Blood Bank 3
advertisement

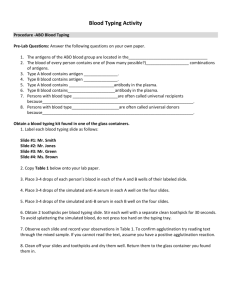
Exp. No.: 2 –cont. ABO System Typing Technique (2) – In-direct (Reverse) Method (Serum Grouping) Background This test is used to confirm and must not substitute the direct grouping that remains the pillar of ABO typing. Reverse grouping is useful in resolving the infrequent but possible dubious or weak results in the direct typing, and it helps to identify the rare cases of false negative and false positive results. The associated Abs; anti-A antibodies and anti-B antibodies are usually IgM antibodies, which are usually produced in the first years of life by exposure to environmental substances such as food, bacteria and/or viruses. Landsteiner′s Rule: ″Individuals who lack particular blood group antigen in their red cells will have antibodies specific to the missing antigen in their plasma″. Principle As focusing on the Landsteiner’s rule above we can imagine; that the presence of a particular Abs in the serum of the tested individual, will indicate IN-DIRECTLY the blood group type, i.e., the presence of anti-A antibody in one individual represents the presence of the opposite antigen on RBCs, so the blood group here will be B. The following table can summarise the overall cases for blood grouping, in regard to the presence/absence of antigens or antibody. Figure -1 (By using known reagent cells A1 and B cells, that expressing identified A and B antigens respectively) Anti-A which present in the plasma of B type will react with A1 cells (A antigen). Anti-B which present in the plasma of A type will react with B cells (B antigen). Anti-A and Anti-B which present in the plasma of O type will react with A and B cells (A and B antigens). Since No Abs present in the plasma of AB type, so NO REACTION WILL OCCURE. Objectives 1. To recognize the reverse/indirect method principle. 2. To be able to interpret the test result that they had. 3. To have the capability of grading the agglutination reactions. Materials Unknown serum or plasma samples for blood group determination, A1 and B cells, small test plastic tubes (10 x 75 or 12 x 75), Centrifuge and Micropipette. Procedure In-direct (Reverse) Tube Method 1. Label two clean test tubes as A1 and B cells. 2. Add 2 drops of plasma (of unknown blood samples) to each tube; (this plasma should be free of hemolysis). 3. Add 1 drop of A1 reagent cells to the tube labeled A1. 4. Add 1 drop of B reagent cells to the tube labeled B. 5. Mix the contents of the tubes gently and centrifuge them at 2500 rpm for 2 min. 6. Examine the serum overlying the cell buttons for evidence of hemolysis. 7. Gently re-suspend the cell buttons and examine them for agglutination. 8. Read, interpret, and record grading of agglutination. 9. Compare serum test results with those obtained in testing red cells. Prepare additional 2 tubes to perform the direct tube ABO grouping method as described previously. Fill the results and interpretation of both forward and reverse methods as in the following table Table -1 Grading of Agglutination Grade Negative (0) Weak (+/-) +1 +2 +3 +4 Description No clumps or aggregates Tiny Clumps or aggregates barely visible be naked eye needs Microscope Few small visible clumps/aggregates Medium size clumps/aggregates Several large clumps/aggregates Only one solid clump/aggregate Table -2 Figure -2 Questions?? 1. Compare and contrast between Reverse and forward method 2. In reverse method the blood fraction tested is? ....... 3. What are the causes of discrepancies between direct and indirect ABO typing? Note It must be remembered that natural anti-A/anti-B may be absent in some physiological or pathological situations: - newborns up to 4-8 months don’t have anti-A or anti-B antibodies - old persons may have a very low titer or absence of detectable anti-A and/or anti-B antibodies - persons that are deeply immunosuppressed because of drugs or of disease may not have detectable Anti-A and/or anti-B The subgroups of the antigen A Blood group A can be divided both serologically and genetically into two distinct subgroups: A1 and A2. Likewise, it was recognized that group AB could be subdivided into A1B and A2B. Approximately 80% of the group A population are of the subgroup A1. The remaining 20% are A2. The same percentages also apply to the group AB. Since the discovery