Red Blood Cells
advertisement
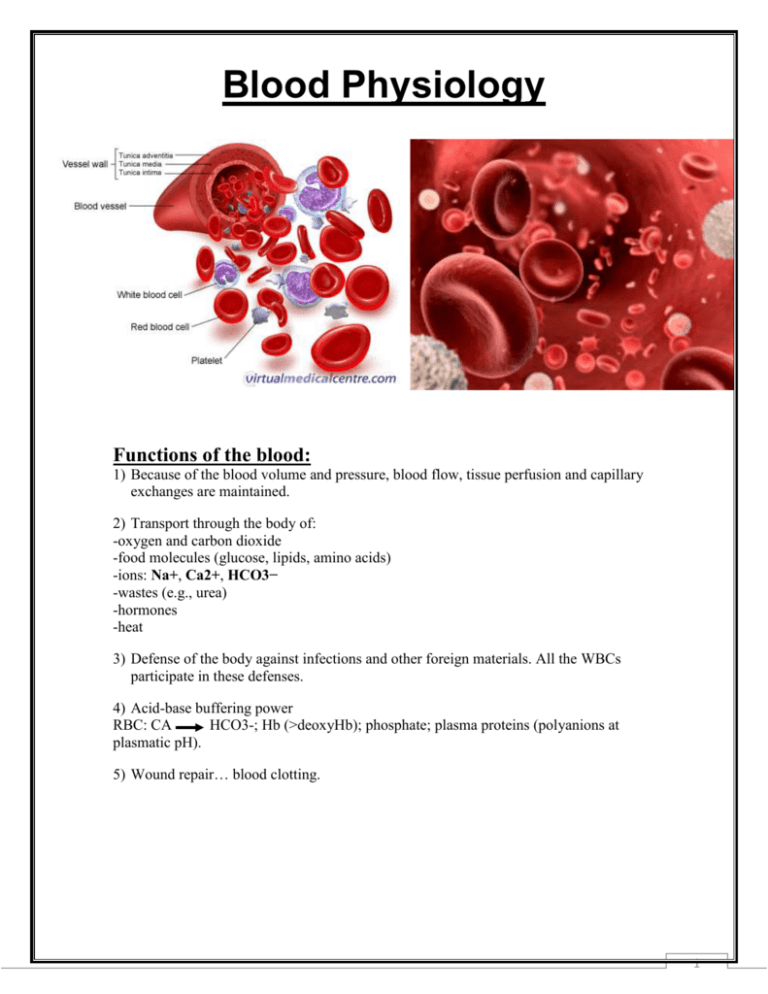
Blood Physiology Functions of the blood: 1) Because of the blood volume and pressure, blood flow, tissue perfusion and capillary exchanges are maintained. 2) Transport through the body of: -oxygen and carbon dioxide -food molecules (glucose, lipids, amino acids) -ions: Na+, Ca2+, HCO3− -wastes (e.g., urea) -hormones -heat 3) Defense of the body against infections and other foreign materials. All the WBCs participate in these defenses. 4) Acid-base buffering power RBC: CA HCO3-; Hb (>deoxyHb); phosphate; plasma proteins (polyanions at plasmatic pH). 5) Wound repair… blood clotting. 1 Blood components: 1 - Blood cells / cell fragments – hematocrit a) Red blood cells (RBCs) or erythrocytes. The fraction occupied by the red cells is called the hematocrit. Normally it is approximately 45%. Values much lower than this are a sign of anemia. b) Platelets or thrombocytes. c) Five kinds of white blood cells (WBCs) or leukocytes - 3 kinds of granulocytes (neutrophils, eosinophils and basophils) - 2 kinds of leukocytes without granules in their cytoplasm (lymphocytes and monocytes). 2- Plasma - plasmatic volume: Plasma is the non-cellular part of the blood and communicates continuously with the interstitial fluid through pores of the capillary membranes. 2 Blood smear: thin film of capillary blood on surface of microscope slide; can be stained with special dyes to show different types of formed elements. Red Blood Cells (Erythrocyte) or "RBC's": Biconcave disk –Optimizes both volume and surface area. Volume important for storage. Surface area important for transport. They have no nuclei or other organelles and only rudimentary enzyme systems. RBCs carry hemoglobin which carries oxygen and carbon dioxide. Hemoglobin molecule Consists of : 1- Protein called globin 2- Non-protein pigment [ heme] which an iron (Fe++) containing pigment part of hemoglobin to which oxygen binds. 3 ABO-Rh Blood Typing With Synthetic Blood: Another important antigen found on the surface of blood cells is the Rh factor, named for the Rhesus monkey in which it was first discovered. Blood containing this antigen is said to be Rh positive (Rh+); blood lacking this antigen is said to be Rh negative (Rh–). The production of an Rh antibody requires exposure to the antigen. Determination of blood group: 1. Using the dropper vial, place a drop of the first synthetic blood sample in each well of the blood typing slide. Replace the cap on the dropper vial. Always replace the cap on one vial before opening the next vial to prevent cross contamination. 2. Add a drop of synthetic anti-A (blue) to the well labeled A. Replace the cap. 3. Add a drop of synthetic anti-B serum (yellow) to the well labeled B. Replace the cap. 4. Add a drop of synthetic anti-Rh serum (clear) to the well labeled Rh. Replace the cap. 5. Using a different color mixing stick for each well (blue for anti-A, yellow for anti-B, white for anti-Rh), gently stir the synthetic blood and anti-serum drops for 30 seconds. Remember to discard each mixing stick after a single use to avoid contamination of your samples. 