T cells B cells Site of maturation Thymus Bone marrow
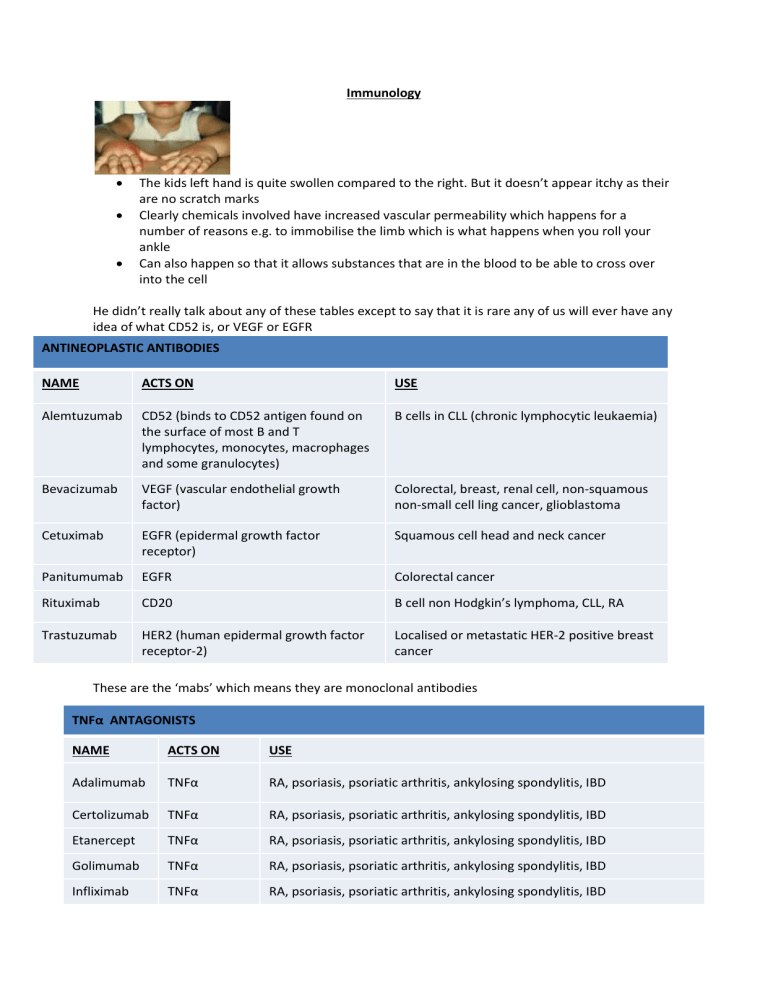
Immunology
The kids left hand is quite swollen compared to the right. But it doesn’t appear itchy as their are no scratch marks
Clearly chemicals involved have increased vascular permeability which happens for a number of reasons e.g. to immobilise the limb which is what happens when you roll your ankle
Can also happen so that it allows substances that are in the blood to be able to cross over into the cell
He didn’t really talk about any of these tables except to say that it is rare any of us will ever have any idea of what CD52 is, or VEGF or EGFR
ANTINEOPLASTIC ANTIBODIES
NAME ACTS ON USE
Alemtuzumab CD52 (binds to CD52 antigen found on the surface of most B and T lymphocytes, monocytes, macrophages and some granulocytes)
Bevacizumab VEGF (vascular endothelial growth factor)
Cetuximab EGFR (epidermal growth factor receptor)
Panitumumab EGFR
Rituximab CD20
B cells in CLL (chronic lymphocytic leukaemia)
Colorectal, breast, renal cell, non-squamous non-small cell ling cancer, glioblastoma
Squamous cell head and neck cancer
Colorectal cancer
B cell non Hodgkin’s lymphoma, CLL, RA
Trastuzumab HER2 (human epidermal growth factor receptor-2)
Localised or metastatic HER-2 positive breast cancer
These are the ‘mabs’ which means they are monoclonal antibodies
TNFα ANTAGONISTS
NAME ACTS ON
Adalimumab TNFα
Certolizumab TNFα
Etanercept TNFα
Golimumab TNFα
Infliximab TNFα
USE
RA, psoriasis, psoriatic arthritis, ankylosing spondylitis, IBD
RA, psoriasis, psoriatic arthritis, ankylosing spondylitis, IBD
RA, psoriasis, psoriatic arthritis, ankylosing spondylitis, IBD
RA, psoriasis, psoriatic arthritis, ankylosing spondylitis, IBD
RA, psoriasis, psoriatic arthritis, ankylosing spondylitis, IBD
CYTOKINE MODULATORS
NAME
Abatacept
ACTS ON
Co-stimulation modulator.
