Title: Plasma Hydrogen Sulfide (H2S) Levels in CKD Patients
advertisement
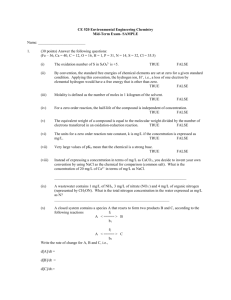
P169 Plasma Hydrogen Sulphide (H2S) Levels in CKD Patients Stephen John 1 , Michael J. Garle 2, Paul J. Owen 1, Vera Ralevic 2, Saoirse O'sullivan 2, Chris W. McIntyre 1,2 1. Department of Renal Medicine, Royal Derby Hospital, Derby 2. Graduate Entry Medicine and Health, University of Nottingham, Derby Background: Animal models of chronic kidney disease (CKD) and CKD patients have reduced plasma hydrogen sulphide (H2S) concentrations. H2S inhibits phosphate-induced calcification and osteoblastic differentiation of vascular smooth muscle cells, which suggests a role in arterial calcification. We aimed to investigate the role of H2S in vascular calcification and arterial stiffness in CKD. Methods: We recruited 54 hypertensive non-diabetic patients (≥70 yrs) (CKD 3/4 (n=29), non-CKD controls (n=25)). Pulse wave velocity (PWV) and analysis were assessed by applanation tonometry, central haemodynamics by continuous digital pulse wave analysis, vascular calcification (VC) by superficial femoral artery CT and routine bloods were collected. Multiple bone markers (including FGF-23, OPN, OPG, PTH, SOST, IL-1beta) were assayed. Plasma H2S was assayed following conversion to methylene blue using the zinc-dimethyl phenylenediamine trapping method. Patients were assessed at baseline (after antihypertensive (AHT) withdrawal), after AHT reintroduction to BP 130/80mmHg, and after 12 months follow-up. Data are presented as median±IQR or Spearman correlations. Results: Baseline H2S level (2.25±2.42µM) was independent of CKD status, gender and age but lower in smokers (1.77±1.64, 2.43±3.07µM, p=0.037). In those with significant VC (50%), H 2S inversely correlated with VC score (r=-0.427, p=0.026) and arterial stiffness (AIx r=-0.463, p=0.015). Protein-corrected H2S inversely correlated with carotid-femoral PWV (r=-0.408, p=0.039). H2S inversely correlated with PTH (r=-0.297, p=0.038) and, in CKD, with serum calcium (r=0.470, p=0.010). No correlations were seen with vitamin D, phosphate, central haemodynamics or baseline visit bone markers. AHT reintroduction was associated with a significant rise in H2S (2.25±2.42, 4.82±6.15µM, p<0.001), with a trend to a blunted improvement with beta-blockade (1.15±4.49, 4.14±6.03µM, p=0.089). Over 12 months H2S fell (4.82±6.15, 3.74±1.92µM, p=0.005) and VC change inversely correlated with H2S change (r=-0.343, p=0.023). Conclusions: These data support a central role for H2S in both cardiovascular risk and the progression of VC. H2S modulation by AHT therapy suggests a further non-traditional role for both AHT therapy and potentially the choice of agents used.