External regulation of immune response
advertisement
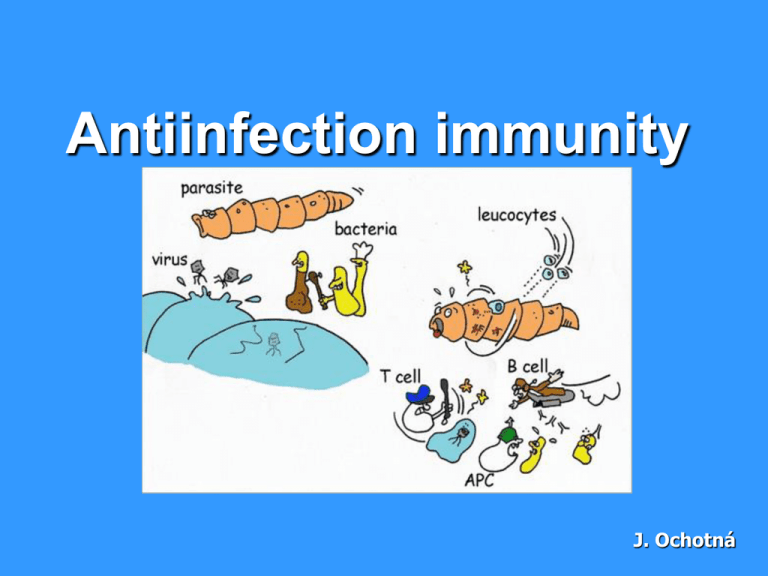
Antiinfection immunity J. Ochotná Defence against extracellular pathogens Defence against extracellular pathogens bacteria (gram-negative, gram-positive cocci, bacilli), unicellular parasites for their elimination is necessary opsonization (C3b, lectins, antibodies ...) neutrophilic granulocytes are chemotactic attracting to the site of the infection (C5a, C3a and chemotactic products of bacteria) absorbed bacteria are destroyed by the microbicidal systems (products of NADP-H oxidase, hydrolytic enzymes and bactericidal substances in lysosomes) phagocytes produce proinflammatory cytokines (IL-1, IL-6, TNF) that induce an increase in temperature, metabolic response of the organism and synthesis of acute phase proteins in later stages of infection are stimulated antigen-specific mechanisms plasma cells initially produce IgM isotype after isotype switching produce IgG1 and IgA (opsonization) sIgA protect against intestinal and respiratory infections by bacteria bacteria with a polysaccharide capsule may cause T-independent IgM antibody production (after the establishment to the bacteria activate the classical complement path) after infection persist IgG, IgA (protective effect) and memory T and B lymphocytes in the defense against bacterial toxins apply neutralizing antibodies (Clostridium tetani and botulinum ...) "indirect toxins - bacterial Lipopolysaccharide (LPS) stimulates big number of monocytes to release TNF, which can cause septic shock extracellular bacterial infections are especially at risk individuals with disorders in the function of phagocytes, complement and antibody production Defence against intracellular pathogens Defense against intracellular pathogens bacteria, fungi and unicellular parasites intracellular parasites are resistant to the microbicidal mechanisms of phagocytes macrophages, which absorbed them, produce IL-12 → TH1 differentiation, production of IFNg and membrane TNF → activation of macrophages and induction of iNOS plasma cells under the influence of IFNg produce IgG2, immune complexes containing IgG2 bind to Fc receptors on macrophages and thus stimulate them - in the defense against intracelular parasites, which escape from phagolysosomes apply TC lymphocytes intracellular microorganisms infections are at risk individuals with certain disorders of phagocytes and defects of T lymphocytes Defense against intracellular pathogens Anti-viral defence Anti-viral defence interferons - in infected cells is induced production of IFNa and IFNb (prevents viral replication and in uninfected cells cause the anti-virus status); IFNg stimulates the conversion to activated macrophages (iNOS) NK cells - ADCC (Antibody-dependent cell-mediated cytotoxicity) = cytotoxic reaction depends on the antibodies; the NK-lymphocyte recognizes cell opsonized with IgG by stimulation Fc receptor CD16 and then activate cytotoxic mechanisms (degranulation) infected macrophages produce IL-12 (a strong activator of NK cells) in the defense against cytopathic viruses mostly applied antibodies: sIgA inhibit mucosal adhesion of viruses (defense against respiratory viruses and enteroviruses) neutralizing IgG and IgM antibodies activate the classical way of complement, which is capable of some viruses lysis IgA and IgG derived in viral infection have a preventive effect in secondary infection effector TC lymphocytes destroy infected cells in direct contact (granzym/perforin; FasL) and by produced cytokines (lymfotoxin) some viruses after infection integrate into the host genome, where persist for years (varicella zoster, EBV, papillomavirus) by these infections are at risk individuals with T lymphocyte immunodeficiency and with combined immune disorders increased susceptibility to herpes infections in individuals with dysfunction of NK cells Defense against parasites Defense against protozoa parasites Toxoplasma gondii, Leishmania, Trypanosoma defense against protozoa parasites is similar to bacteria extracellular parasites - antibodies intracellular parasites - TH1 lymphocytes and activated macrophages Defense against multicellular parasites Defense against multicellular parasites contact of mast cells, basophils and eosinophils with parasite antigens TH2 stimulation under the influence of IL-4 (mast cells and other APC stimulated by parasite) TH2 stimulate B cells with BCR-specific parasite antigens isotype switching under the influence of IL-4 to IgE IgE bind to FceRI on mast cells and basophils („antigenspecific receptors“) establish of multivalent antigen (multicellular parasite) using the IgE to highafinity Fc receptor for IgE (FceRI) aggregation of several molecules FceRI initiate mast cell degranulation (cytoplasmic granules mergers with the surface membrane and release their contents) activation of arachidonic acid metabolism (leukotriene C4, prostaglandin PGD2) - amplification of inflammatory responses cytokine production by mast cell (TNF, TGFb, IL-4, 