of A1 and A2, many more different subgroups of A have been reported and 12 groups are now known, all showing varying serological and chemical characteristics. The majority of these do not play a significant role in everyday serology. It is possible for people of subgroups A2 and A2B to have anti-A1 in their serum, but this is usually weak and is of no importance in selecting donor blood for transfusion. Weak forms of the B antigen are rare, but may be found in Chinese populations. The following Figure summarizes the subgroups of the antigen A. Table - 3 Anti-A1 and anti-AB in blood grouping tests anti-A Anti-A consists of a mixture of two antibodies: � anti-A which agglutinates A1, A2, A1B and A2B cells � anti-A1 which agglutinates only A1 and A1B cells. Anti-A1 can also be obtained from the seeds of the plant Dolichos biflorus and can be made into an anti-A1 grouping reagent. Table -4 shows the serological reactions with anti-A, anti-AB and anti-A1. Activity What are the possible reasons for the ABO grouping results in the following table Answers 1 Group A with another antibody present, possibly anti-A1 ( B2 Blood group) 2 Group O 3 Group AB with another antibody present, possibly anti-A1 Summary for ABO Reverse Typing This test is used to detect ABO antibodies in an individual's serum, and is used to confirm the ABO Forward Typing. The outcome of the serum typing (Reverse Typing) is compared with the outcome of the cell typing (Forward Typing) to ensure the accurate ABO determination. Any discrepancy must be resolved before final interpretation of the blood group is made. Group A individuals lack the B antigen and their serum will agglutinate the reagent B cells due to their naturally occurring anti-B. Their serum will not agglutinate the reagent A cells since this antigen is present on their own cells. Group B individuals lack the A antigen and their serum will agglutinate A cells with their naturally occurring Anti-A. Their serum will not agglutinate the reagent B cells. Group O individuals lack both A and B antigens and their serum will agglutinate both the A and B reagent red cells. Group O individuals have 3 naturally occurring antibodies in their serum: anti-A, anti-B and anti- AB. Group AB individuals have both A and B antigens on their red cells, and their serum will not agglutinate the A or B reagent red cells. The forward type must correlate with the reverse type and any discrepancy must be resolved. An ABO discrepancy is a situation in which reactions obtained in the forward type DO NOT match or correlate with reactions obtained in the revers type. No blood may be issued for transfusion until the ABO discrepancy has been resolved. If the need is urgent the technician may need to consult with the patient’s physician and the pathologist. The type of discrepancy involved will determine how the situation is to be handled. Reasons for an ABO discrepancies: ! Subgroup of A (A2 or A2B) with anti-A1 - patient forward types as A but agglutinates A R.B.Cs 1 ! Patient may be an infant, elderly or immunodeficient resulting in decreased antibody levels - lack of expected agglutination reactions of reverse cells. ! Unexpected antibodies in the serum -unexpected positive reactions in reverse cells. ! Patient’s red blood cells heavily coated with protein - unexpected positive reactions in forward type. Resolution of ABO discrepancies: 1. Repeat the forward and reverse - this should always be the first course of action. 2. If patient is group A or AB, but reverse types as an O (false positive), test the RBCs with anti-A1. If the patient is A2 or A2B test their serum against A2 cells. Lack of agglutination of the A2 cells indicates that the patient has anti-A1. 3. If the reverse type gives false negative reactions allow the serum and cells to incubate at RT for 5-10 minutes. Respin. False negative reactions are usually due to low levels of antibody being present. The incubation period allows time for additional antibody attachment. 4. False positive results in the forward type may be due to the red blood cells being so heavily coated with Immunoglobulin that the cells spontaneously agglutinate. Perform a DAT, a positive result confirms this as the cause. An extensive work up would be initiated. Transfuse with O negative if this is an emergency or valid typing cannot be determined.