View/Open - Minerva Access
advertisement
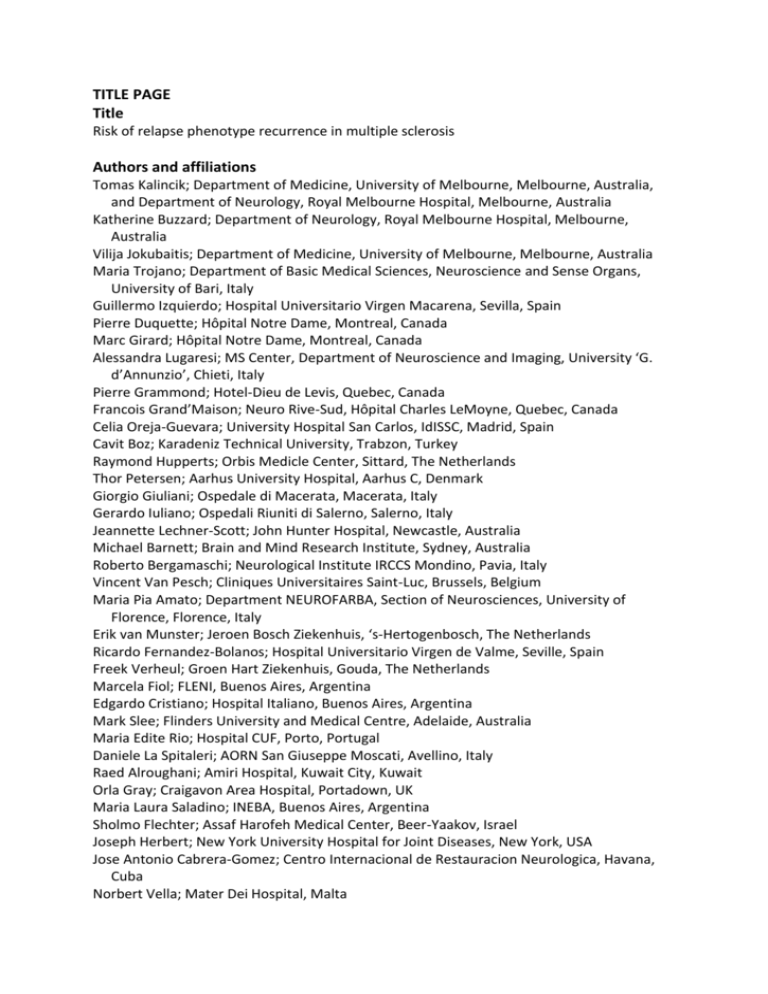
TITLE PAGE Title Risk of relapse phenotype recurrence in multiple sclerosis Authors and affiliations Tomas Kalincik; Department of Medicine, University of Melbourne, Melbourne, Australia, and Department of Neurology, Royal Melbourne Hospital, Melbourne, Australia Katherine Buzzard; Department of Neurology, Royal Melbourne Hospital, Melbourne, Australia Vilija Jokubaitis; Department of Medicine, University of Melbourne, Melbourne, Australia Maria Trojano; Department of Basic Medical Sciences, Neuroscience and Sense Organs, University of Bari, Italy Guillermo Izquierdo; Hospital Universitario Virgen Macarena, Sevilla, Spain Pierre Duquette; Hôpital Notre Dame, Montreal, Canada Marc Girard; Hôpital Notre Dame, Montreal, Canada Alessandra Lugaresi; MS Center, Department of Neuroscience and Imaging, University ‘G. d’Annunzio’, Chieti, Italy Pierre Grammond; Hotel-Dieu de Levis, Quebec, Canada Francois Grand’Maison; Neuro Rive-Sud, Hôpital Charles LeMoyne, Quebec, Canada Celia Oreja-Guevara; University Hospital San Carlos, IdISSC, Madrid, Spain Cavit Boz; Karadeniz Technical University, Trabzon, Turkey Raymond Hupperts; Orbis Medicle Center, Sittard, The Netherlands Thor Petersen; Aarhus University Hospital, Aarhus C, Denmark Giorgio Giuliani; Ospedale di Macerata, Macerata, Italy Gerardo Iuliano; Ospedali Riuniti di Salerno, Salerno, Italy Jeannette Lechner-Scott; John Hunter Hospital, Newcastle, Australia Michael Barnett; Brain and Mind Research Institute, Sydney, Australia Roberto Bergamaschi; Neurological Institute IRCCS Mondino, Pavia, Italy Vincent Van Pesch; Cliniques Universitaires Saint-Luc, Brussels, Belgium Maria Pia Amato; Department NEUROFARBA, Section of Neurosciences, University of Florence, Florence, Italy Erik van Munster; Jeroen Bosch Ziekenhuis, ‘s-Hertogenbosch, The Netherlands Ricardo Fernandez-Bolanos; Hospital Universitario Virgen de Valme, Seville, Spain Freek Verheul; Groen Hart Ziekenhuis, Gouda, The Netherlands Marcela Fiol; FLENI, Buenos Aires, Argentina Edgardo Cristiano; Hospital Italiano, Buenos Aires, Argentina Mark Slee; Flinders University and Medical Centre, Adelaide, Australia Maria Edite Rio; Hospital CUF, Porto, Portugal Daniele La Spitaleri; AORN San Giuseppe Moscati, Avellino, Italy Raed Alroughani; Amiri Hospital, Kuwait City, Kuwait Orla Gray; Craigavon Area Hospital, Portadown, UK Maria Laura Saladino; INEBA, Buenos Aires, Argentina Sholmo Flechter; Assaf Harofeh Medical Center, Beer-Yaakov, Israel Joseph Herbert; New York University Hospital for Joint Diseases, New York, USA Jose Antonio Cabrera-Gomez; Centro Internacional de Restauracion Neurologica, Havana, Cuba Norbert Vella; Mater Dei Hospital, Malta Mark Paine; St Vincent’s Hospital, Melbourne, Australia Cameron Shaw; Geelong Hospital, Geelong, Australia Fraser Moore; Jewish General Hospital, Montreal, Canada Steve Vucic; Westmead Hospital, Sydney, Australia Aldo Savino; Consultorio Privado, Buenos Aires, Argentina Bhim Singhal; Bombay Hospital Institute of Medical Sciences, Mumbai, India Tatjana Petkovska-Boskova; Clinic of Neurology Clinical Center, Skopje, Macedonia John Parratt; Royal North Shore Hospital, Sydney, Australia Carmen-Adella Sirbu; Central Clinical Emergency Military Hospital, Bucharest, Romania Csilla Rozsa; Jahn Ferenc Teaching Hospital, Budapest, Hungary Danny Liew; Melbourne EpiCentre, University of Melbourne and Melbourne Health, Melbourne, Australia Helmut Butzkueven; Department of Medicine, University of Melbourne, Melbourne, Australia, Department of Neurology, Royal Melbourne Hospital, Melbourne, Australia, and Department of Neurology, Box Hill Hospital, Monash University, Box Hill, Australia on behalf of the MSBase Study Group* *Contributing members of the MSBase Study Group are listed in the Acknowledgements. Keywords multiple sclerosis, presentation of neurological diseases, phenotype, prognosis, MSBase Corresponding author Tomas Kalincik; L4 Centre, Melbourne Brain Centre at Royal Melbourne Hospital, Grattan St, Parkville VIC 3050, Australia; Tel: +61 3 9342 4404, Fax: +61 3 9349 5997 ABSTRACT Objectives To analyse risk of relapse phenotype recurrence in MS and to characterise the effect of demographic and clinical features on this phenotype. Methods Information about relapses was collected using MSBase, an international observational registry. Associations between relapse phenotypes and history of similar relapses or patient characteristics were tested with multivariable logistic regression models. Tendency of relapse phenotypes to recur sequentially was assessed with principal component analysis. Results Among 14,969 eligible patients (89,949 patient-years), 49,279 phenotypically characterised relapses were recorded. Visual and brainstem relapses occurred more frequently in early disease and in younger patients. Sensory relapses were more frequent in early or nonprogressive disease. Pyramidal, sphincter and cerebellar relapses were more common in older patients and in progressive disease. Women presented more often with sensory or visual symptoms. Men were more prone to pyramidal, brainstem and cerebellar relapses. Importantly, relapse phenotype was predicted by the phenotypes of previous relapses. (OR=1.8-5, p=10-14). Sensory, visual and brainstem relapses showed better recovery than other relapse phenotypes. Relapse severity increased and the ability to recover decreased with age or more advanced disease. Conclusion Relapse phenotype was associated with demographic and clinical characteristics, with phenotypic recurrence significantly more common than expected by chance. INTRODUCTION Clinical relapses in MS can result in residual functional impairment [1, 2] and may lead to long-term accumulation of disability [3-5]. They have a significant impact on patients’ quality of life and employability and contribute to healthcare-related expenses. Therefore, reduction of relapse frequency is a common primary outcome in clinical trials of immunomodulatory agents. In some demyelinating diseases, such as neuromyelitis optica, relapses occur almost exclusively in specific neuroanatomical regions. However, in MS, our knowledge