CD80, CD86
USE
Difficult to control RA
Anakinra IL-1 Difficult to control RA
Rituximab
Reduces B lymphocyte induced T cell activation
Tocilizumab IL-6
Difficult to control RA
Difficult to control RA
Immunology
Vaccination – to provide protective immunity by inducing a memory response to an infectious microbe using a non-toxic antigen o Most effective, safe, cost effective advances in medicine
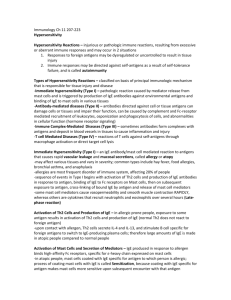
Hypersensitivity
Autoimmunity – an acquired immune reactivity to self antigens tissue damage o Target organ specific – Type 1 diabetes, hyperthyroidism, IBD o Non target organ specific – SLE, RA, MS, Scleroderma
Transplantation – antibodies and cell-mediated immunity are responsible for graft rejection - so we use medications to stop the rejection of organs
Tumors – Immune responses can develop or be induced to develop. (Monoclonal antibodies are generally not tumor specific. They kill by complement activation, ADCC (antibodydependent cellular cytotoxicity) or phagocytosis)
Immunodeficiency
Congenital (inherited) – complement deficiencies, phagocytic defects, B-cell deficiencies.
These are rare
Secondary /acquired is common
SITE SOURCE
Eyes
Ears
Lacrimal glands (tears)
Sebaceous glands
Mouth Salivary glands
Skin Sweat and sebaceous glands
SUBSTANCES SECRETED
Lysozyme*, IgA and IgG
Oily waxy secretion, fatty acids
Digestive enzymes, lysozyme, IgA and IgG
Lysozyme, Oily secretion and fatty acids
Stomach Gastric juices Digestive enzymes (pepsin, acid (pH 1-2) . PPI’s reduce the ability of these external defences
The immune system has external defences against all sorts of pathogens (against worms, protozoans, fungi, bacteria, viruses (e.g. Polio, flu, HIV) o Lysozyme digests proteoglycans in bacterial cell walls. o NB There are physical defences e.g. Mucosal epithelial cells (If you break that physical defence you can introduce a pathogen), mucociliary escalator (little hairs with a sticky coat of mucous above the trachea. This mucous catches pathogens and the mucous is then brushed upwards to be spat out or swallowed and destroyed by digestive enzymes. Smoking kills these hairs/cilia)
The above table is different ways the immune system protects the body
Immunoglobulins are antibodies which is a protein the body makes
The bone marrow/stem cell is what makes all these cells including, T and B cells, RBC’s, and granulocytes
Granulocytes are cells that contain little granules that contain chemicals, which can then be released
Granulocytes are monocytes – the chemicals released have affects in the body e.g. can call other cells to come help
T cells and B cells make T lymphocytes and antibodies which can send chemicals and other cells to do processes. These two work together to perform various functions
All of these are found in the blood (i.e. antibodies) except T lymphocytes which are found in the cells that’s why it’s called cell-mediated immunity
Important to the immune system – T lymphocytes, the antibodies and the granulocytes
B and T cells
• BONE MARROW - produces all hemopoietic cells
• THYMUS -this gland takes immature T cells and generates antigen specificity
• Spleen – major component of the mononuclear phagocytic system (MPS)
• Lymph nodes – contain B and T lymphocytes. These lymph nodes are all around the body
• In general, free-floating antigens are dealt with through free-floating antibodies, whereas intracellular organisms like viruses or bacteria, which cannot be reached by antibodies, are dealt with through cell mediated immunity (T cells).
