If HIS HEAD HAS ENTERED THE PELVIS AND THE MAURICEAU
advertisement

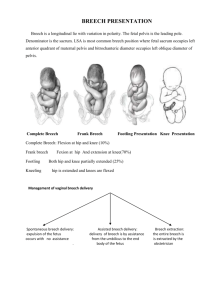
BREECH PRESENTATION CORRECTING A BREECH PRESENTATION EXTERNAL CEPHALIC VERSION can be done at any time after 34 weeks, until labour starts. It is not necessary before 34 weeks. You may not succeed after 36 weeks, but it is still worth trying. Figure 19.2: CORRECTING A BREECH PRESENTATION. A, to C, external cephalic version. Flex him between his hands so that you make him do a forward somersault. D, the knee–chest position. Ask his mother to spend 10 minutes tid like this. Contraindications (1) Multipara. (2) Antepartum bleeding in this pregnancy. (3) A previous Caesarean section. (4) The need to do a Caesarean section in this pregnancy for some other reason. (5) A diastolic blood pressure greater than 100 mm. (5) A detected fetal abnormality. (6) A Rhesus-negative mother and no anti-Rh imunoglobulin to treat her with. Method Explain carefully what you are going to do. Ask her to empty her bladder and lie on her back tilted a little to one side. Make sure your hands are warm and she is comfortable. You may find it helpful to lubricate your hands and her abdomen with glove powder. Find which side the baby’s back is. Count his heart rate. Place one hand below his breech, and your other hand above his head. Flex him between your hands, so that you make him do a forward somersault (turn head over heels). Listen to his heart. If his heart rate slowed to less than 100, turn her on her side and wait until it is more than 100. If his heart rate has not started to recover within 2mins, turn him into his original position. His umbilical cord may be tight round his neck. If a forward somersault fails, try turning him in a backward somersault. If both fail, rest her with the foot of her bed raised. If she is anxious give her diazepam 5 mg by month. Try again in an hour. If you fail again, try again at the next visit. If you succeed, see her again 1wk later to make sure the presentation is still cephalic. If you cannot turn her by 37 weeks, manage her as a breech delivery. INDICATIONS FOR CAESAREAN SECTION IN A BREECH DELIVERY If she has a normal or large pelvis, and he is a normal-sized baby, she will probably deliver vaginally. If you cannot touch her sacral promontory easily, and her diagonal conjugate is >11 cm (true conjugate >9cm), she probably has a large enough pelvis. If you can touch her sacral promontory easily, and her diagonal conjugate is <11 cm, she has a small pelvis. Most additional factors, which compromise the wellbeing of a baby, are indications for section. Only a healthy normal-sized mother with a baby less than 3.7 kg (as indicated by a fundal height of <40 cm), who progresses normally in both stages of labour, should be allowed a vaginal delivery. In more detail the indications for section are these: ANTENATAL INDICATIONS. (1) CPD or suspected CPD. (2) A large baby; feel the size of his head. If he feels as if he is big, that is >3.7 kg (fundal height >40 cm), regardless of the size of her pelvis, do a Caesarean section. (3) The scar from a previous section. (4) Other obstetric hazards, such as placenta praevia, diabetes, gestational hypertension, or APH. (5) An elderly primigravida, or a long history of infertility. (6) A previous stillbirth, especially if it was associated with a breech. (7) Postmaturity >42 weeks. (8) Perhaps a baby with IUGR, or prematurity, weighing 1000–1500 g, especially if he is a footling. INDICATIONS DURING LABOUR. (1) A prolonged active phase. (2) Arrest at the brim, or delay in the descent of the breech during the second stage. (3) A footling presentation. A multipara is likely to develop an irresistible desire to push before full dilatation, as her baby’s feet enter her vagina. This can result in his head being caught behind her undilated cervix. (4) Cord presentation or prolapse. (5) Fetal distress. (6) Prolonged rupture of the membranes. ASSISTED BREECH DELIVERY CAUTION! For breech delivery you need a quiet atmosphere and good communication with the patient. A crowd of supporters crying ‘Push, push’ is not what you want. Quiet them and explain what is happening. You will need an assistant. Figure 19.3: THE BURNS–MARSHALL MANOEUVRE for delivering the head in a breech delivery, if it does not deliver spontaneously. A, allow his body to hang, until you can see the hair at the back of his neck. B, hold his feet. C, swing his feet upwards over his mother’s abdomen. Free his mouth and pause while you clean it. D, finish delivery by swinging him over her abdomen. THE FIRST STAGE. If her cervix dilates at < 1cm/hr in the active phase, or there are any other signs of delay, do a Caesarean section. Until his buttocks are delivered, you can turn back and do a Caesarean section. Only when his buttocks have been delivered have you reached the point of no return. If there is any delay before the delivery of his buttocks, do a Caesarean section. THE SECOND STAGE. A common fault is to try to deliver a breech through an incompletely dilated cervix, which may force his arms to extend and make his head difficult to deliver. Full dilatation may not be easy to diagnose in a breech, so don’t consider that the second stage