Centers for Disease Control & Prevention
advertisement
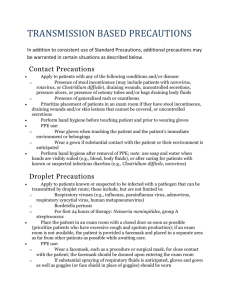
Centers for Disease Control & Prevention Middle East Respiratory Syndrome (MERS) Interim Guidance for Health Professionals: Patients in the U.S. Who Should Be Evaluated Healthcare professionals should evaluate patients for MERS-CoV infection (case definition) If they develop fever (≥38°C, 100.4°F) and pneumonia or acute respiratory distress syndrome (based on clinical or radiological evidence) AND / ANY ONE OF THE FOLLOWING THREE SCENARIOS: 1. Have history of travel from countries in or near the Arabian Peninsula (i.e., Bahrain, Iraq, Iran, Israel, Jordan, Kuwait, Lebanon, Oman, Palestinian territories, Qatar, Saudi Arabia, Syria, the United Arab Emirates [UAE], and Yemen) within 14 days before symptom onset; OR 2. Have had close contact* with a symptomatic traveler who developed fever and acute respiratory illness (not necessarily pneumonia) within 14 days after traveling from countries in or near the Arabian Peninsula; *Close contact is defined as: a. Any person who provided care for the patient, including a healthcare worker or family member, or had similarly close physical contact; or b. Any person who stayed at the same place as the patient (i.e., lived with, visited) while the patient was ill. OR 3. Is a member of a cluster of patients with severe acute respiratory illness (i.e., fever and pneumonia requiring hospitalization) of unknown etiology in which MERS-CoV is being evaluated, in consultation with state and local health departments. Patients who meet the criteria for a MERs CoV investigation should also be evaluated for common causes of community-acquired pneumonia (Examples of respiratory pathogens causing community-acquired pneumonia include influenza A and B, respiratory syncytial virus, Streptococcus pneumoniae, and Legionella pneumophila). This evaluation should be based on clinical presentation and epidemiologic and surveillance information. Testing for MERS-CoV and other respiratory pathogens can be done simultaneously. Positive results for another respiratory pathogen should not necessarily preclude testing for MERS-CoV. Page 1 of 5 Reporting Patients Under Investigation (PUIs) Healthcare professionals should immediately report to their state or local health department any person being evaluated for MERS-CoV infection as a patient under investigation (PUI). Health departments should immediately report PUIs to CDC using the MERS PUI short form below. Middle East Respiratory Syndrome (MERS) Patient Under Investigation (PUI) Short Form o Download PDF file [1 page] o Download Microsoft Word file [1 page] Contact information: Jewish Hospital & St. Mary's Healthcare Infection Prevention and Control: Patricia Gould (JH): 502.587.4870 Kim New (FRI): 502.582.7639 Cathy Pattengale (SMEH): 502.361.6708 Louisville Metro Public Health & Wellness (Jefferson County): 502.574.6570 Bullet County Public Health Dept.: 502.955.7837 Hardin County Public Health Dept.: 1.270.765.6196 KY Department for Public Health Reporting line: 1.888.973.7678 or 1.502.564.3418 Specimen Collection__________________________ For suspected MERS-CoV cases, healthcare providers should collect the following specimens for submission to CDC or the appropriate state public health laboratory: nasopharyngeal swab, oropharyngeal swab (which can be placed in the same tube of viral transport medium), sputum, serum, and stool/rectal swab. CDC recommends collecting multiple specimens from different sites at different times after symptom onset. Recommended infection control precautions should be utilized when collecting specimens. Specimens can be sent using category B shipping containers. Providers should notify their state or local health departments if they suspect MERS-CoV infection in a person. State or local health departments should notify CDC if MERS-CoV infection in a person is suspected. Additional information is available at http://www.cdc.gov/coronavirus/mers/guidelines-clinical-specimens.html. Interim Infection Prevention and Control Recommendations for Hospitalized Patients with Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Standard, contact, and airborne precautions are recommended for management of hospitalized patients with known or suspected MERS-CoV infection. As information becomes available, these recommendations will be re-evaluated and updated as needed. Page 2 of 5 Key Components of Standard, Contact, and Airborne Precautions Recommended for Prevention of MERS-CoV Transmission in U.S. Hospitals For full details of these precautions, see 