of relapse phenotype recurrence is limited. It is the experience of many clinicians that patients presenting with certain symptoms or signs experience further relapses with a similar phenotype. This clinical impression was substantiated in a single-centre study of 195 patients, showing an increased recurrence risk of phenotypically similar first and second relapses after a first attack [6]. More specifically, this association was apparent for relapses affecting the spinal cord, optic nerve, brainstem and cerebellum. In this study, we used the international MSBase registry dataset [7] to assess the risk of phenotypic relapse recurrence in a large, representative MS population, with long-term, prospectively acquired follow-up data. We examined recurrence relationships between various relapse phenotypes and characterised relapse patterns in relation to clinical and demographic data. PATIENTS AND METHODS Data collection in the MSBase registry [7] was approved by the Melbourne Health Human Research Ethics Committee, and by the local ethics committees in all participating centres (or exemptions granted, according to applicable local laws and regulations). Written informed consent was obtained from enrolled patients as required. Longitudinal clinical data from 18,885 patients from 55 MS centres in 25 countries were extracted from the MSBase registry in February 2012. Inclusion criteria consisted of a diagnosis of MS or clinically isolated syndrome (CIS) and availability of minimal dataset. The minimal dataset consisted of patient date of birth, sex, MS centre, dates of MS onset and clinical follow-up, disease course at inclusion and censoring, dates of disease modifying therapy and list of clinical relapses (including date of onset, clinical presentation and treatment status). Expanded Disability Status Scale (EDSS) score at inclusion and censoring was not required. Patients with primary progressive MS were excluded. The analysed data were recorded as part of routine clinical practice, with real time or nearreal time data entry in relation to clinical visits. Relapse information was recorded when reported by patients, however, retrospective entry of pre-MSBase relapses was allowed. The MSBase protocol stipulates minimum annual updates of the minimum dataset, but patients with less frequent visits were not excluded. Data entry portal was either the iMed clinical record system or the MSBase online data entry system. Data quality assurance procedures are described elsewhere [8]. MS course was classified by treating neurologists as CIS, relapsing-remitting MS (RRMS), secondary progressive MS (SPMS) or relapsing-progressive MS (RPMS). Progressive MS was defined by continuous clinical progression over at least one year. Onset of progressive phase was identified by participating neurologists. Disability was assessed by accredited scorers using EDSS (Neurostatus certification was required at each centre). A clinical relapse was defined as occurrence of new symptoms or exacerbation of existing symptoms persisting for at least 24 hours, in the absence of concurrent illness or fever, and occurring at least 30 days after a previous relapse [9]. For the purpose of this study, the initial attack was referred to as a relapse. For all analysed relapses, new or worsening signs/symptoms were classified according to functional domains defined by Kurtzke[10]. Formal scoring of relapseassociated disability was not required. A proportion of relapses were classified by the clinicians as mild, moderate or severe, as described elsewhere [11], and the presence/absence of their impact on activities of daily living was reported by patients. In a subset of relapses, clinical recovery was evaluated by the neurologists as complete or incomplete. Treatment of relapses with glucocorticoids was recorded. Statistical analysis was carried out using Statistica 10 (Statsoft, Tulsa, USA) and R (http://www.R-project.org). All hypotheses were tested at two-tailed 0.05 level of significance, after applying Benjamini-Hochberg correction for multiple hypothesis testing. To evaluate independent determinants of relapse phenotype, a multivariable logistic regression model was built for each functional system, with the relapse phenotype (dichotomised as present/absent) as the dependent variable and sex, age, MS duration, MS course and presence/absence of phenotypically similar previous relapses as independent predictors. A separate series of multivariable logistic regression models were used to evaluate independent determinants of relapse severity (mild/moderate/severe), impact on activities of daily living (present/absent) and recovery (complete/incomplete), with the tested candidate determinants being sex, age, MS duration, MS course and relapse phenotype. Effect of total number of previous relapses was evaluated in a separate multivariable logistic models. In the subpopulation of patients followed in MSBase from CIS and at least one relapse following the initial episode, a multivariable logistic model was built to evaluate the initial relapse phenotype as a determinant of the subsequent dominant (i.e. the most frequent) relapse phenotype. Multiple dominant phenotypes were allowed where several phenotypes were tied. The dependent variable (dichotomised) indicated convergence between the phenotypes of the initial and the subsequent relapses, with independent predictors comprising sex, age and relapse phenotype. All models were adjusted for MS-specific therapy, centre and date of relapse onset, and the analysis of recovery was adjusted for steroid therapy (present/absent). Goodness of model fit was evaluated with Akaike Information Criterion. Principal component analysis was used to identify the likelihood of coincidence of relapse phenotypes in individual patients over the course of MS. For each patient the overall number of relapses was recorded for each phenotype. Components were identified by an eigenvalue>1, explaining at least 15% of the variance in the model and containing at least two variables with loadings>0.5‡. RESULTS Patients and relapses Of the 18,885 patients with data in the MSBase registry in February 2012, data from 14,969 patients and 89,949 patient-years