has started until his anterior buttock is easily visible. Put her into the lithotomy position (essential if you do the Burns Marshall manoeuvre or apply forceps to his aftercoming head) when his posterior buttock is distending her perineum. As soon as she wants to bear down, do a vaginal examination to make sure that her cervix is fully dilated. His breech should advance with every contraction. Infiltrate her perineum, and do an episiotomy, when his buttocks are distending it, and you can see a boy’s scrotum (or a girl’s labia). Protect his scrotum (you don’t want the episiotomy to castrate him!). His buttocks and legs will then deliver. When his umbilicus delivers there is often a temporary halt in descent. Look at the clock. He should be delivered in the next 5 minutes. Wait for progress to resume with the next contraction. His shoulders and arms should deliver with a twisting movement, and his head should follow immediately. Don’t touch him, or try to disentangle his legs, until you see his umbilicus. Touching him promotes breathing movements and the aspiration of meconium. Put your hand on the mother’s fundus, observe each contraction, and keep a steady gentle pressure on his head. When his umbilicus appears, disengage his extended legs and pull down a loop of his cord, which may be stretched. CAUTION! Encourage him to turn so that his back is uppermost. Never allow his ventral surface to face upwards. When his anterior scapula appears (and not before), search for his arms in front of his chest. If, as is usual, his arms are not extended, they will both be in front of his chest. You should be able to deliver one or both of them. If you have difficulty, feel up to his shoulder and from there feel down his arm, first one then other. Allow his body to hang (23-3A). His own weight will make his head descend through her birth canal. It will have been entering her pelvis, and will be compressing his cord. Assist its descent with gentle suprapubic pressure. He must be able to breathe in the next 5 minutes. If his head does not immediately deliver spontaneously when his arms are out, try the BURNS–MARSHALL manoeuvre. Wait until you can see the hairs on the nape of his neck (23-3A). Stand with your back to her left leg, take his legs in your right hand (23-3B), pull him outwards a little and draw him outwards over her pubis. Guard her perineum with your left hand and prevent his head from emerging too quickly. As soon as his mouth and nose appear, pause, and ask your assistant to clear his airways and allow him to breathe (23-3C). Then, carefully deliver the rest of his head (23-3D). If you cannot get at least his mouth and nose into fresh air with the Burns– Marshall method: (1) use the MAURICEAU–SMELLIE–VEIT manoeuvre, or (2) apply forceps to his aftercoming head. Rest his belly and chest on your right forearm; put your right middle finger in his mouth, and your index and ring fingers on his malar bones. Put your left hand over his back; put your middle finger on his occiput and your index and ring fingers over his shoulders. This will give you some control over the flexion and rotation of his head. Grip his skull and guide it through her birth canal. Ask her to stop pushing. Ask your assistant to put his fist on the baby’s head, which is still palpable above her pubis, and to press obliquely downwards in the direction of her coccyx. You will feel a ‘plop’ indicating that his head has gone into her pelvis, and further delivery by the Mauriceau–Smellie–Veit manoeuvre should then be easy. CAUTION! This is a method for getting a grip directly on his head. NEVER pull on his shoulders, you can too easily distract his cervical vertebrae and damage his cord. NOTE: Although Mauriceau–Smellie–Veit is a cumbersome eponym, it is preferred to the alternative which is ‘jaw shoulder traction’ since this suggests, although it does not intend, traction on the neck, which is very dangerous. EARLY DIFFICULTIES DELIVERING A BREECH CAUTION! (1) Do an episiotomy (except in a grand multipara with a very lax outlet) before you do any manipulations, because there is a high risk of a perineal tear. (2) Don’t squeeze his abdomen! (3) If his head fails to descend, don’t pull on his neck. (4) If his head becomes impacted and he dies, don’t sever his neck, or be tempted to open her uterus from above. Figure 19.4: TWO METHODS FOR DELIVERING THE HEAD IN A BREECH PRESENTATION. A, applying forceps to the aftercoming head. B, the Mauriceau– Smellie–Veit manoeuvre is a method for getting a grip directly on a baby’s head. Rest his belly and chest on your right forearm; put your right middle finger in his mouth, and your index and ring fingers on his malar bones. Put your left hand over his back; put your middle finger on his occiput and your index and ring fingers over his shoulders. This will give you some control over the flexion and rotation of his head. Guide his head through his mother’s birth canal and don’t pull on his shoulders. The finger in his mouth is for convenience only. If his breech is DELAYED AT THE BRIM, or in midcavity, this is probably a warning sign of CPD; do a Caesarean section. Don’t try to deliver her with oxytocin. If his breech is DELAYED AT THE OUTLET, make