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Setting. Component Patient Placement Recommendation(s) Airborne Infection Isolation Room (AIIR) Aerosol Generating Procedure Comments If an AIIR is not available, the patient should be transferred as soon as is feasible to a facility where an AIIR is available. Pending transfer, place a facemask on the patient and isolate him/her in a single-patient room with the door closed. The patient should not be placed in any room where room exhaust is recirculated without high-efficiency particulate air (HEPA) filtration. Once in an AIIR, the patient’s facemask may be removed. When outside of the AIIR, patients should wear a facemask to contain secretions Limit transport and movement of the patient outside of the AIIR to medically-essential purposes. Implement staffing policies to minimize the number of personnel that must enter the patient's room. After a potentially infectious patient leaves a room, unprotected individuals, including HCP, should not be allowed in the room until sufficient time has elapsed for enough air changes to remove potentially infectious particles. More information on clearance rates under differing ventilation conditions is available. Use a combination of measures to reduce exposures from aerosol-generating procedures when performed on MERSCoV patients. Limiting the number of HCP present during the procedure to only those essential for patient care and support. Conduct the procedures in a private room and ideally in an AIIR when feasible. Room doors should be kept Although there are limited data available to definitively define a list of aerosol generating procedures, procedures that are usually included are those planned ahead of time, such as bronchoscopy, sputum induction, elective intubation and extubation; and some procedures that often occur in unplanned, emergent settings and can be life-saving, such as Page 3 of 5 closed except when entering or leaving the room, and entry and exit should be minimized during and shortly after the procedure. HCP should adhere to PPE precautions in this interim guidance (i.e., gloves, a gown, and either a face shield that fully covers the front and sides of the face or goggles, and respiratory protection that is at least as protective as a fit-tested N95 filtering facepiece respirator [e.g., powered air purifying or elastomeric respirator]) during aerosol-generating procedures. Conduct environmental surface cleaning following procedures (see section below on environmental infection control). cardiopulmonary resuscitation, emergent intubation, and open suctioning of airways. Once the patient vacates a room where aerosol generating procedures were conducted, unprotected individuals, including HCP, should not be allowed in that room until sufficient time has elapsed for enough air changes to remove potentially infectious particles. More information on clearance rates under differing ventilation conditions is available. Personal Protective Equipment (PPE) for Healthcare personnel (HCP) Gloves Recommended PPE should be Gowns worn by HCP upon entry into patient Eye protection (goggles or face shield) rooms or care areas. Respiratory protection that is at least Upon exit from the patient room as protective as a fit-tested NIOSHor care area, PPE should be removed certified disposable N95 filtering and either facepiece respirator. o Discarded, or o If a respirator is unavailable, a o For re-useable PPE, facemask should be worn. In this cleaned and disinfected according situation respirators should be made to the manufacturer’s reprocessing available as quickly as possible. instructions o Hand hygiene should be performed after removal of PPE Hand Hygiene HCP should perform hand hygiene frequently, including before and after all patient contact, contact with potentially infectious material, and before putting on and upon removal of PPE, including gloves. Healthcare facilities should ensure that supplies for performing hand hygiene are available. Environmental Infection Control Follow standard procedures, per hospital policy and manufacturers’ instructions, for cleaning and/or disinfection of: o Environmental surfaces and equipment o Textiles and laundry Hand hygiene in healthcare settings can be performed by washing with soap and water or using alcoholbased hand rubs. If hands are visibly soiled, use soap and water, not alcohol-based hand rubs. Use EPA-registered hospital disinfectants to disinfect hard nonporous surfaces. o Follow label instructions for use Searchable EPA website of registered products Page 4 of 5 o Food utensils and dishware Page 5 of 5