Antibodies (made by B cells)
• Antibodies (immunoglobulins) are proteins that bind antigen
• The different immunoglobulins:
• IgG - immunity to most blood borne infectious agents
• IgA – prevents colonisation of mucosal surfaces by pathogens and mediates phagocytosis
• IgM – first antibody produced by an immune response while IgG is being produced
• IgE – hypersensitivity /allergic reactions. There are different types of allergic drug reactions
• Type 1 is IgE e.g. which is a rash from penicillin. An immediate type allergic reactions. IgE is usually found on mast cells which contain lots of inflammatory chemicals in places like the respiratory tract and if they discharge it gives you an asthma attack or hayfever when this occurs in the head. IgE sits on the basophil/mast cell and causes the release
• Type 2 is IgM or IgG. Cytotoxic type – IgM or IgG sit on a RBC or platelet and the body then recognises these as ‘non-self’ so people get anaemia or thrombocytopenia . Not associated with community pharmacy
• Type 3 is IgM or IgG as well. Complex mediated type – there is an antigen in the blood and the antibody complexes with it and as they complex they go around the body to it is complete but this complex may get stuck in a blood vessel and cause inflammation (vasculitis) or cause inflammation in a joint (arthritis)
• Type 4 is cell mediated or t cells (rash that comes after a few weeks of using something).
• Type 1 and 4 are common in community pharmacy
• Maternal IgG crosses the placenta and is present in high levels in the newborn
• IgA is present 1-2 months after birth. IgA in breast milk coats the GIT passive mucosal immunity/protects the surface
• Fetus produces IgM
There are 4 chains – 2 heavy and 2 light
There is a variable region and constant
The Fc part binds to cells such as macrophages or mast cells
The Fab part is the antigen binding region
IgA is on the mucous membrane surface
IgE is on the mast cell and basophils like “a pin on a grenade”
IgM and IgG in the blood
Tissue lymphocytes
The lumen at the top could be the open part of the mouth or intestine
IgA is waiting to interact with an antigen
IGe is also waiting
IgM is a big complex of IgM’s and is ready to bind with many things
IgG is more selective in its binding
IgA is present in breast milk so a baby has a lot of IgA protection
When it binds tightly to neutralise – kind of like holding an aggresive person tightly so they can’t move and then stopping damage
Chemotaxis (broad call for help) or phagocytosis (eat the antigen) is another option
Activation is the last but the immune system also has ways to dampen down its activity
None of the above actions takes place as well in old people as the thymus gland is less effective while the bone marrow is less productive as well
Characteristics of B and T cells
Antibodies are very mobile and move quickly about the body
T cell products are much slower. He must have pointed with his finger in the lecture but I think he was saying that TNF-alpha is produced first than IL-4,5 and 6 after
IL stands for interleukin which are cytokines (chemical that calls for help)
B cells mature into plasma cells and plasma cells make antibodies
Natural (innate) immunity and adaptive immunity
Characteristics Cells Molecules
INNATE immunity
Responds rapidly, has some specificity but no memory
ADAPTIVE immunity
Phagocytes
(PMNs/polymorphonucleus and macrophages), NK/natural killing cells, Mast cells
Slow to start, highly specific, memory .
Kind of like a sniper who must set up his gun and adjust for wind etc
T and B cells
Complement, cytokines, chemokines, acute phase proteins
Antibodies, cytokines, chemokines
Your immune system is interested in the antigen that has been acquired
An analogy is when a person goes into a job interview – person is the antigen.
The persons CV defines what type of worker they are
The CV of the antigen defines its size, its closeness to ‘self’ etc
IgE mediated symptoms cause
• Asthma
• Rhinitis
• Urticaria – terrible itchy rash
• Allergic dermatitis (e.g. atopic*) Atopy is a condition of secreting IgE in response to common environmental allergens
• Food hypersensitivity
• Anaphylaxis
• Stinging insect allergies
• People have enormous amounts of IgE and are highly environmentally reactive and suffer from many of these conditions above. Most likely inherit this trait to produce high amounts of IgE from parents
The early phase response
• Allergen binds to IgE on mast cells, which degranulate and
– Release pre-formed inflammatory mediators
– Synthesize other mediators
• Preformed inflammatory mediators:
Histamine
Tryptase (antihistamines probably not that good against this)
Heparin (or this either)
• Synthesized mediators:
PGD
2
– prostaglandin 2
LTC
4
– leukotriene C4
Inflammatory mediators in type 1 hypersensitivity / IgE hypersensitivity