were retained (Figure 1). The number of eligible patients per centre varied between 20 and 1340. Population characteristics are shown in Table 1 and Supplementary Figure 1. Relapse phenotypes by country are shown in Supplementary Table 1. Overall, 49,279 relapses with recorded presenting symptoms were analysed (3.83.2 (meanstandard deviation) per patient; Table 2). The majority of relapses were monosymptomatic (71.4%) and presented with sensory, pyramidal, visual or brainstem symptoms/signs. ---- Figure 1------- Table 1------- Table 2---- Relapse phenotypes Figure 2 shows relapse phenotypes stratified by demographic and clinical features. Table 3 summarises outcomes of the respective multivariable logistic models. Pyramidal, cerebellar or brainstem relapses occurred more commonly in men (odds ratio (OR)=1.1, p≤0.03), visual or sensory relapses were more frequent in women (OR=1.13, p≤0.02). Older age was positively associated with pyramidal and bowel/bladder relapses (OR=1.02, p≤10-8), and negatively associated with visual and brainstem relapses (OR=0.98-0.99, p≤0.008). Longer MS duration was positively associated with cerebellar relapses (OR=1.02, p=0.046) and negatively associated with visual, sensory and brainstem relapses (OR=0.94-0.99, p≤0.023). Compared to the relapses recorded in RRMS, CIS more commonly affected the visual system (OR=2.04, p=0.048). SPMS was positively associated with bowel/bladder relapses (OR=2.46, p=10-5), and negatively associated with brainstem and cerebellar relapses (OR=0.26-0.28, p≤0.05). The relatively rare RPMS was negatively associated with visual, sensory and brainstem relapses (OR=0.39-0.63, p<10-6), and positively associated with pyramidal, bowel/bladder, cerebellar and cognitive relapses (OR=2.05-2.82, p<10-4). Disease modifying therapy at the time of relapse did not have a significant impact on relapse phenotype. ---- Figure 2------- Table 3---- Relapse recurrence Relapses were significantly more likely to present with the same phenotype as the preceding relapses (OR=1.8-5, p=10-14; Table 3), regardless of the number of previous relapses. In patients with data recorded from CIS and 2 recorded relapses (7612, 72% women, age 30±10 years), we examined associations between the initial relapse and the most frequent subsequent relapse phenotype. We observed a significantly increased likelihood of the subsequent relapses to affect the same neurological system as the initial relapse for visual, pyramidal, sensory, cerebellar and brainstem relapses (Table 4). This association was most pronounced for sensory (OR=7.71) and pyramidal relapses (OR=4.99, p=10-15). We also conducted a principal component analysis to identify patterns of relapse phenotypes which were likely to occur in conjunction or consecutively in individual patients over the course of MS. The analysis identified a single component explaining 31% of variance in relapse phenotypes (eigenvalue 2.15). This component consisted of pyramidal (loading 0.68‡) and bowel/bladder (0.65) relapses, followed by sensory (0.59), cerebellar (0.56) and brainstem (0.54) relapses, and finally by cognitive (0.41) and visual (0.39) relapses (Supplementary Figure 2), suggesting that the closest associations exist between pyramidal, bowel/bladder and sensory phenotypes. ---- Table 4---- ---- Table 5---- Relapse severity, impact and recovery Information about clinical severity was available for 17,282 relapses (35%). The availability of information about severity was proportional across the phenotypes (34-45%), with the exception of cognitive relapses, where it reached 59%. Apart from sensory relapses, all other relapses were more likely to be classified as moderate or severe rather than mild (OR=1.15-2.98, p≤0.042; Table 5). In addition, moderate relapse severity was positively associated with patient age (OR=1.01, p=0.013) and negatively associated with female sex (OR=0.95, p=0.042). Both moderate and severe relapses were less frequent in CIS compared to RRMS (OR=0.44-0.71, p≤0.003). With the exception of sensory relapses (OR=0.91, p=0.017), all other relapse phenotypes were likely to impact on activities of daily living (OR=1.29-2.97, p≤0.012), with pyramidal and cerebellar relapses having the most prominent impact. The relapses with significant impact on daily activities were more common among patients with longer disease duration (OR=1.01, p=0.049) and were less common in CIS (OR=0.59, p=0.0001). Pyramidal, bowel/bladder, cognitive and cerebellar relapses had increased risk of incomplete recovery resulting in residual disability (OR=1.34-1.40, p≤10-6; adjusted for corticosteroid treatment). In contrast, brainstem relapses were more likely to recover without clinical residuum (OR=0.91, p=10-5). Incomplete recovery was more common in SPMS (OR=1.52, p=0.0007) and RPMS (OR=2.24, p=10-10) compared to RRMS and less common in CIS (OR=0.58, p=10-8) and in females (OR=0.96, p=0.012). The likelihood of incomplete recovery increased independently with age (OR=1.03, p<10-15) and number of previous relapses (OR=1.04, p=10-8) but not with disease duration (p=0.4). DISCUSSION Using data from approximately 15,000 patients representing almost 90,000 patient-years recorded in the observational international MSBase registry and representative of MS population managed in academic MS centres, we have examined trends in clinical presentations of MS relapses. We have shown that relapses tend to recur within previously affected neurological domains. Sensory, pyramidal, visual, brainstem or cerebellar initial relapses are predictive of the predominant phenotype of future relapses. Our observations confirm and extend prior published work. In a cohort of 195 patients, Mowry and colleagues showed that CIS relapses localised to the spinal cord, optic nerve or brainstem/cerebellum were commonly followed by relapses of similar phenotype [6]. In addition, relapses in patients on first-line immunomodulatory therapy were often preceded by similar pre-treatment relapses [12]. Our principal component analysis suggested that the relapse phenotypes occurring consecutively in individual patients are most likely to affect anatomically related functions. The most significant