Medical Problem Solving Case study A young Mennonite Patient JE
advertisement

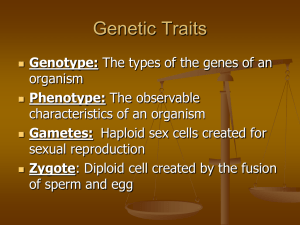
Medical Problem Solving Case study A young Mennonite Patient JE was 20 months of age when first referred by her pediatrician to a university health center child neurologyclinic. Her mother’s pregnancy period was normal. There were no concerns about her physical or neurological health until age 8 months, when she began to fall over from a crawling position. She sat at 12 months, cruised at 16 months, and was not walking when first evaluated at age 20 months. Neurological examination was notable for truncal ataxia only when standing (not when sitting), ‘‘clumsy’’ upper extremity movements (without true target-seeking tremor), and symmetrically brisk patellar tendon reflexes. Muscle power and tone were normal and she was adept at crawling. During the initial evaluation, she was speaking in short sentences. Intellectual function and social interactions were appropriate for age. Linear growth delay was recognized at age 2.5 years and she had a poor endogenous growth hormone (GH) response to arginine loading. She continued to have gross and fine motor delays, and did not ambulate independently until after age 3 years. Gait subsequently deteriorated, necessitating the use of canes and ankle supports. She walked with a wide base, continued to have truncal titubation, and developed a target-seeking tremor. Tendon reflexes, initially brisk, were hypoactive by age 4 years. Language and cognitive delays became more evident with advancing age, and significant learning disabilities were apparent once she entered school. Over a 4.5 year period, JE was evaluated by specialists in pediatric neurology and biochemical genetics, had two sedated MRIs, a fluorodeoxyglucose PET scan, karyotype testing, and a variety of biochemical test. MRI findings were similar at ages 2 and 4 years, showing supratentorial hypomyelination and a thin corpus callosum. In 2003, JE’s parents informed the doctor about a second cousin of the proband exhibiting a similar clinical course. With IRB approval and appropriate signed consents, doctors initiated a genome-wide mapping study using the two affected patients, their parents, and Affymetrix GeneChip Mapping 10K Arrays Your Task: Spend some time using OMIM database to see if you can diagnose this child’s condition. How do I do that? Well this data base is useful if you can pick out key words pertaining to this illness. Go back and write down some important facts about this patient. Need a clue? Mennonite would be a good one. (Hint )If you are listing multiple symptoms, capitalize the A in And in your search. Website for Online Mendelian Inheritance and Man= http://www.ncbi.nlm.nih.gov/sites/entrez?db=omim What did you use to search at first?_________________________________________________________________ ._______________________________________________ Fill in the chart with your top three genes from the website Candidate Gene Gene location (locus) Example 10q17-q20 Physical location (click on Map viewer located to the right) Your gene will be highlighted. The # will be on the ruler Having some trouble? ? Try gross motor delay Mennonite And truncal ataxia And slow linear growth. This will give you one disorder. What is it?_______________________________ What does this gene do? What is the actual name of this disorder in the Mennonite population?________________________ Fig. 2. Genome-wide SNP mapping study localizes unexplained DD phenotype in two Old Order Mennonite children. A: Concise pedigree showing the relationship between the two affected children. Question: Is this homozygous dominant or recessive?__________________________ How could you tell?_________________________________________ B: Two mapping parameters, homozygous haplotype length (i.e., number of contiguous homozygous SNPs) and location score (as previously described in Puffenberger et al., 2004), were maximized on chromosome 6q12-14 in the two patients. Fifty-five contiguous SNPs delimited the linked region, which contained 55 genes including SLC17A5. This analysis did not explicitly rely on genotype or haplotype data from theparents, except that the untransmitted alleles from the parents were used to determine population-specific allele frequencies Question: If the X axis is the actual 23 chromosome pairs, for these two patients with the disorder, which chromosome do they share the greatest homozygous haplotype length?__________________________________ What do you think the first part of 6q12-14 is telling you?______________________ . C: Sequence analysis of the SLC17A5 exon 2 revealed a homozygous pathogenic sequence variant, 115C!T (R39C), in both patients. This is the common variant found in Salla disease patients from Finland. Question: Using your best deductive reasoning-Is Salla disease a missense, nonsense or other mutation?__________________________Why?