JC article 2-25-13 Problem Based Learning
advertisement
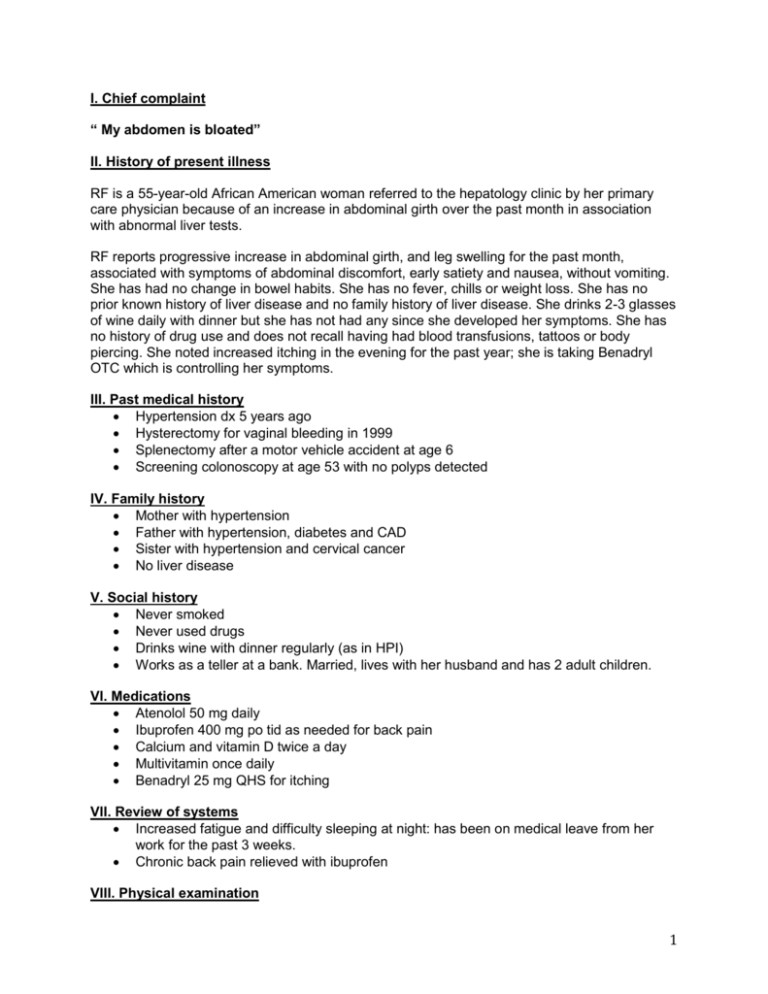
I. Chief complaint “ My abdomen is bloated” II. History of present illness RF is a 55-year-old African American woman referred to the hepatology clinic by her primary care physician because of an increase in abdominal girth over the past month in association with abnormal liver tests. RF reports progressive increase in abdominal girth, and leg swelling for the past month, associated with symptoms of abdominal discomfort, early satiety and nausea, without vomiting. She has had no change in bowel habits. She has no fever, chills or weight loss. She has no prior known history of liver disease and no family history of liver disease. She drinks 2-3 glasses of wine daily with dinner but she has not had any since she developed her symptoms. She has no history of drug use and does not recall having had blood transfusions, tattoos or body piercing. She noted increased itching in the evening for the past year; she is taking Benadryl OTC which is controlling her symptoms. III. Past medical history Hypertension dx 5 years ago Hysterectomy for vaginal bleeding in 1999 Splenectomy after a motor vehicle accident at age 6 Screening colonoscopy at age 53 with no polyps detected IV. Family history Mother with hypertension Father with hypertension, diabetes and CAD Sister with hypertension and cervical cancer No liver disease V. Social history Never smoked Never used drugs Drinks wine with dinner regularly (as in HPI) Works as a teller at a bank. Married, lives with her husband and has 2 adult children. VI. Medications Atenolol 50 mg daily Ibuprofen 400 mg po tid as needed for back pain Calcium and vitamin D twice a day Multivitamin once daily Benadryl 25 mg QHS for itching VII. Review of systems Increased fatigue and difficulty sleeping at night: has been on medical leave from her work for the past 3 weeks. Chronic back pain relieved with ibuprofen VIII. Physical examination 1 Vital signs: P: 68, BP: 122/76, R: 10, T: 98.9, 98% sat on room air Wt 220 lbs, Ht 5’7” General: Evidence of temporal wasting HEENT: Slightly icteric Neck: supple without adenopathy or jugular venous distention Cardiovascular: normal rate, regular rhythm, no murmurs Chest and lungs: symmetrical expansion, clear to auscultation and percussion Abdomen: LUQ scar of prior splenectomy. Distended abdomen, tense, mild diffuse tenderness to palpation. Dull to percussion at the flanks with evidence of shifting dullness. No fluid wave detected. Extremities: without clubbing or cyanosis; 1+ lower extremity edema appreciated bilaterally. Neurologic examination: normal exam. Fully alert and oriented. No asterixis. IX. Laboratory evaluation Component WBC Hgb MCV Platelets INR Na K BUN Creatinine Albumin Total bilirubin Alkaline Phosphatase AST ALT Ferritin HAV serologies HBV serologies HCV antibody AFP ASMA ANA Ig Quant Reference range (4.5-13.5 THO/μL) (13-16 g/dL) (83 – 93) (150-400 THO/μL) (0.9-1.1) (134-142) (3.6 – 5.0) (10-20) (0.6-1.35 mg/dL) (3.6-5.0 g/dL) (0.3-1.2 mg/dL) (38-120 U/L) (10-40 U/L) (9-60 U/L) (0-5 IU/mL) (Less than 1:20) (Less than 1:40) Value 12 THO/μL 10.9 g/dL 96 140 THO/μL 1.7 134 4.0 8 1.0 mg/dL 3.2 g/dL 4.4 mg/dL 187 U/L 128 U/L 78 U/L 12 Negative Negative Positive 8 IU/mL 1:40 1:160 IgG 1.6 g/mL (ULN 1.2) IgA, IgM within normal Table 1 X. Medical imaging: Ultrasound of the abdomen was obtained. The liver had a heterogeneous echotexture, but did not appear nodular. No focal liver lesions. The hepatic and portal veins appeared patent by 2 Doppler. Large amount of ascites noted. Gallbladder is normal. Spleen is absent. Kidneys are of normal size and echogenicity, no hydronephrosis. XI. Follow up Visit A- Initial intervention The patient underwent an 8.1 L paracentesis with albumin replacement. Ascitic fluid analysis revealed an ascitic fluid protein of 1.0, albumin < 1.0, WBC 35. Ibuprofen was stopped, she received diet counseling for a 2 gram Na restricted diet. Spironolactone 100 mg daily and furosemide 40 mg daily were started. Visit B- Two months follow up She presents for follow up 2 months later. She has been abstinent of alcohol. Ascites is controlled on diuretics. The following laboratory tests are obtained on follow up. Component WBC Hgb Platelets INR Na K BUN Creatinine Albumin Total bilirubin Alkaline Phosphatase