associations were found between pyramidal, bowel/bladder and sensory relapses. This is strongly suggestive of their co-localisation in the spinal cord. It could be hypothesised that anatomical distribution of inflammatory activity is an inherent property of individual MS phenotype with a great inter-individual variability. This view is supported by several studies demonstrating associations between lesion distribution and genetic or immunological variables [13-15]. Cumulative structural damage resulting from previous relapses might diminish local functional reserve and thus enhance the impact of any further inflammatory activity on the previously affected neurological networks. Autopsy studies have shown that demyelination commonly occurs in previously remyelinated areas and may represent a pathological correlate of disability progression [16, 17]. In support of this concept, accrual of persistent disability within the visual, pyramidal, sensory or cerebellar systems is commonly preceded by clinical relapses within corresponding anatomical locations [18]. The phenotype of CIS has previously been characterised [19]. However, a complex evaluation of clinical relapse presentations, severity, impact and recovery, with detailed analysis capturing the full spectrum of MS courses, duration and patient demography has not been performed. In this study we have shown that relapse patterns vary according to age, sex, MS course and MS duration. Compared to the relapses in clinically definite MS, initial events are more likely to involve visual function. In a population-based sample of 1424 patients, Cossburn and colleagues reported the following proportions of the initial events: visual 18%, long tract 47%, cerebellar 10%, brainstem 10%, cerebral 1% and polyregional 11% [19]. Our observations generally confirm these results (see Table 4). However, a direct comparison between the two studies is not possible due to differing clinical classification of relapses. The likelihood of visual relapses decreases with longer MS duration, older patient age and more progressive MS course. This is also in agreement with the previously cited work, which showed that optic neuritis as an initial event is most common among children and decreases with age [19]. A similar pattern is apparent for the relapses affecting brainstem functions. Additionally, the likelihood of sensory relapses decreases with MS duration and is also lower in RPMS. In contrast, the risk of pyramidal and bowel/bladder relapses increases with more progressive disease course and older age. Here again, our observations are in agreement with those of Cossburn, who reported agedependent increase in the incidence of CIS affecting sphincter, sexual and locomotor functions [19]. The likelihood of cerebellar relapses increases with MS duration and is higher in RPMS. It should be noted that the higher proportion of cerebellar relapses in SPMS compared to RRMS seen in unadjusted data is most likely driven by other confounders (such as sex, age and MS duration) as the statistical models showed a negative independent association. In our cohort, sensory and bowel/bladder relapses were disproportionately low and pyramidal, cerebellar and brainstem relapses were high among children younger than 10 years. With the exception of cognitive relapses, our results are similar to those reporting 245 relapses from 105 MS patients younger than 18 years: visual 24-26%, spinal cord 3641%, brainstem/cerebellar 39-51% and cerebral 9-11% [20]. This phenomenon could be attributed to underreporting of sensory and sphincter presentations in paediatric patients. We have shown that relapses are more likely to present with sensory or visual symptoms in women, and with pyramidal, brainstem or cerebellar symptoms in men. It is of interest that sensory relapses are less likely to interfere with activities of daily living and both sensory and visual relapses are less likely to result in incomplete recovery. Therefore we may expect that women should present with milder relapses with a better prospect of recovery compared to men, an assumption which has been confirmed by our data. We and others previously demonstrated that relapses are more frequent among women than in men [21, 22] and that higher relapse frequency early in the disease course is associated with less favourable disability outcomes [4, 24, 25]. In contrast, several other studies suggested that male sex predisposes to poorer long-term disease outcomes [25, 26]. This seemingly conflicting evidence could potentially be explained by the impact of relapse severity and recovery on disability outcomes. It has been shown that more severe relapses are less likely to recover completely [27] and that a poor recovery from relapses leads to more pronounced disability accrual [2, 25, 28, 29]. Therefore, we can speculate that women, who are more likely to experience more frequent but less severe relapses with better recovery, will also show better long-term disease outcomes than men. We have observed that relapses with higher impact and poorer recovery were associated with longer MS duration, progressive disease course or older age. With the exception of age, these observations are in agreement with previously published data [19, 30]. In addition, sensory relapses are of relatively lower severity and impact, and together with visual and brainstem relapses are relatively less likely to result in incomplete recovery compared to the other relapse phenotypes. A potential limitation of our study is the quality of the data collected within MSBase, which is likely to be lower in an observational registry than in a clinical trial. Recall bias could play a role in an observational database, where the relapse information is usually recorded retrospectively at the clinical visit following the onset of the relapse. In addition, underreporting of relapses could conceivably confound results but would have to occur differentially to do so. Reassuringly, our previous work studying incidence of relapses in MSBase, which used a cohort largely overlapping with the cohort used in our present analysis [21], showed annual relapse rates which were similar to the relapse rates in the recent randomised