5,6 ...) in later stages are activated TH1 and are produced antibodies of other classes eosinophils fagocyte complexes of parasitic particles with IgE via their receptors for IgE eosinophils use against parasites extracellular bactericidal substances released from granules (eosinophil cationic protein, protease) Activation of mast cell External regulation of immune response Causal treatment a) Stem cell transplantation for serious congenital disorders of the immune system and some lymphoproliferative and myeloproliferative disorders complications: infectious complications Graft-versus-host disease obtaining stem cells - collection from shovel hip bone - from umbilical cord blood - from peripheral blood after stimulation with GM-CSF b) Gene therapy with a suitable expression vector is introduced functional gene (to replace dysfunctional gen) into the lymphocytes or stem cells used as a treatment for some cases of SCID Substitution treatment autologous stem cell transplantation following chemotherapy and radiotherapy treatment with intravenous immunoglobulin (derived from plasma of blood donors) substitution of C1 inhibitor for hereditary angioedema substitution of erythropoietin in patients with chronic renal failure substitution of G-CSF in agranulocytosis Immunomodulation = medical procedure to adjust the disrupted immune function Non-specific immunosuppressive therapy nonspecific = affects not only autoreactive and aloreactive lymphocytes, but also other components of immunity (risk of reduction antiinfectious and antitumor immunity) used for treatment of autoimmune diseases, severe allergic conditions and for organ transplantation Non-specific immunosuppressive therapy corticosteroids - anti-inflammatory, immunosuppressive effects - blocking the activity of transcription factors (AP-1, NFkB) - suppress the expression of genes (IL-2, IL-1, phospholipase A, MHC gp II, adhesion molecules) - inhibition of histamine release from basophils - higher concentrations induce apoptosis of lymfocytes immunosuppressants affecting the metabolism of DNA - cyclophosphamide (alkylating agent) - methotrexate (antimetabolite) - azathioprine (purine analogue) immunosuppressant selectively inhibiting T lymphocytes - immunosuppressive ATB: cyclosporine A, tacrolimus, rapamycin (suppressing the expression of IL-2 and IL-2R in activated T lymphocytes) - monoclonal antibody anti-CD3 (Immunosuppression after transplantation, treatment of rejection crises) immunoglobulins in the immunosuppressive indication - Polyspecific intravenous immunoglobulins (Inhibition of B lymphocytes, antiidiotype activity, inhibition of cytokines, neutralization of toxins, inhibition of complement activation ...) Anti-inflammatory and antiallergic treatment nonsteroidal anti-inflammatory drugs antihistamines - blocking H1 receptor - reduce the expression of adhesion molecules - reduce the secretion of histamine ... inhibitors of inflammatory cytokine - receptor antagonist for IL-1 - monoclonal antibodies against TNF - thalidomide (TNF inhibitor) enzyme therapy - in the enzyme mixture has a major effect trypsin and bromelain - anti-inflammatory and immunomodulatory effects Non-specific immunostimulant therapy synthetic immunomodulators Methisoprinol (Isoprinosine) - used in viral infections with more severe or relapsing course bacterial extracts and lysates Broncho-Vaxom - prevention of recurrent respiratory tract infections Ribomunyl products of the immune system IL-2 - renal adenocarcinoma IFNa, IFNb - viral hepatitis, some leukemia Erythropoietin – renal failure G-CSF, GM-CSF – neutropenia Transfer factor (blood donors leukocytes undergoing dialysis) Thymus hormones Antigen-specific immunomodulatory therapy specific immunomodulation = induce an immune response or tolerance against a specific antigen a) active immunization = use of antigen to induce an immune response that can later protect against a pathogen bearing the antigen (or similar antigen) immunization vaccines are made from inactivated or attenuated microorganisms or their antigens (polysaccharide capsule, toxins) creates long-term immunity activate cellular and antibody immunity administration of antigen injectable, oral prophylaxis risk of infection or anaphylactic reactions b) passive immunization natural - transfer of maternal antibodies in fetal blood therapeutically - the use of animal antibodies against various toxins (snake toxins, tetanus toxin, botulinum toxin) prophylaxis - the human immunoglobulin from immunized individuals (hepatitis A, rabies, tetanus) - Anti-RhD antibodies - preventing maternal immunization with RhD+ fetus provides a temporary (3 weeks) specific humoral immunity the risk anaphylactic reactions c) specific immunosuppression = induction of tolerance to a specific antigen ongoing clinical studies induction of tolerance by oral administration of antigen (treatment of certain autoimmune diseases) allergen immunotherapy (pollen, insect poisons) d) vaccination against cancer immunization by dendritic cells