AST ALT HCV RNA HCV genotype Reference range (4.5-13.5 THO/μL) (13-16 g/dL) (150-400 THO/μL) (0.9-1.1) (0.6-1.35 mg/dL) (3.6-5.0 g/dL) (0.3-1.2 mg/dL) (38-120 U/L) (10-40 U/L) (9-60 U/L) Value 4.3 THO/μL 12.0 g/dL 182 THO/μL 1.2 132 4.3 23 1.2 mg/dL 3.5 g/dL 2.9 mg/dL 198 U/L 58 U/L 38 U/L 1,200,000 units 1b Table 2 Visit C- One month later RF continued to be well until about 1 month after her follow up visit when she started developing leg swelling, followed by increased abdominal distention and confusion progressing over 5 days prior to presentation. She is brought to the ED by her husband who reported that she has not been drinking alcohol and has been taking all of her medication as instructed. She has not had fever or chills. No cough or shortness of breath or headache. No urinary symptoms. She has been complaining of a mild abdominal discomfort and nausea and has a reduced oral intake over the past 48 hours. Vitals BP110/65, Pulse 88, RR 14, Temp 99.2 She is icteric, has a distended abdomen with flank dullness, +2 LE edema, she opens her eyes when her name is called. She responds to questions with an incomprehensible mumbling. Milk maid sign is positive. Component Reference range Value 3 WBC Hgb Platelets INR Na K Creatinine Albumin Total bilirubin Alkaline Phosphatase AST ALT (4.5-13.5 THO/μL) (13-16 g/dL) (150-400 THO/μL) (0.9-1.1) (0.6-1.35 mg/dL) (3.6-5.0 g/dL) (0.3-1.2 mg/dL) (38-120 U/L) (10-40 U/L) (9-60 U/L) 8.8 THO/μL 10.3 g/dL 96 THO/μL 2.1 130 5.1 2.72 mg/dL 2.9 g/dL 7.0 mg/dL 113 U/L 48 U/L 44 U/L Table 3 Issues for contemplation A. Initial Presentation Discuss the finding of a distended abdomen on exam in our patient and the diagnostic accuracy of physical exam maneuvers in identifying ascites as a cause of abdominal distention. What other physical exam findings would you look for that would help you with the differential diagnosis? What is your assessment of the patient’s alcohol intake? What other elements of history would you like to obtain to ascertain whether the patient has signs of alcohol dependence? Discuss the abnormalities in liver associated enzymes, markers of liver synthetic function, and CBC on presentation in our patient and how this helps you in formulating a differential diagnosis for the cause of her symptoms. Discuss the finding of a low Ferritin level on initial evaluation. What was the significance of a positive hepatitis C antibody? What are the sensitivity and specificity of this finding in detecting a chronic hepatitis C infection? What are the risk factors for chronic hepatitis C? Who should be screened for this infection in the general population? What is the likely mode of transmission of HCV to our patient? What are the factors associated with a severe liver injury due to hepatitis C? Discuss the clinical significance of a positive ANA and elevated IgG fraction in our patient. Are there additional tests that you like to obtain at the time of the initial evaluation of our patient? Are there additional management interventions that you would recommend after initial evaluation? B. Hepatitis C management What is the current standard of care in treatment of hepatitis C infection and the expected outcome of treatment in the general population of infected patients? What are the potential adverse effects of the standard of care treatment? 4 What are the risks and benefits of HCV treatment in the case of our patient at initial presentation and at the time of the first follow up visit. C. Presentation to the ED What is your interpretation of the patient’s history and physical exam findings at presentation to the ED? What is your interpretation of her laboratory tests on presentation? What is your differential diagnosis for this acute illness? Are there findings on her initial evaluation and testing that suggest that she is a risk for a specific complication? What would you initial steps in management be? Assuming that, after an initial diagnostic evaluation and treatment, three days after the initial presentation, her mental status is improved, bilirubin is reduced to 4.0 and INR to 1.7, but Creatinine continues to rise and is now 3.6. She is making about 80 cc of urine per day. How would you evaluate the renal further? What are the next steps in management? What is her long term prognosis, and how does this affect your management decisions? 5