• Prostaglandins are inflammatory mediators with pharmacologic effects on smooth muscle
• Mast cells produces prostaglandin D2 which causes bronchial constriction
• Mast cells also produce the protein neutrophil chemotactic factor of anaphylaxis (IL-8)
• Mast cells produce tryptase, a major protease which can cause tissue destruction – people with asthma can have tissue destruction
• Leukotrienes are derived from membrane fatty acids. LTB4 is a potent chemotactic factor for
PMNs (which are phagocytes) and macrophages
• All of these are present in asthma and rhinitis
Microbrial products interact with the mast cell
IgE/ allergen also interact
Dead cells (patern recognition receptors) so many different things interact
Therefore mast cells are not just for allergies they are for many problems and when any of these things happen the mast cells releases the chemicals which cause vasodilation, increase vascular permeability, neutrophils to eat microbes
Molecules of the immune system (he skipped over it but said to still read it)
The complement system – over 20 interdependent proteins synthesized by hepatocytes and monocytes. On activation it can initiate acute inflammation, attract neutrophils (= chemotaxis), opsonise (attach to) microbe, and kill
Acute phase proteins (e.g. C-reactive protein) – plasma proteins important in innate defence against microbes and in limiting tissue damage caused by infection, trauma, malignancy and other diseases. Mainly produced in the liver in response to infection or in response to certain cytokines
(e.g. IL-1, IL-6, TNFα)
For dummies
20 year old diagram
1 st dose of antigen goes into the lymph node which creates IgE and this then sits on a mast cell with the Fc in the cell and Fab waiting to interact
2 nd dose cross links the IgE’s and the mast cell discharges
For smart fucks
This is meant to be exactly the same as the diagram above
Have a naive B cell and t helper cell
IgE secreting plasma cell with IgE binding to the mast cell
The allergen cross links the IgE on the mast cell and triggers the release of mediators (listed at the bottom)
Same diagram but more complicated
Cells of the innate and adaptive systems (skipped this as well but still read)
• Phagocytes are “eating” cells of which there are two main types – neutrophils and macrophages
• Neutrophils (or Polymorphonuclear cells) comprise the majority of blood leukocytes. They patrol the body via the bloodstream and are pivotal cells in acute inflammation
• The MONONUCLEAR PHAGOCYTE SYSTEM disposes of microbes and dead body cells e.g.
CELLS LOCATION
Monocytes Bloodstream
Kupffer cells Liver
Microglial cells Brain
Alveolar macrophages Lungs
Natural killer (NK) cells – produced in the bone marrow, found mainly in the circulation, comprise 5-15% of the total lymphocyte fraction, whose main function is to kill virus infected cells and some tumour cells
Mast cells and basophils are granulocytes produced in the bone marrow. Mast cells are found throughout the body in connective tissues close to blood vessels and particularly in the respiratory, genitourinary and gastrointestinal tracts. They both release their granules as a result of e.g. binding of allergen to IgE which sits on their cell surface through its Fc receptor; also as the result some drugs (e.g. opioids, radiocontrast agents)
Molecules of the immune system
• Cytokines signal between cells, inducing growth, chemotaxis and activation of cytotoxicity of immune cells (neutrophils, macrophages, NK cells) and/or regulation of immunity. Many are classified as INTERLEUKINS, as they are primarily produced by and communicate with leukocytes
• TNFα is a cytokine produced by monocytes and T cells. TNFα antagonists (adalimumab, certolizumab, etanercept, golimumab, infliximab) are indicated for rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and plaque psoriasis. Adalimumab is indicated for
Crohns disease, Infliximab for both Crohns Disease and Ulcerative Colitis
• Chemokines are cytokines made by monocytes, macrophages, endothelial cells, platelets, neutrophils, T cells, keratinocytes and fibroblasts. They are primarily involved in chemoattraction of lymphocytes, monocytes and neutrophils. IL-8 is a chemokine, chemoattractant for activation of PMNs (i.e. Neutrophils) and naive T cells
Cell mediated immunity
Characteristic clinical presentations of immunodeficiency
• Humoral (i.e. mediated by antibodies) immunodeficiency. Hypogammaglobulinaemia recurrent sinopulmonary infection (S pneumoniae, H influenzae, Neisseria species). So this is what happens if you have too few antibodies
• Cellular immunodeficiency.
T cell dysfunction infections with viruses (CMV, varicella zoster, herpes simplex), fungi
(candida, aspergillus, crytococcus, histoplasma, pneumocystis), protazoa (toxoplasma, microsporidium, cryptosporidium). This is T cell dysfunction problem
• Combined immunodeficiency.
