Infections of the Gastrointestinal Tract
advertisement

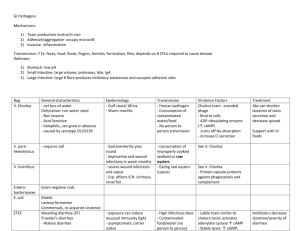
Infections of the GI and Diarrheal Illness Clinical Syndromes 1. Gastritis - inflammation of the stomach - pain in the upper abdomen, sometimes bleeding 2. Gastroenteritis - inflammation of stomach & intestines - primarily diarrhea, sometimes nausea, vomiting, crampy abdominal pain 3. Colitis - intestinal syndrome that primarily involves the colon or large intestines. 4. Enterocolitis - inflammation of mucosa of both large & small intestine = dysentery - diarrhea often contains blood & mucus. 5. Hepatitis - liver damage causes a clinical syndrome called hepatitis. Patients with hepatitis become jaundiced because bilirubin builds up in their bodies. Pathogens Cause disease by 3 mechanisms: a. action of toxins b. adherence to & effacement of microvilli inflammation c. invasion of intestinal epithelial cells A. Toxins cause disease – microbes are not present in the body Toxin types Action on intestine/intestinal cells Enterotoxin results in net secretion w/out intestinal damage Cytoskeleton-altering toxin alters cell shape, may injure cells but is not lethal Cytotoxin causes cell damage and ultimately cell death Neural toxin alters smooth muscle activity in intestines 1. Bacterial Food Poisoning - Intoxications NOT infections – a. Clostridium botulinum - botulism - canned foods, spores survive 5 hrs boiling & germinate under anaerobic conditions in can neural toxin gut – binds to epithelial cell and is transported across bloodstream presynaptic regions (disease of CNS, symptoms begin 1248h) b. Staphylococcus aureus - most common – 2 different heat [100ºC for 30 min] & enz stable enterotoxins stimulate vegus nerve (so also a neural toxin) of stomach lining emetic response (vomiting),w or w/o diarrhea 30 min to 8 hrs after ingestion. These toxins also function as superantigens and stimulate T cells to over secrete IL2. 1ug of toxin is enough to induce symptoms, can be achieved when # of Staph in food reaches 1,000/gram. Resolves within 24h. c. Bacillus cereus 2 distinct presentations caused by two different toxins – only one is atrue intoxication emetic – cereulide (an enterotoxin) targets vagus nerve nausea & vomiting 1-5 hrs after ingestion of toxin - lasts ~1-6 hrs. can be difficult to distinguish from S. aureus food poisoning. B. True infections – microbes enter and then colonize the GI - 3 mechanisms for damage 1. Pathogens colonize epithelial surfaces of small intestine & then release toxins Vibrio cholera - cholera Source Pathology 1. Ingestion of large numbers (> 108) 2. Flagella & mucinase allow Vibrio to reach epithelial cells 3. Attachment by way of fimbriae to receptors on brush border & crypt cells of small intestine 4. Damage due to production of toxin called cxt that is an ADP ribosyl transferase. Toxin binds to receptors for the glycolipid GM1 ganglioside by the B subunit & A enters epithelial cells disrupts adenylate cyclase (cxt - enterotoxin, cytotoxin, neural toxin) 5. Secretion of large quantities of Cl- into intestine, causing H2O & and Na+ to follow hypersecretion of fluids & electrolytes Incubation – Symptoms - Txt - Also enterotoxigenic E. coli strains (ETEC) - traveler’s diarrhea – 2 enterotoxins – LT-1 similar to cholera toxin. ST – activates guanylate cyclase activity increase in cGMP increased fluid secretion. B. cereus – ingested diarrheal toxin produced in the small intestine (cytotoxin targets villi villus necrosis) diarrhea 8-16.5 hrs after ingestion 2. Pathogens attach to and enter epithelial cells, multiply intracellularly & destroy (efface) microvilli of epithelial cells (may release toxins), and induce diarrhea. Shigella spp. (dysenteriae, boydii, flexneri, sonnei) – shigellosis - 14,581 U.S. / 212 MI Source Pathology 1. Ingestion - only 10 organisms required - most effective of bacterial pathogens of GI 2. Adhere specifically to epithelial cells of colon by way of outer membrane proteins (OMP) 3. Induce parasite-directed endocytosis by M cells of GALT (Gut Associated Lymphoid Tissue) that transport Shigella across intestinal epithelium 4. Phagocytized by macrophages but escape from phagolysosome into cytoplasm 5. Trigger macs to produce IL-1, also triggers apoptosis 6. IL-1 induces inflammation & stimulates edema & extravasation of neutrophils (PMNs) across epithelial barrier. 7. movement of PMNs across destroys the epithelial barrier & Shigella can now move across in massive number. 8. Further induce prod of cytokines & intense inflammation w/ destruction of epithelium S. dystenteriae also secretes a cytotoxin Incubation – Symptoms - Txt – Complications - Also Enterohemorrhagic E. coli (EHEC) including E. coli O157:H7 4,323 U.S ./ 158 MI Human diarrhoeal viruses (rotavirus, Norwalk virus) - gastroenteritis Virus replicates in intestinal epithelial cells, damages transport mechanisms in the gut, leads to loss of water, salt, glucose diarrhea Infected cells are destroyed but no inflammation, no blood. Shed at rate of 1,000 million virus particles/g feces. Campylobacter enteritis + diarrhea Entamoeba histolytica amoebic dysentery 3. Pathogen attaches to, enters, & multiplies in deep tissues that are normally sterile submucosal or subepithelial tissues – sometimes will spread systemically. Salmonella enteritidis, S. typhimurium salmonellosis 44,468 U.S. / 911 MI Salmonella typhi, paratyphi – invasive species typhoid fever Source Pathology 1. Ingestion of large numbers (105-109) 2. Attach specifically to fibronectin of epithelial cells of small intestine 3. Transported by M cells of GALT 4. Invade gut wall ulcerations & hemorrhage. Also spread to intestinal lymphatics & are phagocytized by macs but escape from phagolysosome into cytoplasm 5. Produces toxin that increase cAMP & fluid secretion loose, watery diarrhea & nausea (enterotoxin and cytoskeletal altering toxin) 6. Causes influx of PMN (nontyphoid) that confines infection to GI 7. OR influx of macrophages (typhoid) and systemic spread S typhi organisms spread through the reticuloendothelial system, mainly to the liver, spleen, and bone marrow. Within 14 days, the bacteria appear in the bloodstream, facilitating secondary metastatic foci (eg, spleen, heart). In some patients, gallbladder infection leads to long-term carriage of S typhi or S paratyphi in bile and secretion to the stool Salmonellosis Incubation – Symptoms – Txt Complications – Also Hepatitis A virus - 1,849 cases U.S. / 70 MI Reoviruses Enteroviruses (includes poliovirus)