sure that the episiotomy is adequate. There may be CPD. If her pelvis feels contracted, or he is large, do a Caesarean section. If all is otherwise well, do gentle groin traction, as for breech extraction. Figure 19.5: LØVSET’S MANOEUVRE for the delivery of the shoulders in a breech presentation. The bottom row of drawings show a view from the patient’s perineum. The top row shows the same stage viewed from her left. Remember: ‟if you don’t know which way to turn him, keep his back anterior, so that it passes under her clitoris”. Many obstetricians merely wiggle him one way then the other, pull, and try to find an arm: but this is the detailed manoeuvre. Practise it on a model. If you have delivered his legs but BOTH HIS SHOULDERS HAVE NOW STUCK above the pelvic brim, his arms are probably extended (23-5A). Normally you can put a finger up her posterior vaginal wall and easily bring them down. If you cannot, they are probably forced into extension. Try LØVSET’S manoeuvre. It is a breech extraction for obstruction late in delivery, and should rarely be necessary. The delivery of his shoulders is prevented by two obstructions at different levels; (1) her sacral promontory, (2) her pubis. The principle of this method is that, by pulling him tightly down on to both, and by turning him through 180 , the shoulder which was held up above her pubis will turn to pass into the hollow of her sacrum, and the shoulder which was above her sacrum will now be above her pubis. Two further ‘unscrewing’ half-turns like this, each bringing his shoulders progressively below these obstructions will deliver him. Grasp his thighs and pelvis with both hands (if he is slippery use a gauze swab or small towel), your thumbs along his sacrum, your forefingers on his symphysis, and your remaining fingers round his thighs. If, in the extreme case, he obstructs transversely (23-5A), start by turning him through 90 , so that his back faces to her left. His left shoulder will then be above her symphysis, and his right shoulder above her sacrum (23-5B). With your first 180 turn (23-5B–C), bring his left shoulder under her sacrum. With your second second turn (23-5C–D) bring his right shoulder under her sacrum. His left arm will now be low enough for you to gently sweep it down. With your third turn (23-5D–E) bring his right shoulder under her pubis; it will now be low enough for you to bring his right arm down. CAUTION! (1) These three 180 turns are in opposite directions, so that his back always passes under her clitoris, and the arm which started posterior always drags across his face. His belly should never pass under her clitoris. (2) In the worst case you start in 23-5A with both arms extended, so you have to begin with a 90 turn, followed by three 180 turns. If he arrests at a later stage, with only one arm extended, you may only need two turns, or perhaps only one. (3) The first two turns release the shoulder which was arrested above her symphysis when you started it. The third enables you to bring down his right arm. (5) Don’t squeeze his belly, or back, or you may rupture his liver, kidneys, spleen, or adrenals (huge in the newborn). If you hold his chest, take care not to compress his abdomen. (6) Remember that the upper part of the birth canal, in which he has stuck, is directed backwards, so start by pulling him backwards. If LØVSET’S MANOEUVRE FAILS TO DELIVER HIS SHOULDERS, it is usually a failure of technique. You may have to be a little firmer, or reach up a little higher to get his arm down. A broken arm will soon heal, so it is no disaster, and is better than letting him die. LATER DIFFICULTIES DELIVERING A BREECH CPD is the most important cause. IF HIS HEAD IS STUCK ABOVE THE BRIM, you are in trouble. You may be able to draw it into her pelvis with the Mauriceau–Smellie–Veit manoeuvre. If this fails, he will probably be dead, and the best treatment will be craniotomy (see below). If HIS HEAD HAS ENTERED THE PELVIS AND THE MAURICEAU– SMELLIE–VEIT MANOEUVRE FAILS to deliver it, rotating his head in her pelvis may help. Stop struggling and think. What is the cause? If it is CPD, and you are an experienced symphysiotomist with an equally experienced obstetric team, a quick symphysiotomy may save him. On the other hand, an unskilful symphysiotomy may cause pelvic trauma and laceration of her urinary tract, so only attempt this if you and your team are expert. If CPD IS THE CAUSE OR SHE IS NOT FULLY DILATED, and you cannot deliver him, let him die and avoid harming her. While she is still in the lithotomy position, sedate her with pethidine 50mg and let him hang for a while. His head will usually mould, or her cervix will dilate, so that he is delivered in less than an hour. Alternatively, if his head has stuck in her incompletely dilated cervix (uncommon) either: (1) Apply standard obstetric forceps, such as those of Neville Barnes, inside it. While you apply gentle traction, try to slip her cervix over his head. Or, (2) if this fails, cut her cervix boldly with scissors at 4 and 8 o’clock, and repair your incisions afterwards. Some contributors consider this a relatively safe and successful method, one considers it bloody and dangerous. This complication usually happens