Natural killer cell dysfunction recurrent herpes virus infection, recurrent papilloma virus
(warts) infection
Phagocyte defects recurrent pyogenic (pus producing) infections, recurrent abscesses
Australian Prescriber 2010; 33(3): 84-7
Investigations for suspected immunodeficiency (what we look for if the things above are
happening)
• Humoral immunodeficiency – IgG, IgA, IgM, FBCC, lymphocyte subsets
• Cellular immunodeficiency – IgG, IgA, IgM, FBCC, lymphocyte subsets, HIV testing if indicated
Atopic dermatitis – immunological abnormalities
• LANGERHANS cells (antigen-presenting cells of the skin) in the affected skin are increased in number and express antigen-specific IgE on their surface.
• T (helper) lymphocytes produce large amounts of interleukin (proteins) which raises serum
IgE and activates B cells and mast cells. This may occur (in part) due to Langerhans cell activity.
RA – biological agents
TNF-alpha antagonists – they bind to TNF-alpha
The names are chosen for a reason as you can see below
ADALIMUMAB
ADA = chosen by manufacturer
LIM = for immune and inflammatory diseases
U = human
MAB = monoclonal antibody
INFLIXIMAB
INF = chosen by manufacturer
LI = for immune and inflammatory diseases
XI = chimeric
MAB = monoclonal antibody
HPA axis
• Glucocorticoids damp down immune (inflammatory) responses
• Glucocorticoids are anti-inflammatory
• Inhibit release of IL-1, IL-2, IL-6, IFN-gamma, TNF-alpha by dendritic cells and macrophages; they also inhibit mast cell function
• They are potent anti inflammatories made by the body
RA – immunology
“mAbs to human targets are generated either in other species – for example, in mice – or through recombinant engineering. With chimeric mAbs, the variable region of a murine/mouse-derived mAb is fused to the Fc piece of a human IgG molecule. The resulting construct is approximately one quarter murine and three quarters human.”
(Recombinant engineering – the use of viruses or yeast to create antibodies rather than mice)
Completely skipped this part
• Immune system cells originate from stem cells of the bone marrow
• They differentiate into lymphocyte stem cells or myeloid stem cells
• Lymphocyte stem cells produce T lymphocytes and B lymphocytes
• Myeloid cells produce granulocytes (neutrophils, eosinophils, basophils, mast cells, monocytes and macrophages – the last 2 cell types producing the cytokines TNF, IL-1 and IL-
6)
• T lymphcytes bind to the antigen directly, through their surface receptors (i.e. CD (“cluster of differentiation”) receptors).
• T lymphocytes, monocytes and macrophages contribute to immunological responses through release of cytokines
• B lymphocytes produce immunoglobulins or antibodies (i.e. IgG, IgA, IgM, IgD, IgE)
• An antibody molecule is Y-shaped. The stem of the Y = Fc fragment. It binds to the cell surface receptor
• The two forks = Fab ( ab = antigen binding) fragments
• B lymphocytes are thought to play a pathogenic role in RA by producing autoantibodies (i.e. rheumatoid factor, anticyclic citrullinated protein)
• IL-6 is a multifunctional cytokine that is involved in the acute inflammatory response. It induces the development of B cells, osteoclastogenesis, and acute phase proteins production in the liver. High levels of Il-6 have been found in the synovial fluids from inflamed joints of patients with RA
O is mouse
U is human
Xi is chimeric – bit of mouse and a bit of human – the more human it is the less you will react
RA – TNF (skipped this too)
• TNF is a proinflammatory cytokine in RA, psoriatic arthritis, and ankylosing spondylitis
• TNF activates various cell types, promotes accumulation of immunocompetent cells at sites of inflammation by activation of the vascular endothelium, and stimulates synthesis of other pro-inflammatory cytokines (e.g. IL-1, IL-6)
• Both TNF and IL-1 mediate bone and cartilage destruction through activation of osteoclasts and macrophages to release destructive mediators (collagenase, prostaglandins)
Cytokine modulators (skipped this too)
• ANAKINRA is a recombinant Il-1ra (ra = receptor antagonist).
• TOCILIZUMAB is a humanised anti IL-6 receptor mAB that binds to both soluble and membrane-bound IL-6 receptor
• ABATACEPT is a soluble protein consisting of the extracellular domain of CTLA-4 (cytotoxic T lymphocyte-associated antigen 4) linked to the Fc portion of IgG1
He said for the exam he just wants us to understand the principles, don’t need to know the fine details. Know the GENERAL purpose of things