GERD Case 416 Sept.
advertisement

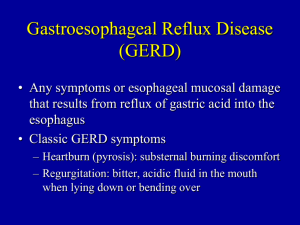
A Burning Question (Level II) Learning Objectives After completing this case study, students should be able to: Describe the clinical presentation of gastroesophageal reflux disease (GERD), including typical, atypical, and alarm symptoms. Discuss appropriate diagnostic approaches for GERD, including when patients should be referred for further diagnostic evaluation. Recommend appropriate nonpharmacologic and pharmacologic measures for treating GERD. Develop a treatment plan for a patient with GERD, including both nonpharmacologic and pharmacologic measures and monitoring for efficacy and toxicity of selected drug regimens. Effectively counsel patients with GERD on the proper use of their drug therapy. Patient Presentation Chief Complaint “I'm having a lot of heartburn. These pills I have been using have helped a little but it's still keeping me up at night.” HPI Janet Swigel is a 68-year-old woman who presents to the GI clinic with complaints of heartburn four to five times a week over the last 5 months. She also reports some regurgitation after meals. She states that her symptoms are much worse at night, particularly when she goes to bed. She finds that her heartburn worsens and she coughs a lot at night, which keeps her awake. She has had difficulty sleeping over this time period and feels fatigued during the day. She reports no difficulty swallowing food or liquids. She has tried OTC Prevacid 24HR once daily for the last 3 weeks. This has reduced the frequency of her symptoms to 3-4 days per week, but they are still bothering her, and she needs help. PMH Atrial fibrillation × 12 years Asthma × 10 years Type 2 DM × 5 years HTN × 10 years SH Patient is married with three children. She is a retired school bus driver. She drinks one to two glasses of wine 4-5 days per week. She does not use tobacco. She has Blue Cross prescription drug coverage. FH Father died of pneumonia at age 75, mother died at age 68 of gastric cancer. Meds Diltiazem CD 240 mg po once daily Metformin 500 mg po twice daily Aspirin 81 mg po daily Fluticasone/salmeterol DPI 100/50 one puff twice daily All Peanuts (hives) ROS Reports being tired all the time, (-) SOB or hoarseness; (+) cough at night, (+) frequent episodes of heartburn, sometimes after meals, but is worse at night; (-) N/V; (-) BRBPR or dark/tarry stools; (-) dysuria, nocturia, or frequency Physical Examination Gen Well-developed African-American woman in NAD VS BP 139/82, P 90, RR 17, T 36°C; Wt 100 kg, Ht 5′7″ Skin No lesions or rashes HEENT PERRLA; EOMI; moist mucous membranes; intact dentition; oropharynx clear Neck/Lymph Nodes Trachea midline; (-) thyromegaly; (-) lymphadenopathy; (-) JVD Lungs/Thorax Mostly CTA bilaterally, some intermittent wheezes Cv Tachycardia with irregularly irregular rhythm; no MRG Abd Obese; NT/ND; (+) BS; (-) HSM Genit/Rect Gyn exam deferred; heme (-) brown stool MS/Ext No CVA tenderness Neuro A & O × 3, CN II-XII intact, 5/5 upper- and lower-extremity strength bilaterally Labs Save Table | Print Na 138 mEq/L Hgb 13 g/dL AST 21 IU/L K 3.8 mEq/L Hct 39% ALT 24 IU/L Cl 108 mEq/L RBC 4.6 × 106/mm3 Alk Phos 55 IU/L CO2 21 mEq/L Plt 400 × 103/mm3 Fasting lipid panel: BUN 18 mg/dL WBC 8.7 × 103/mm3 TC 230 mg/dL SCr 1.3 mg/dL Neutros 60% LDL 130 mg/dL FBG 220 mg/dL Bands 1% TG 170 mg/dL Ca 8.9 mg/dL Eos 2% HDL 42 mg/dL Phos 4.1 mg/dL Lymphs 32% Monos 5% A1C 9.0% EGD Grade B esophagitis; normal gastric and duodenal mucosa; small hiatal hernia. Biopsy results of esophagus and stomach are negative for atypical cells and H. pylori. Assessment A 68-year-old woman presenting with uncontrolled GERD symptoms despite self-treatment with OTC PPI therapy. EGD show erosive esophagitis and a hiatal hernia. Instructions Work in groups ( 12 groups of 5 students and 2 groups of 6 students) to solve the case & answer the case related questions Every group is required to 1. Read the case carefully 2. Use the book chapter, guidelines and/or any other references to answer the following questions: Classify the GERD symptoms this patient is experiencing. Are they typical or atypical in nature? Are any alarm symptoms or features present? What factors could be contributing to the development of GERD symptoms in this patient? Develop a list of pharmacotherapeutic goals for this patient. What lifestyle modifications or nonpharmacologic therapies may improve this patient’s GERD symptoms? (at least 4 specific recommendations) Develop a complete treatment plan for managing this patient’s GERD symptoms (drug, dose, duration, frequency) Does this patient require maintenance therapy? If yes, recommend a drug regimen. What parameters should be monitored to assess both the efficacy and toxicity of your selected drug regimen for GERD treatment? What would be the best management if the patient still complains of infrequent breakthrough symptoms after meals even after receiving your recommended therapy? Be specific when recommending any treatment even when multiple options are available. Select the single most appropriate therapy. Appropriate scientific references should be used. Websites targeting patients are not considered appropriate. List all references used in the proper format (Vancouver reference style). Copying/pasting from any reference, website…..etc. is not acceptable. You should understand the text & then answer questions using your own wording & expressions. Copying/pasting from previous or current students’ assignments is considered academic plagiarism. Zero grade will be awarded to all groups/students involved. The due date for submission is Sunday 9th November 2014. Late submissions will not be accepted. All work should be submitted as hard copy. The assignment accounts for 5 marks.