6. Carefully examine the thin films of liquid mixture left behind. If a film remains uniform in appearance, there is no agglutination. If the sample appears granular, agglutination has occurred. Determine the blood type of the sample using the data table below. Answer yes or no as to whether agglutination occurred in each sample. A positive agglutination reaction indicates the blood type. 7. Record the results for the first blood sample in the data table. 8. Thoroughly rinse the blood typing slide, and then repeat steps 1 through 7 for synthetic blood samples 2, 3, and 4. Sample 1 Sample 2 Sample 3 Sample 4 Yes No Yes No Anti-A No Yes Yes No Anti-B Yes Yes No Yes Rh (Anti-D) A+ B+ AB– O+ Blood Type 4 White Blood Cells (Leukocytes) or "WBC's": - Originate from the same hemocytoblast stem cell as the red cells and platelets. Colorless, have nuclei and granules which can be made visible by staining. 5 Granulocytes: have observable granules when stained. Neutrophils: The most numerous WBCs, making up about 65% of normal white count. These cells are the most important phagocytic cell in the circulation. Also called PMN (polymorphonuclear) neutrophils because of their nuclear shape. These cells spend 8 to 10 days in the circulation making their way to sites of infection etc. Where they are phagocytic and engulf pathogens or debris in the tissues; also release cytotoxic enzymes and chemicals to kill pathogens. Basophils: Important in inflammatory reactions by secreting histamine and a heparin like molecule. Histamine makes blood vessels permeable and heparin inhibits blood clotting. Migrate to sites of injury & cross capillary endothelium to accumulate within damaged (emigration or diapedesis). Tissues arrival enhances local inflammation initiated by mast cells. Eosinophils 2% : Attack objects that have already been coated with antibodies. Phagocytic cells & will engulf antibody-marked bacteria, immune response against parasitic worms, or cellular debris. Sensitive to circulating allergens (materials trigger allergies), eosinophils increase in number during allergic reactions as well. Attracted to sites of injury, where they release enzymes that reduce degree of inflammation & control its spread to adjacent tissues. 6 Agranulocytes: Don’t have observable granules when stained. Monocytes: Monocytes are the biggest of the white blood cells, carry out phagocytosis and are also called macrophages. Produced in the bone marrow. Lymphocytes: 25-30% of all leukocytes; B and T cells provide specific immunity. They are produced in adults in lymph tissue. T (thymus gland-derived) cells - Helper T-cells: recognize antigen, help B-cells to make antibodies and T-cells to kill. - Killer T-cells: poisonous to cells, kill cells infected by viruses and intracellular bacteria. B (bone marrow-derived) cells - originate in the bone marrow. - They recognize free antigen in the body fluids and make antibodies. Platelets (Thrombocytes): Responsible for the intrinsic clotting mechanism. 7