Department of Pediatrics Clinicopathologic Conference February 3
advertisement

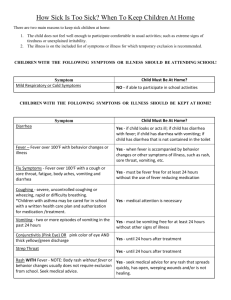
Case History Family History: Sickle Cell Trait in mother HPI: 2 month old female with perinatal HIV exposure presented to CHoR Emergency Department August 9, 2014 for fever, vomiting, diarrhea and fussiness that began the day prior to admission. Fever noted as high 104 ⁰ F at home, not responsive to over the counter antipyretics (acetaminophen). Emesis was described as non-bloody, non-bilious and was also not posttussive. Diarrhea was non-bloody and without mucous. She had decreased intake but no change in her urine output. No cough, congestion, respiratory distress, diarrhea or rashes noted at admission. She was initially admitted to General Pediatrics. Blood, urine and CSF cultures were obtained. Inadequate CSF volume was obtained for sending cell counts or HSV. She was started empirically on vancomycin and ceftriaxone for rule-out sepsis. Macular rash subsequently developed over her trunk on August 10, day off illness #2 with perioral dermatitis, cracked lips, and desquamating diaper dermatitis. Abdominal distension developed on August 11, day off illness #3 and nasogastric sump placed. On August 14, day of illness #5, she developed worsening tachycardia, tachypnea, a new oxygen requirement, generalized edema, oliguria, diarrhea, worsening anemia and thrombocytopenia. She was transferred to the PICU where central access was obtained, she was intubated and doxycycline was added to her antibiotic regimen. She required platelet and packed red blood cell transfusions. She continued to spike fevers and remained intubated without an identified etiology of her illness. She was given an empiric course of IVIG. The patient continued to spike fevers and have intermittent bouts of diarrhea until Aug 22, day of illness #14. PMH: Full term – mom HIV +, undetectable viral load. Other labs benign Sickle Cell Trait Perinatal HIV exposure – completed 6 weeks AZT with negative PCR testing at birth, 4 weeks, 8 weeks of age PSH: None Social History: Lives with mom and dad Family from Sierra Leona (have been in US for 5 years) Allergies: No known allergies Medications: Tylenol as needed Physical Exam – at time of PICU Transfer Vital Signs: T 38.0 C, BP 97/74, HR 182, RR 54, SpO2 96% on 2L NC, Wt 6.8 kg (up 800 g since admission) General: crying in mom’s arms, not easily consolable, generalized edema HEENT: Anterior fontanel soft and flat, no scleral icterus, + conjunctival injection with clear drainage and desquamation of lids, erythematous and cracked lips with erythematous tongue, no intraoral lesions Neck: supple Resp: head bobbing, nasal flaring; good aeration bilaterally without wheezes, rales or rhonchi CV: tachycardic, no murmurs appreciated. Dorsalis pedis pulse 2+, diffuse non-pitting edema of extremities and face noted. Abd: soft, distended, normal bowel sounds present. Palpable liver edge 2 cm below costal margin, palpable spleen tip, reducible umbilical hernia MSK: transverse brown lines on fingernails Neuro/Psych: awake, alert, tracking, no focal deficits, spontaneously moving all extremities Integument: erythematous diaper dermatitis with desquamation; macular erythematous rash across trunk Laboratory and Imaging Admission Labs (8/10): WBC – 20.8 x 109/L (N 64%, L 28%, M 6%, E 2%), Hemoglobin – 10.4 g/dL, Hematocrit – 31.6%, Platelets – 275 x 109/L Na – 135 mmol/L, K – 4.6 mmol/L, Cl – 105 mmol/L, HCO3 – 23 mmol/L, BUN – 7 mg/dL, Cr – 0.22 mg/dL, Glu – 135 mg/dL, Ca – 9.6 mg/dL AST – 50 U/L, ALT – 32 U/L, Alk Phos – 206 U/L, Bilirubin – 0.8 mg/dL, Protein – 5.4 g/dL, Albumin – 3.5 g/dL CRP – 9.6 mg/dL Additional Work-Up: Blood culture 8/10: Negative Urine Culture 8/10: Negative CSF Culture 8/10: Negative CSF Enterovirus 8/11: Negative Respiratory Pathogen Panel: Negative West Nile Virus: Negative Enterovirus (Stool): Negative Echo (8/14): trivial mitral regurgitation, normal left ventricle and size, normal coronary arteries, trivial pericardial effusion, small ASD vs PFO CXR (8/10): No focal consolidation, effusion or pneumothorax Abd US (8/14): Mild hepatomegaly, small intraperitoneal free fluid Department of Pediatrics Clinicopathologic Conference February 3, 2015 Bone Marrow Biopsy (8/15): Normocellular Admission Medications: Vancomycin Ceftriaxone Continued Laboratory Studies 8/14/14: WBC – 14.0 x 109/L (N 86%, L 8%, M 3% E 2%); Hemoglobin – 8.4 g/dL, Hematocrit – 25.8%, Platelets – 30 x 109/L CRP – 15.5 mg/dL PT – 19.4 sec, INR – 1.7, PTT – 50 sec, Fibrinogen – 265 mg/dL, D-Dimer – 3.04 mcg/mL FEU AST – 32 U/L, ALT – 24 U/L, Alk Phos – 100 U/L, Bili – 0.6 mg/dL, Protein – 3.0 g/dL, Albumin – 1.8 g/dL Zinc: < 25 ug/dL, Copper – 81 ug/dL Triglyceride – 198 mg/dL Ferritin – 813 ng/mL Anti-ds DNA Ab: < 12.3 IU/mL Haptoglobin – 142 mg/dL, Lactate Dehydrogenase – 335 U/L A confirmatory laboratory test was sent 2 month old female with fever, diarrhea and rash