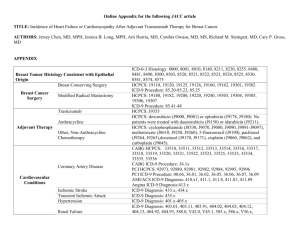
Supplementary material Table A1. Codes used in defining the
advertisement

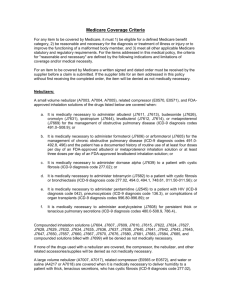
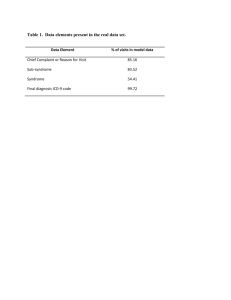
Supplementary material Table A1. Codes used in defining the outcome and the covariates. Description Endocarditis Code source ICD-9 Codes 421.0, 421.9, 424.9 Valve-related risk factors for endocarditis, including congenital disorders Valvuloplasty HCPCS ICD-9 Replacement Valvotomy Conduits 35.96, 35.1, 35.10 – 35.14 HCPCS 33405, 33406, 33410 - 33413, 33430, 33465, 33475 ICD-9 35.06, 35.07, 35.08, 35.09, 35.2, 35.20, 35.21-35.28 HCPCS 33420, 33422, 33460, 33470, 33471, 33472, 33474 ICD-9 Resection, repair 33400, 33401, 33403,33425, 33426, 33427, 33463, 33464 HCPCS 35.0, 35.00 - 35.05 33414-33417, 33468, 33476, 33478, 33496 ICD-9 35.97 HCPCS 33404 ICD-9 35.92-35.95 Diseases of mitral valve ICD-9 394, 394.0, 394.1, 394.2, 394.9, 396.0-396.3, 396.8, 396.9, 424.0, 746.5, 746.6, Diseases of aortic valve ICD-9 395, 395.0, 395.1, 395.2, 395.9, 424.1, 746.3, 746.4 Diseases of tricuspid valve 397, 397.0, 397.9, 424.2, 746.1, 746.2 Diseases of pulmonary valve 397.1, 424.3, 746.0, 746.00, 746.01, 746.02, 746.09 Rheumatic fever with heart involvement ICD-9 391, 391.1, Structural heart risk factors for endocarditis other than valve-related Septum-related HCPCS 33641, 33645, 33647, 33660, 33665, 33670, 33681, 33684, 33688, 1 ICD-9 35.4, 35.41, 35.42, 35.5, 35.50-35.55, 35.6, 35.60 – 35.63, 35.7, 35.70 – 35.73, 35.98 745.5, 745.6, 745.60, 745.61, 745.69, 745.7, 745.9 Sinus of Valsalvarelated Non-valvular congenital disorders HCPCS 33702, 33710, 33720, 33722 ICD-9 35.39 ICD-9 745.0, 745.1, 745.10-745.12, 745.19, 745.2, 745.3, 745.4, 745.8, 746.7, 746.81-746.84, 746.9 Intravascular devices Pacemakers HCPCS ICD-9 33206 - 33208, 33210, 33214 – 33218, 33220, 33222 – 33226, 33233 - 33235, 33238, 33240, 33241, 33243, 33244, 33249. 00.50, 00.51, 00.52, 00.54, 37.7, 37.70, 37.71, 37.72, 37.73, 37.75, 37.78, 37.8, 37.80 – 37.83, 37.85 – 37.87, 37.89 Peritoneal-venous shunt HCPCS 49425-49429 Ventriculo-atrial shunt HCPCS 62220 ICD-9 02.32 ICD-9 585.6 End stage renal disease Dialysis-related procedures HCPCS 90921, 90925, 90935, 90937, 90940, 90945, 90947, 90989, 90993, 90997, 90999, 36800, 36810, 36815, 36818, 36819, 36820, 36821. Venous catheterization for renal dialysis ICD-9 38.95 Arteriovenostomy for renal dialysis ICD-9 38.95, 39.42, 39.43 Hemodialysis ICD-9 39.95 Peritoneal dialysis ICD-9 54.98 Anemia ICD-9 280.0, 280.1, 280.8, 280.9, 281.0, 281.8, 281.9, 285.1, 285.2, 285.9 Gastrointestinal bleeding ICD-9 286.5, 459.0, 