controlled trials (0.3-0.4 within the initial 10 years from disease onset)[31, 32]. Given the reporting of relapses may change over time, we adjusted all analyses for relapse date. Further variance could potentially be introduced by the differences in clinical classification of relapses between evaluating physicians. In relation to disability severity and phenotype, patients may be biased in reporting certain relapse phenotypes. In a large proportion of relapses the information about severity, impact and recovery was not recorded, and where available, this information was based on subjective assessment. Preferential recording of this information in relapses with specific presentation or severity, or in specific disease course could have potentially confounded the analysis. Finally, the studied population was representative of patient populations managed at large academic MS centres, which may impact on the generalisation of our observations. In conclusion, the demonstrated propensity of relapses to occur in previously affected systems could reflect increased vulnerability of previously demyelinated CNS regions to further autoimmune attacks [16, 17, 33]. The increased likelihood of men to suffer pyramidal relapses, especially as these are also likely to be recurrent, may at least partially explain the widely reported worse disability progression outcomes in men. We plan to examine this relationship in future work. In spite of increased risk of phenotypic recurrence in individual patients’ relapses, there is also a completely unexplained decrease in the proportion of visual relapses and a concomitant increase in the proportion of pyramidal and sphincter relapses with older age, longer disease duration and in progressive MS. Discovery of a neurobiological substrate for this shift could have major implications for our understanding of MS pathogenesis. ACKNOWLEDGEMENTS MSBase study group contributors: From the MS-Centrum Nijmegen, Nijmegen, The Netherlands Dr Cees Zwanikken; from the Centre hospitalier del’Universite de Montreal, Hopital Notre-Dame, Canada, Dr Elaine Roger and Dr Pierre Despault; from the Royal Melbourne Hospital, Australia, Dr Mark Marriott, Dr Anneke Van der Walt, Dr John King, Dr Jill Byron, Ms Lisa Morgan and Ms Eloise Hansen; from Box Hill Hospital, Monash University, Australia, Dr Olga Skibina and Ms Jodi Haartsen; from Department of Neuroscience and Imaging, University ‘G. d’Annunzio’, Italy, Dr Giovanna De Luca, Dr Valeria Di Tommaso, Dr Daniela Travaglini, Dr Erika Pietrolongo, Dr Maria di Ioia and Dr Deborah Farina; from Hospital Italiano, Italy, Dr Juan Ignacio Rojas and Dr Liliana Patrucco; from Hopital Tenon, Paris, France, Dr Etienne Roullet; from FLENI, Argentina, Dr Jorge Correale and Dr Celica Ysrraelit; from Ospedale di Macerata, Italy, Dr Elisabetta Cartechini and Mr Eugenio Pucci; from John Hunter Hospital, Australia, Dr David Williams and Dr Lisa Dark; from Sheba Medical Center, Tel Hashomer, Israel, Dr Joab Chapman; from Jahn Ferenc Teaching Hospital, Hungary, Dr Krisztian Kasa; from Francicus Ziekenhuis, Roosendaal, The Netherlands, Ms Leontien den Braber-Moerland; from Al-Zahra Hospital, Isfahan, Iran, Dr Vahid Shaygannejad; from Multiple Sclerosis Centre Kamillus-Klinik, Asbach, Germany, Dr Dieter Poehlau; from Hospital Ecoville, Curitiba, Brazil, Dr Walter Oleschko Arruda; and from Hospital Angeles Mexico City, Lomas, Mexico, Dr Eli Skromne. Funding acknowledgement: The work was supported by the Multiple Sclerosis Research Australia Postdoctoral Fellowship [grant number 11-054] and NHMRC Early Career Fellowship (Clinical) to TK [grant number 1071124]; NHMRC Career Development Award (Clinical) to HB [grant number 628856]; NHMRC Project Grant [grant number 1032484]; NHMRC Centre for Research Excellence [grant number 1001216] and the MSBase Foundation. The MSBase Foundation is a not-for-profit organization that receives support from Merck Serono, Biogen Idec, Novartis Pharma, Bayer-Schering, Sanofi-Aventis and BioCSL. CONFLICT OF INTEREST STATEMENT Aldo Savino did not declare any competing interests. Alessandra Lugaresi is a Bayer Schering, Biogen Idec, Genzyme, Merck Serono Advisory Board Member. She received travel grants and honoraria from Bayer Schering, Biogen Idec, Merck Serono, Novartis, Sanofi Aventis and Teva, research grants from Bayer Schering, Biogen Idec, Merck Serono, Novartis, Sanofi Aventis and Teva, travel and research grants from the Associazione Italiana Sclerosi Multipla. Bhim Singhal received consultancy honoraria and compensation for travel from Biogen-Idec and Merck-Serono. Cameron Shaw did not declare any competing interests. Carmen-Adella Sirbu received speaking honoraria from Teva, and travel grants from BayerSchering and Teva. Cavit Boz has received travel grants from Merck Serono, Biogen Idec, Novartis, BayerSchering, Merck-Serono and Teva; has participated in clinical trials by Sanofi Aventis, Roche and Novartis. Celia Oreja-Guevara received honoraria as consultant on scientific advisory boards from Biogen-Idec, Bayer-Schering, Merck-Serono, Teva and Novartis; has participated in clinical trials/other research projects by Biogen-Idec, GSK, Teva and Novartis. Csilla Rozsa has received speaker honoraria from Bayer Schering, Novartis and Biogen Idec, congress and travel expense compensations from Biogen Idec, Teva, Merck Serono and Bayer Schering. Daniele La Spitaleri received honoraria as a consultant on scientific advisory boards by Bayer-Schering, Novartis and Sanofi-Aventis and compensation for travel from Novartis, Biogen Idec, Sanofi Aventis, Teva and Merck-Serono. Danny Liew did not declare any competing interests. Edgardo Cristiano received honoraria as consultant on scientific advisory boards by BiogenIdec, Bayer-Schering, Merck-Serono, Genzyme and Novartis; has participated in clinical trials/other research projects by Merck-Serono, Roche and Novartis. Elizabeth Alejandra Bacile Bacile did not declare any competing interests. Erik van Munster did not declare any competing interests. Francois Grand’Maison received honoraria from Biogen Idec, Genzyme, Novartis and Roche. Fraser Moore has participated in clinical trials sponsored by EMD Serono and