Efficacy of immunoglobulin plus prednisolone for prevention of
advertisement

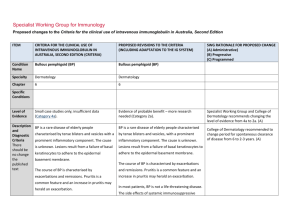
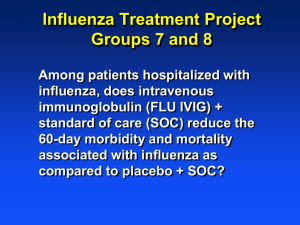
SCH Journal Club Immunoglobulin plus prednisolone in severe Kawaski disease (RAISE study) Steph Borg 22 November 2012 Aim • To assess the efficacy of primary prednisolone treatment as an addition to conventional treatment with intravenous immunoglobulin The Clinical Question Population Patients with Kawasaki’s disease Intervention IV immunoglobulin plus prednisolone Comparison IV immunoglobulin Outcome Reduce incidence of coronary artery abnormalities Design Randomised, controlled, non blinded trial Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawaski disease (RAISE study): a randomised, open label blinded-endpoints trial Kobayahi T, Saji T, Takeuchi et al The Lancet 2012 Vol 379: 1613-20 SCH current practice/guidelines • Immunoglobulin IV 2g/kg within 10days of fever developing – 2nd dose can be given • Aspirin – high dose 80-100mg/kg/day in 4 divided doses until fever settled • Steroids, infliximab and cyclophosphamide can be used in refractory patients in conjunction with rheumatology/immunology Methods • Sep 2008 – Dec 2010 • 74 Japanese hospitals • Diagnostic criteria – – – – – – Fever persisting 5 days or more Bilateral conjunctival congestion Changes of lips and oral cavity Polymorphous exanthema Changes of peripheral extremities Acute non purulent cervical lymphadenopathy • 5 items required for diagnosis Methods • Exclusion criteria – Low risk score, history Kawasaki disease, diagnosed after day 9 of illness, coronary artery abnormalities at diagnosis, other significant medical disorders • Randomly assigned to either IVIG or IVIG + prednisolone • Median duration of prednisolone treatment 21 days Outomes • Primary endpoint – Incidence of coronary artery abnormalities during the study period (Week 1 ,2 ,4) • Secondary endpoints – – – – – – Coronary abnormalities after 4 weeks Z scores of coronary arteries Incidence of need for additional rescue treatment Duration of fever after enrolment CRP at week 1 and week 2 Serious adverse events Are the results valid? • Did the trial address a clearly focussed issue? – Yes • Was the assignment of patients to treatment randomized – Yes • Where all of the patients entered accounted for at its conclusion – Yes Are the results valid? • Where patients, health workers and study personnel blind to treatment – No one blinded except those assessing echos • Where the groups similar at the start of the trial? – Closely matched • Aside from the experimental intervention where the groups treated equally? – Nearly - except no placebo for prednisolone What are the results? • June 2010 – Interim analysis after enrolment of 200th patient • Significant difference in incidence of coronary artery abnormalities between the 2 groups (p<0.0001) • Dec 2010 – Study terminated early Incidence of coronary artery abnormality • During study period – IVIG + Pred 4/121 (3%) – IVIG 28/121 (23%) • risk difference 0.20; CI 0.12-0.28; NNT = 5 • At week 4 – IVIG + Pred 4/120 (3%) – IVIG 15/20 (13%) • Risk difference 0.09; CI 0.02-0.16; NNT = 10 Coronary artery abnormalities • Z-score for proximal right coronary arteries, left main coronary artery, proximal left anterior descending arteries lower in IVIG + prednisolone group at all time points • Fever resolution faster in IVIG + pred vs IVIG group Secondary endpoints • Fever resolution faster in IVIG + pred group • Non response to primary therapy was significantly less in IVIG +pred group • No difference in the rate of relapse between groups Adverse events • In the IVIG + pred group – WCC and HCT higher at week 1,2 and 4 – Neutrophils higher at week 1 and 2 – Cholesterol higher at weeks 1,2 and 4 Serious adverse events • 3/121 IVIG + pred – 2 patients – high total cholesterol – 1 patient - neutropenia • 2/121 IVIG – High total cholesterol – Non-occlusive thrombus left coronary artery Can the results be applied to the local population? • Japanese population • 2 US studies showed no difference between groups – But … used pulsed corticosteroids, single dose Were all clinical important outcomes considered? • Insufficient follow up to assess – – – – – Severe bacterial infection Thrombosis Bone mineral loss Osteonecrosis Ophthalmic power • Insufficient statistical power to exclude adverse events