Intern H&P Form
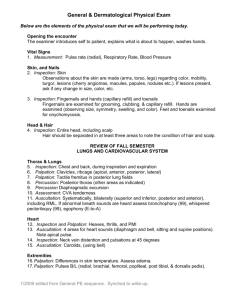
advertisement
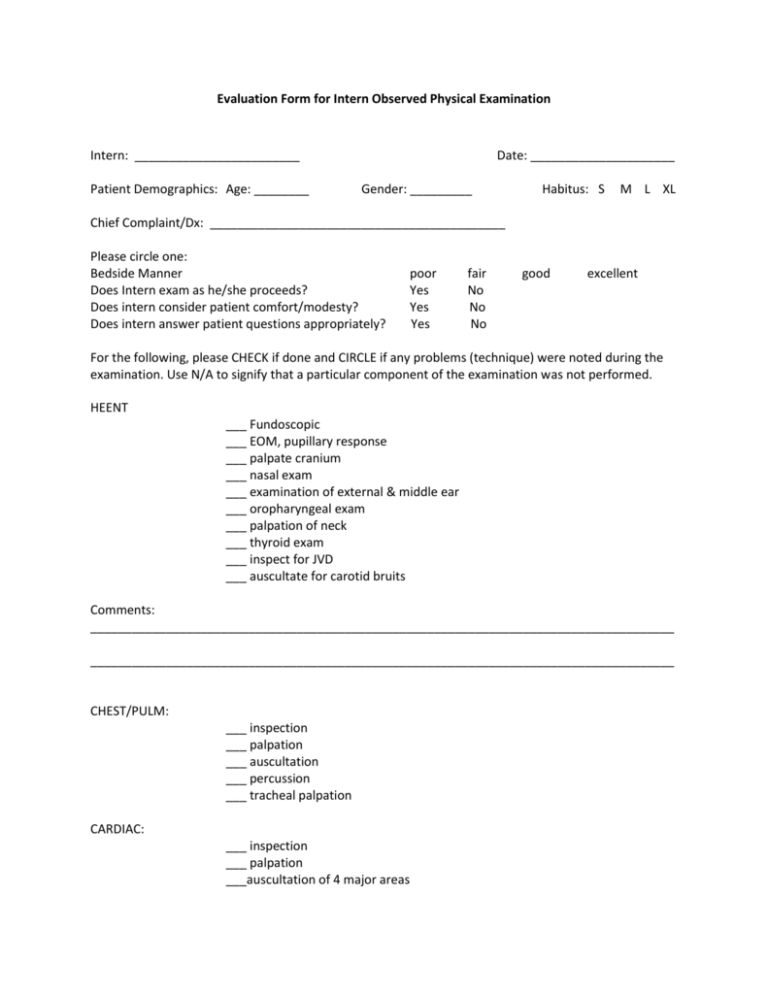
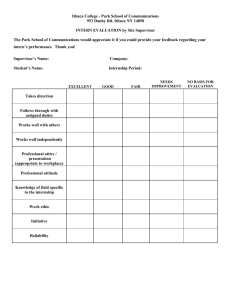
Evaluation Form for Intern Observed Physical Examination Intern: ________________________ Patient Demographics: Age: ________ Date: _____________________ Gender: _________ Habitus: S M L XL Chief Complaint/Dx: ___________________________________________ Please circle one: Bedside Manner Does Intern exam as he/she proceeds? Does intern consider patient comfort/modesty? Does intern answer patient questions appropriately? poor Yes Yes Yes fair No No No good excellent For the following, please CHECK if done and CIRCLE if any problems (technique) were noted during the examination. Use N/A to signify that a particular component of the examination was not performed. HEENT ___ Fundoscopic ___ EOM, pupillary response ___ palpate cranium ___ nasal exam ___ examination of external & middle ear ___ oropharyngeal exam ___ palpation of neck ___ thyroid exam ___ inspect for JVD ___ auscultate for carotid bruits Comments: _____________________________________________________________________________________ _____________________________________________________________________________________ CHEST/PULM: ___ inspection ___ palpation ___ auscultation ___ percussion ___ tracheal palpation CARDIAC: ___ inspection ___ palpation ___auscultation of 4 major areas ABDOMINAL: ___ inspection ___ palpation (light and deep) ___ percussion ___ auscultation ___ maneuvers to accentuate abnormalities ___ CVA tenderness ___ checks femoral pulses; listen for bruits Comments: _____________________________________________________________________________________ _____________________________________________________________________________________ EXTREMITIES/SKIN: ___ inspection (including accurate verbal description of skin/nail chgs) ___ comments on muscle bulk, atrophy or signs of physical trauma ___ check for peripheral pulses ___ accurately assesses cyanosis/capillary refill ___ can identify signs of chronic peripheral vascular disease ___palpation of joints, checking for effusions ___ testing for knee joint stability ___ can accurately describe any joint abnormality ___ testing for sciatic irritation (SLR) ___ assesses for edema and accurately rates it (if present) ___ can identify clubbing NEUROLOGIC: ___ knows how to perform MMSE ___ comments on any abnormal movement disorders ___ cranial nerve testing ___ deep tendon reflexes ___ cerebellar testing ___ evaluates gait appropriately ___ accurately rates muscle strength ___ comments on muscle tone; recognizes spaticity/rigidity ___ plantar reflex ___ appropriate sensory examination (pain, microfilament, temp) ___ proprioception testing Comments: _____________________________________________________________________________________ _____________________________________________________________________________________ NOTE: Genitourinary examination testing will be performed at a later date; but have intern explain how they would perform: ___ prostate/rectal exam ___ inguinal hernia testing ___ scrotal examination ___ breast examination ___ pelvic speculum exam ___ bimanual palpation of cervix, ovaries, uterus ___ how to obtain a pap smeer ________________________________ Supervising Attending or Chief _________________ Date Evaluation form for intern chart stimulated review Intern: ________________________ Setting: Inpatient Date: _____________________ Outpatient Primary Diagnosis: ___________________________________________ 1. CC/HPI: Were the salient presenting symptoms of this patient adequately represented? YES NO Comments: _______________________________________________________________ 2. PMHx: Were pertinent positive and negatives documented? YES NO Comments: _______________________________________________________________ 3. Were the following reported in appropriate depth? Family Hx Yes ____ No ____ Social Hx Yes ____ No ____ Medications Yes ____ No ____ Surgical Hx Yes ____ No ____ Allergies Yes ____ No ____ ROS Yes ____ No ____ 4. Please comment on the completeness of the PE report: ____________________________________________________________________________ ____________________________________________________________________________ 5. Were the initial lab/diagnostic studies ordered and interpreted appropriately? YES NO Comments: _______________________________________________________________ 6. Was a thoughtful differential diagnosis generated and discussed? YES NO Comments: _______________________________________________________________ 7. Was the therapeutic plan logical and well-described? YES NO Overall evaluation for Observed H&P + Chart Stimulated Review ___ Exceeded expectations for level of training ___ Met expectations for this level of training ___ Minor deficiencies noted and discussed with interns ___ Major deficiencies noted, needs to repeat this exercise after remediation Final Comments: _____________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ________________________________ Supervising Attending or Chief _________________ Date