Novartis. Freek Verheul is an advisory board member for Teva Biogen Merck Serono and Novartis. Gerardo Iuliano had travel/accommodations/meeting expenses funded by Bayer Schering, Biogen Idec, Merck Serono, Novartis, Sanofi Aventis, and Teva Giorgio Giuliani did not declare any competing interests. Guillermo Izquierdo received speaking honoraria from Biogen-Idec, Novartis, Sanofi, Serono and Teva. Helmut Butzkueven has served on scientific advisory boards for Biogen Idec, Novartis and Sanofi-Aventis and has received conference travel support from Novartis, Biogen Idec and Sanofi Aventis. He serves on steering committees for trials conducted by Biogen Idec and Novartis, and has received research support from Merck Serono, Novartis and Biogen Idec. Jeannette Lechner-Scott has accepted travel compensation from Novartis, Biogen and Merck Serono. Her institution receives the honoraria for talks and advisory board commitment and also clinic support from Bayer Health Care, Biogen Idec, CSL, Genzyme Sanofi, Merck Serono and Novartis. Jose Antonio Cabrera-Gomez did not declare any competing interests. Joseph Herbert did not declare any competing interests. Katherine Buzzard has received travel compensation from Sanofi-Aventis and Genzyme. Marc Girard received consulting fees from Teva Canada Innovation, Biogen Idec, Novartis and Genzyme Sanofi; lecture payments from Teva Canada Innovation, Novartis and EMD Serono. Dr Girard has also received a research grant from Canadian Institutes of Health Research. Marcela Fiol received honoraria from Merck-Serono and Bayer. Maria Edite Rio did not declare any competing interests. Maria Laura Saladino did not declare any competing interests. Maria Pia Amato received honoraria as consultant on scientific advisory boards by BiogenIdec, Bayer-Schering, Merck-Serono, Teva and Sanofi-Aventis; has received research grants by Biogen-Idec, Bayer-Schering, Merck-Serono, Teva and Novartis. Maria Trojano received speaking honoraria from Biogen-Idec, Bayer-Schering, Sanofi Aventis, Merck-Serono, Teva and Novartis; has received research grants from Biogen-Idec, Merck-Serono, and Novartis. Mark Paine did not declare any competing interests. Mark Slee has participated in, but not received honoraria for, advisory board activity for Biogen Idec, MerckSerono, BayerSchering, Sanofi Aventis and Novartis. Merilee Needham has received honoraria as a consultant from Novartis. Michael Barnett has served on scientific advisory boards for Biogen-Idec, Novartis and Genzyme and has received conference travel support from Biogen-Idec and Novartis. He serves on steering committees for trials conducted by Novartis. His institution has received research support from Biogen-Idec, Merck-Serono and Novartis. Norbert Vella received compensation for travel and honoraria from Novartis, Biogen Idec, Glaxo-Smith-Kline. Norma Deri received funding from Bayer, Merck Serono, Biogen Idec, Genzyme and Novartis. Orla Gray received honoraria as consultant on scientific advisory boards for Biogen Idec, Merck Serono and Novartis; has received travel grants from Biogen Idec, Merck Serono and Novartis; has participated in clinical trials by Biogen Idec and Merck Serono. Pierre Duquette did not declare any competing interests. Pierre Grammond is a Novartis, Teva-neuroscience, Biogen Idec advisory board member, consultant for Merck Serono, received payments for lectures by Merck Serono, TevaNeuroscience and Canadian Multiple sclerosis society, and received grants for travel from Teva-Neuroscience and Novartis. Raed Alroughani received honororia from Biologix, Bayer, Merck Sorono, GSK and Novartis, and served on advisory board for Biologix, Novartis and Merck Sorono. Raymond Hupperts received honoraria as consultant on scientific advisory boards from Merck-Serono, Biogen-Idec, Genzyme-Sanofi and Teva, research funding from Merck-Serono and Biogen-Idec, and speaker honoraria from Sanofi-Genzyme. Ricardo Fernandez-Bolanos did not declare any competing interests. Roberto Bergamaschi received speaker honoraria from Bayer Schering, Biogen, Novartis, Sanofi-Aventis, Teva; research grants from Bayer Schering, Biogen, Novartis, Sanofi-Aventis, Teva; congress and travel expense compensations from Bayer Schering, Biogen, Novartis, Sanofi-Aventis, Teva. Santiago Vetere did not declare any competing interests. Sholmo Flechter did not declare any competing interests. Steve Vucic did not declare any competing interests. Tatjana Petkovska-Boskova did not declare any competing interests. Thor Petersen received funding or speaker honoraria from Biogen Idec, Merck Serono, Novartis, Bayer Schering, Sanofi-Aventis, Roche, and Genzyme. Tomas Kalincik received compensation for travel from Novartis, Biogen Idec, Sanofi Aventis, Teva and Merck Serono. Vilija Jokubaitis has received conference travel support from Novartis. Vincent Van Pesch has served on advisory boards for Biogen Idec and Genzyme; has received travel grants from Biogen Idec, Bayer Schering, Sanofi Aventis, Merck Serono and Novartis Pharma ; has received consultancy fees from Biogen Idec, Teva and Novartis Pharma; has received research grants from Bayer Schering. NOTES ‡ The loadings indicate the relative contribution of each variable (relapse phenotype) to the principal component. REFERENCES 1. Hirst C, Ingram G, Pearson O, Pickersgill T, Scolding N, Robertson N. Contribution of relapses to disability in multiple sclerosis. J Neurol 2008;255(2):280-7. 2. Lublin FD, Baier M, Cutter G. Effect of relapses on development of residual deficit in multiple sclerosis. Neurology 2003;61(11):1528-32. 3. Scalfari A, Neuhaus A, Degenhardt A, Rice GP, Muraro PA, Daumer M, et al. The natural history of multiple sclerosis: a geographically based study 10: relapses and long-term disability. Brain 2010;133(Pt 7):1914-29. 4. Kalincik T, Vaneckova M, Tyblova M, Krasensky J, Seidl Z, Havrdova E, et al. Volumetric MRI Markers and Predictors of Disease Activity in Early Multiple Sclerosis: A Longitudinal Cohort Study. PLoS One 2012;7(11):e50101. 5. Lhermitte F, Marteau R, Gazengel J, Dordain G, Deloche G. The frequency of relapse in multiple sclerosis. A study based on 245 cases. Zeitschrift für Neurologie 1973;205(1):47-59. 