to premature breech deliveries, who may not be worth the risk involved. If the ABOVE MEASURES FAIL AND CPD is severe, you may have to do a CRANIOTOMY through his foramen magnum (unpleasant but effective) (22.9). Ask an assistant to pull down his body. Retract her anterior vaginal wall with a Sims’ speculum and expose the back of his neck. Pick up a fold of of the skin over his cervical spine with toothed forceps, and incise it transversely. Use curved Mayo’s scissors to cut a tunnel under his skin up to his occipital bone, and push scissors into his head. Open the scissors a few times to break up his brain compartments. Pull gently on his neck while his brain gradually escapes. Or, make a transverse incision over his highest cervical spine and push a straight metal catheter through it on into his foramen magnum. Or perforate his occiput. He should now deliver quite easily by the Mauriceau–Smellie–Veit manoeuvre. If he still does not deliver, pass a crotchet up the tunnel and hook it on to the base of his skull. If he has HYDROCEPHALUS, see 23.6. If she is brought in with HIS DEAD BODY PROTRUDING FROM HER VULVA, examine to feel if her cervix is fully dilated or not. If it is fully dilated, proceed directly to decompress his head with a craniotomy. If it is not fully dilated, hang a weight of 1 kg on his trunk. His head will usually mould and deliver within 1hr. If this fails, do a craniotomy. CAUTION! Don’t try to pull his head forcefully through her undilated cervix. You may cause tears which extend into her lower segment. If his NECK HAS BEEN SEVERED, and his head has gone back into her uterus, it will be difficult to find and remove. Use craniotomy equipment. If his CORD PROLAPSES, manage her as you would with a cephalic presentation—do a Caesarean section, unless her cervix is fully dilated, and she is about to deliver. Cord prolapse is more common with breech deliveries, especially with a footling. OTHER METHODS FOR BREECH DELIVERY BREECH EXTRACTION uses your pulling forces, rather than her pushing forces. It is a quick way of delivering a small breech baby, usually a second twin. It may be indicated for: (1) Delay with the second twin. (2) Fetal distress with the second twin. (3) Cord prolapse at full dilatation with a breech. (4) A transverse lie in a second twin, following internal version. (5) A dead baby. METHOD She must be in the lithotomy position. Proceed as for an assisted breech delivery. You will need good anaesthesia: a subarachnoid (spinal) anaesthetic, an epidural or a pudendal block. Avoid GA. An episiotomy is vital. Hook the index fingers of each hand into his groins and pull, preferably during a contraction. When his umbilicus appears, hook out his legs by flexing his knees. Do this by applying lateral and dorsal pressure in his popliteal fossae, and by sweeping each leg laterally and downwards. Pull on his pelvis, keeping his back anterior. Pull posteriorly. A common error is to pull him towards you, which is not in the axis of her birth canal. When you see his scapulae, hook out his arms. If his arms are not across his chest do Løvset’s manoeuvre. Push his head into his mother’s pelvis from above. Then, if necessary, consider applying forceps to his aftercoming head. The main difficulty is that his arms are more likely to be extended above his head, and his head is more likely to become deflexed. Løvset’s manoeuvre and the Mauriceau– Smellie–Veit manoeuvre should solve these problems. Alternatively, if he is dead: (1) Pull on his leg(s), if you can reach them, or (2) use a combined breech hook and crotchet (19-2). Pass the blunt hook end of this instrument over an extended leg into his groin, and pull on that. If he is macerated his leg may be pulled off. If it is pulled off, turn the instrument round and hook the sharp crotchet end over his iliac crest. FORCEPS FOR THE AFTERCOMING HEAD. Standard obstetric forceps, such as those of Neville Barnes: (1) Are not easy to use on the aftercoming head. (2) Are liable to misuse if they are in the labour ward at all. (3) Create the impression for midwifery students that a breech delivery is something that only doctors can do. They must see methods used that they can use themselves at home or in a clinic. Outlet forceps (Wrigley’s) are not long enough when you really need them. If they will reach his head they are hardly necessary in a breech delivery. If you are going to use them, wait until you see his hair line. Ask your asistant to lift him by his ankles, then apply the left blade, followed by the right one. Slowly and gradually deliver his head with them. THE CORRECTED PERINATAL MORTALITY FOR BREECH DELIVERIES (see above). This should be fairly easy to calculate from your labour ward record books, which should routinely record presentation, birth weight, obvious abnormalities, and live and still births. (1) Work out your perinatal mortality for all babies, excluding breeches, babies <2.5 kg, twins, and babies with obvious malformations. The perinatal period lasts from the 28th week to the end of the first week of life. (2) Do the same for breech deliveries only. Subtract (1) from (2). If the difference is >20/1000, do external version. In many district hospitals it is 50/1000.