beginning of their next pregnancy. We > investigated the existence of inherited (deficiencies of protein C, > protein S, antithrombin III, a resistance to the activated protein C> including Leiden V mutation) or acquired thrombophilia (APA> anticardiolipin antibodies, antiphosphatidylserine antibodies, lupus > anticoagulant). Natural killer cell activity was measured using flow > cytometry. In addition, the following lymphocytes surface antigens: > CD3, CD4, CD8, CD16, CD56 were studied using flow cytometry. We also > studied the existence of autoimmunity: antinuclear antibodies (ANA), > antithyroid antibodies (ATA). According to presence of auto- or > alloimmunity, we introduce immunotherapy: intravenous immunoglobulin, > alloimmunization, heparin/aspirin, aspirin alone, steroids or combine > therapy. RESULTS: We determined the existence of thrombophilia in 17 > women, ANA in 5 women, ATA in 5 women, increased number of NK cells > in 16 women and increased NK cell activity in 14 women. Forty-one > women were pregnant and followed up during pregnancy, among them > 33/41 delivered normal healthy baby, 7/41 experienced the next > abortion and 1/41 had ectopic pregnancy. Therefore, overall success > of immunotherapy was 80.5%. CONCLUSIONS: Immunotherapy seems to be > effective treatment for women with the history of RSA and combined > immune abnormalities. Regulation of immune system activity may > underlie possible effect of such therapy. > > PMID: 14669403 [PubMed] > > **************** > > 24) Am J Reprod Immunol. 2003 Sep;50(3):232-7. > > GM-CSF and pregnancy: evidence of significantly reduced blood > concentrations in unexplained recurrent abortion efficiently reverted > by intravenous immunoglobulin treatment. > > Perricone R, De Carolis C, Giacomelli R, Guarino MD, De Sanctis G, > Fontana L. > > Department of Internal Medicine, University of Rome Tor Vergata, > Rome, Italy. roberto.perricone@u... > > PROBLEM: Certain Th-2 cytokines and granulocyte-macrophage colony> stimulating factor (GM-CSF) are propitious for the success of > pregnancy and recurrent spontaneous abortion (RSA) is often > characterized by a failure of Th-2 type responses. These > considerations as well as the use of intravenous immunoglobulin > (IVIg) in RSA induced us to evaluate the levels of GM-CSF in normal > pregnancies, in pregnant women affected with unexplained RSA and the > effects of IVIg treatment. METHOD OF STUDY: Peripheral blood free GM> CSF was measured by means of a sandwich enzyme immunoassay in 39 > healthy women (13 non-pregnant, 26 pregnant) and in 53 RSA patients > (11 non-pregnant, 42 pregnant). In 14 pregnant RSA patients GM-CSF > was studied also after the very first IVIg infusion (0.5 g/kg body > weight). RESULTS: In healthy women we found a significant increase of > GM-CSF during pregnancy, in pregnant RSA patients such an increase > was not detected. After IVIg, GM-CSF concentrations were almost > doubled. CONCLUSIONS: GM-CSF is found increased in normal pregnancy > and is very low during pregnancy in RSA. IVIg infusions are capable > of increasing GM-CSF in pregnant recurrent aborters. > > PMID: 14629028 [PubMed] > > *************** > > 25) Akush Ginekol (Sofiia). 2004;43(2):3-10. > > > [Effect of intravenous gamma-globulin therapy on lymphocyte > population in pregnant women with antiphospholipid antibodies] > > [Article in Bulgarian] > > Konova E, Ivanova I, Petrova P, Popov I, Andreeva Kh, Lukanov Ts, > Gecheva S. > > The aim of the study was to establish the distribution of the > lymphocyte populations in peripheral blood in pregnant women with > antiphospholipid antibodies (aPL) and a history of recurrent > pregnancy loss as well as to make a study on the influence of the > intravenous IgG-treatment (IVIg) on the levels of antibodies and > peripheral lymphocytes. MATERIALS AND METHODS: 14 pregnant women were > investigated. The latter had two or more recurrent abortions and > positive aPL--anticardiolipin (aCL) and/or anti-beta 2Glycoprotein I > (anti-beta 2-GPI). The lymphocyte populations were examined, using a > flowcytometric method in peripheral blood before 6-7th gestational > week and on the 10-14 day after the second IVIg infusion. 10 pregnant > women wer used as controls who had no aPL antibodies and no pregnancy > loss. RESULTS: 13 out of 14 pregnancies were successful Lymphocyte > populations of the examined patients before the first infusion > compared to the controls showed statistically significant differences > for: T-lymphocyted Th(reduced) and CD3-CD56 + NK (increased) > Significant increase after therapy was noticed for the levels of T> lymphocytes, and Th while the NK-cell populations were significantly > reduced. CONCLUSIONS: aPL-positive pregnancies most probably were > associated with elevated and activated peripheral NK-cell > subpopulations. The low doses of IVIg successfully reduce the levels > of aPL, as well as peripheral CD3-CD56 + NK cells. > > Publication Types: > Clinical Trial > > PMID: 15185522 [PubMed - indexed for MEDLINE] > ************************