6. Mowry EM, Deen S, Malikova I, Pelletier J, Bacchetti P, Waubant E. The onset location of multiple sclerosis predicts the location of subsequent relapses. J Neurol Neurosurg Psychiatry 2009;80(4):400-3. 7. Butzkueven H, Chapman J, Cristiano E, Grand'Maison F, Hoffmann M, Izquierdo G, et al. MSBase: an international, online registry and platform for collaborative outcomes research in multiple sclerosis. Mult Scler 2006;12(6):769-74. 8. Kalincik T, Spelman T, Trojano M, Duquette P, Izquierdo G, Grammond P, et al. Persistence on Therapy and Propensity Matched Outcome Comparison of Two Subcutaneous Interferon Beta 1a Dosages for Multiple Sclerosis. PLoS One 2013;8(5):e63480. 9. McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 2001;50(1):121-7. 10. Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983;33(11):1444-52. 11. Horakova D, Kalincik T, Dolezal O, Krasensky J, Vaneckova M, Seidl Z, et al. Early predictors of non-response to interferon in multiple sclerosis. Acta Neurol Scand 2012;126(6):390-7. 12. Deen S, Bacchetti P, High A, Waubant E. Predictors of the location of multiple sclerosis relapse. Journal of neurology, neurosurgery and psychiatry 2008;79(10):1190-3. 13. Greer J, Csurhes P, Muller D, Pender M. Correlation of blood T cell and antibody reactivity to myelin proteins with HLA type and lesion localization in multiple sclerosis. The journal of immunology 2008;180(9):6402-10. 14. Gourraud P-A, Sdika M, Khankhanian P, Henry R, Beheshtian A, Matthews P, et al. A genomewide association study of brain lesion distribution in multiple sclerosis. Brain 2013. 15. Mowry EM, Carey RF, Blasco MR, Pelletier J, Duquette P, Villoslada P, et al. Association of Multiple Sclerosis Susceptibility Variants and Early Attack Location in the CNS. PLoS One 2013;8(10):e75565. 16. Bramow S, Frischer JM, Lassmann H, Koch-Henriksen N, Lucchinetti CF, Sorensen PS, et al. Demyelination versus remyelination in progressive multiple sclerosis. Brain 2010;133(10):2983-98. 17. Prineas JW, Barnard RO, Revesz T, Kwon EE, Sharer L, Cho ES. Multiple sclerosis. Pathology of recurrent lesions. Brain 1993;116 ( Pt 3):681-93. 18. Bennetto L, Burrow J, Sakai H, Cobby J, Robertson NP, Scolding N. The relationship between relapse, impairment and disability in multiple sclerosis. Mult Scler J 2011;17(10):1218-24. 19. Cossburn M, Ingram G, Hirst C, Ben-Shlomo Y, Pickersgill TP, Robertson NP. Age at onset as a determinant of presenting phenotype and initial relapse recovery in multiple sclerosis. Mult Scler 2012;18(1):45-54. 20. Fay AJ, Mowry EM, Strober J, Waubant E. Relapse severity and recovery in early pediatric multiple sclerosis. Mult Scler 2012;18(7):1008-12. 21. Kalincik T, Vivek V, Jokubaitis VG, Lechner Scott J, Trojano M, Izquierdo G, et al. Sex as a determinant of relapse incidence and progressive course of multiple sclerosis. Brain 2013; 136:36093617. 22. Tremlett H, Zhao Y, Joseph J, Devonshire V. Relapses in multiple sclerosis are age- and timedependent. J Neurol Neurosurg Psychiatry 2008;79(12):1368-74. 23. Goodin DS, Traboulsee A, Knappertz V, Reder AT, Li D, Langdon D, et al. Relationship between early clinical characteristics and long term disability outcomes: 16 year cohort study (follow-up) of the pivotal interferon beta-1b trial in multiple sclerosis. J Neurol Neurosurg Psychiatry 2011. 24. Tremlett H, Yousefi M, Devonshire V, Rieckmann P, Zhao Y. Impact of multiple sclerosis relapses on progression diminishes with time. Neurology 2009;73(20):1616-23. 25. Confavreux C, Vukusic S, Adeleine P. Early clinical predictors and progression of irreversible disability in multiple sclerosis: an amnesic process. Brain 2003;126(Pt 4):770-82. 26. Leray E, Yaouanq J, Le Page E, Coustans M, Laplaud D, Oger J, et al. Evidence for a two-stage disability progression in multiple sclerosis. Brain 2010;133(Pt 7):1900-13. 27. West T, Wyatt M, High A, Bostrom A, Waubant E. Are initial demyelinating event recovery and time to second event under differential control? Neurology 2006;67(5):809-13. 28. Amato MP, Ponziani G, Bartolozzi ML, Siracusa G. A prospective study on the natural history of multiple sclerosis: clues to the conduct and interpretation of clinical trials. J Neurol Sci 1999;168(2):96-106. 29. Runmarker B, Andersen O. Prognostic factors in a multiple sclerosis incidence cohort with twenty-five years of follow-up. Brain 1993;116 ( Pt 1):117-34. 30. Mowry EM, Pesic M, Grimes B, Deen S, Bacchetti P, Waubant E. Demyelinating events in early multiple sclerosis have inherent severity and recovery. Neurology 2009;72(7):602-8. 31. Cohen JA, Coles AJ, Arnold DL, Confavreux C, Fox EJ, Hartung HP, et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing-remitting multiple sclerosis: a randomised controlled phase 3 trial. Lancet 2012;380(9856):1819-28. 32. Lublin F, Cofield S, Cutter G, Conwit R, Narayana P, Nelson F, et al. Randomized study combining interferon & glatiramer acetate in multiple sclerosis. Annals of neurology 2013. 33. Campbell Z, Sahm D, Donohue K, Jamison J, Davis M, Pellicano C, et al. Characterizing contrast-enhancing and re-enhancing lesions in multiple sclerosis. Neurology 2012;78(19):1493-9. TABLES TABLE 1 Characteristics of the studied population at inclusion patients, number (females, %) 14,969 (71%) age, years‡ 37 ± 11 follow-up duration, years* disease duration, years* 2.8 (0.5, 9.2) disability, EDSS* 2 (1.5, 3.5) EDSS available, number (%) 12,870 (86.0%) EDSS 0-3.5, number (%) 10,110 (78.6%) EDSS 4-5.5, number (%) 1635 (12.7%) EDSS 6-9.5, number (%) 1125 (8.7%) relapses during follow-up, number (%) 1 (initial event only) 2 3-4 5-9 10 or more disease course, number (%) clinically isolated syndrome 5764 (38.5%) relapsing-remitting MS 7902 (52.8%) secondary progressive MS 780 (5.2%) relapsing progressive MS 523 (3.5%) patients treated with disease modifying therapy during follow-up, number (%) ‡, mean standard deviation *, median (quartiles) †, information available in 91% of patients EDSS, Expanded Disability Status Scale at censoring 43 ± 12 4.5 (1.5, 8.9) 10.4 (5.1, 17.1) 2.5 (1.5, 4.5)† 13,556 (90.6%) 8767 (64.7%) 2125 (15.7%) 2664 (19.7%) 3233 (21.4%) 2697 (17.9%) 3458 (22.9%) 2975 (19.7%) 2726 (18.1%) 2021 (13.5%) 10,470 (69.9%) 1955 (13.1%) 523 (3.5%) 10,196 (68.1%) TABLE 2 Characteristics of the recorded relapses all clinical events, number 49,279 by patient age, number (%) 0-10 53 (0.1%) 10-20 2739 (5.6%) 20-30 13,966 (28.3%) 30-40 17,140 (34.8%) 40-50 10,982 (22.3%) 50-60 3705 (7.5%) 60+ 694 (1.4%) by MS course at the time of relapse, number (%) clinically isolated syndrome (initial event) 9723 (19.7%) relapsing-remitting MS 36,627 (74.3%) secondary progressive MS 1861 (3.8%) relapsing progressive MS 1068 (2.2%) by clinical phenotype, number (%) visual 9834 (20.0%) pyramidal 16,932 (34.4%) sensory 23,743 (48.2%) cerebellar 4954 (10.1%) brainstem 8204 (16.6%) bowel / bladder* 2785 (5.7%) cognitive* 735 (1.5%) by severity, number (%) information available 17,117 (34.7%) mild 6799 (39.7%) moderate 9272 (54.2%) severe 1046 (6.1%) by impact on activities of daily living, number (%) information available 10,114 (21.5%) no 2445 (24.2%) yes 7669 (75.8%) by disease modifying therapy (%) on disease modifying agent 13,813 (28.0%) off disease modifying agent 35,466 (72.0%) by steroid treatment (%) no 29,602 (60.1%) yes 19,677 (39.9%) by recovery (%) information available 22,276 (46.2%) complete 11,861 (53.2%) partial 9404 (42.2%) none 1011 (4.5%) *Bowel/bladder and cognitive relapses were usually multi-symptomatic with other associated symptoms/signs (84% and 82%, respectively). TABLE 3 Outcomes of multivariable logistic models in all relapses independent variable visual OR (95% CI) pyramidal OR (95% CI) p relapse phenotype sensory p OR (95% CI) sex [male] 0.88 (0.84-0.93) 10-5 1.11 (1.06-1.16) 10-5 0.89 (0.85-0.92) -14 age 0.98 (0.98-0.99) 10 1.02 (1.01-1.02) 10-14 MS duration 0.94 (0.92-0.96) 10-13 1.01 (1.00-1.03) 0.083 0.99 (0.97-1.00) MS course [RRMS]* N/A N/A N/A [CIS] 2.04 (1.07-3.89) 0.048 0.7 [SPMS] 1 0.2 1.40 (1.02-1.93) [RPMS] 0.39 (0.32-0.48) 10-14 2.82 (2.42-3.28) 10-14 0.57 (0.49-0.65) history of similar relapse 1.81 (1.72-1.91) 10-14 2.97 (2.83-3.12) 10-14 1.98 (1.89-2.08) independent relapse phenotype variable bowel / bladder cognitive OR (95% CI) p OR (95% CI) p sex [male] age MS duration MS course [RRMS]* [CIS] [SPMS] [RPMS] history of similar relapse 1.02 (1.01-1.02) N/A 2.46 (1.63-3.70) 2.48 (1.97-3.12) 0.8 10-8 0.2 0.8 0.9 0.5 N/A 0.1 10-5 10-14 1 0.2 10-4 2.05 (1.42-2.97) p 10-7 0.2 0.023 cerebellar OR (95% CI) 1.09 (1.01-1.16) 1.02 (1-00-1.04) p brainstem OR (95% CI) p 0.03 0.4 0.046 1.10 (1.05-1.17) 0.99 (0.99-1.00) 0.95 (0.93-0.96) 10-4 0.008 10-11 N/A 0.1 0.056 10-14 10-14 N/A 0.28 (0.12-0.65) 1.98 (1.64-2.39) 0.9 0.005 10-11 0.26 (0.14-0.46) 0.63 (0.52-0.76) 0.1 10-5 10-6 3.18 (2.96-3.42) 10-14 2.21 (2.09-2.35) 10-14 2.85 (2.59-3.14) 10-14 5.03 (4.09-6.20) 10-14 All models were adjusted for date, centre and immunomodulatory or immunosuppressive therapy. CI, confidence interval; CIS, clinically isolated syndrome; RPMS, relapsing progressive MS; SE, standard error; SPMS, secondary progressive MS; OR, odds ratio * reference category TABLE 4 Associations between the phenotypes of the initial events and the subsequent relapses initial event phenotype visual pyramidal sensory cerebellar brainstem bowel / bladder cognitive patients (%) 2030 (26.7%) 1700 (22.3%) 3528 (46.3%) 507 (6.7%) 1494 (19.6%) 230 (3%) 108 (1.4%) subsequent relapses, median (quartiles) 3 (1, 5) 3 (1, 5) 3 (2, 5) 3 (1, 5) 3 (1, 5) 3 (2, 5) 3 (2, 5) patients with similar multivariable phenotypes of the initial logistic model and subsequent relapses (%)* OR (95% CI) p 663 (31.2%) 941 (55.4%) 2340 (66.3%) 105 (20.7%) 411 (27.5%) 35 (15.2%) 11 (10.2%) 10-9 10-15 10-15 0.009 10-7 0.5 0.3 1.72 (1.45-2.05) 4.99 (4.23-5.89) 7.71 (6.57-9.05) 1.36 (1.09-1.68) 1.56 (1.32-1.85) Multivariable logistic model with the outcome variable describing phenotypic similarity between the initial relapse and the subsequent relapses, and independent variables comprising relapse phenotype, sex, age, centre and date of relapse onset. The analysed patients were followed in MSBase from clinically isolated syndrome and had at least one documented relapse following the initial event (n=7612). *Defined as patients in whom the initial events and the predominant clinical presentations of the subsequent relapses affected the same functional neurological domains. CI, confidence interval; OR, odds ratio TABLE 5 Relapse severity, impact and recovery relapse phenotype visual pyramidal sensory cerebellar brainstem bowel / bladder cognitive relapse severity1 (n = 17,282) moderate OR (95% CI) 1.65 (1.56-1.75) 1.99 (1.90-2.08) 1.71 (1.61-1.83) 1.42 (1.34-1.50) 1.61 (1.48-1.76) 1.15 (1.02-1.31) p <10-15 <10-15 0.4 <10-15 <10-15 <10-15 0.042 severe OR (95% CI) 2.34 (2.13-2.58) 2.98 (2.74-3.25) 2.03 (1.83-2.26) 1.79 (1.62-1.97) 2.44 (2.16-2.75) 1.40 (1.16-1.70) *The analysis was adjusted for corticosteroid therapy. CI, confidence interval; OR, odds ratio Reference categories: 1mild severity, 2no impact, 3complete recovery. p <10-15 <10-15 0.1 <10-15 <10-15 <10-15 0.001 impact on activities of daily living2 (n = 10,236) incomplete relapse recovery3,* (n = 29,934) OR (95% CI) 1.76 (1.61-1.93) 2.97 (2.75-3.20) 0.91 (0.85-0.98) 2.20 (1.97-2.46) 1.59 (1.46-1.74) 1.87 (1.62-2.17) 1.29 (1.07-1.55) OR (95% CI) p <10-15 <10-15 0.017 <10-15 <10-15 <10-15 0.012 1.40 (1.35-1.44) 1.34 (1.28-1.41) 0.91 (0.87-0.95) 1.37 (1.28-1.41) 1.35 (1.20-1.52) p 0.5 <10-15 0.3 <10-15 10-5 <10-15 10-6 FIGURE LEGENDS Figure 1 CONSORT flowchart of patient disposition. Figure 2 Proportions of relapse phenotypes by sex, age, MS course and MS duration. The graphs show unadjusted incidences. It should be noted that statistical analysis found the association between SPMS (relative to RRMS) and cerebellar relapses negative. Thus, the increasing proportion of cerebellar relapses in SPMS shown here is driven by other confounding predictors (e.g. sex, age and MS duration). CIS, clinically isolated syndrome; RPMS, relapsing progressive MS; RRMS, relapsing-remitting MS; SPMS, secondary progressive MS SUPPLEMENTARY FIGURES - LEGENDS Supplementary Figure 1: Changes in disability during the follow-up period EDSS, Expanded Disability Status Scale Supplementary Figure 2: Principal component analysis: variable importance and loadings