562.02, 562.03, 562.12, 562.13, 569.3, 569.84, 569.85, 569.86, 578.1, 578.9, 792.1, 998.11' Gastrointestinal symptoms ICD-9 Constipation 564.0, 564.00, 564.09, 564.01, 564.02 Diarrhea 008.42, 008.43, 008.45, 008.5, 008.8, 009.0, 009.1, 009.2, 009.3, 558.2, 558.3, 558.9, 564.4, 564.5, 564.8, 2 564.9, 787.91 Change in bowel habit 787.99 Abdominal pain 789.0, 787.3, 789.4, 789.6 Irritable bowel syndrome 564.1 Large bowel obstruction 560, 560.8, 560.9, 560.89 Treatments Colon surgery Chemotherapy1 HCPCS 44140, 44141, 44143, 44144, 44145, 44146, 44147, 44150, 44151, 44152, 44153, 44155, 44156, 44157, 44158, 44160, 44204, 44205, 44206, 44207, 44208, 44210, 44211, 44212 ICD-9 45.72, 45.73, 45.74, 45.75, 45.76, 45.8, 17.3, 17.31, 17.32, 17.33, 17.34, 17.35, 17.36, 17.37, 17.38, 17.39 Betos P1B HCPCS ICD-9 J9000-J99992, Q0083-Q0085, J8520, J8521, J8530, J8540, J8560, J8597, J8610, J8999 9925, V581, V662, V672 Revenue center 0331, 0332, 0335 Visits to the emergency department HCPCS 99281, 99282, 99283, 99284, 99285, 99291, 99292 Clinical evaluation3 HCPCS 99201, 99202, 99203, 99204, 99205, 99211, 99212, 99213, 99214, 99215, 99217, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99241, 99242, 99243, 99244, 99245, 99251, 99252, 99253, 99254, 99255, 99261, 99262, 99263, 99271, 99272, 99273, 99274, 99275, 99301, 99302, 99303, 99311, 99312, 99313, 99361, 99362 1 To identify oral capecitabine in the DME file we used the following National Drug Codes: 00004110020, 00004110150, 00004110116, 00004110051, 00004110013, 00004110022, 00004110113, 00004110151. 2 Excluding the following codes from this sequence: J9003, J9165, J9175, J9202, J9209, J9212- J9226, J9240, J9295, J9381, J9395. 3 3 Clinical evaluation consists on any of the following: new outpatient, established outpatient, hospital observation services, new inpatient, established inpatient, observation/inpatient care services, outpatient consultation, inpatient consultation, follow-up inpatient consultation, confirmatory consultation, nursing facility services and team conference. 4 Table A2. Incidence rate of pyelonephritis and meningitis in between 90 days before and 90 days after the diagnosis of colorectal, lung, breast, and prostate cancer Cases per 100,000 person-months (95% CI) Persons Personmonths Cases Crude rate Standardized rate1 Colorectal Pyelonephritis 167,390 963,521 137 14.2 (11.8-16.6) 14.2 (11.8-16.6) Meningitis 966,382 * 1.1 (0.5-1.8) 1.1 (0.5-1.8) Pyelonephritis 208,702 1,159,817 158 13.6 (11.5-15.7) 14.8 (12.1-17.5) Meningitis 1,162,863 24 2.1 (0.4-1.2) 1.6 (0.9-2.3) 996,830 102 10.2 (8.2-12.2) 10.2 (8.2-12.3) 169,991 1,000,374 * 0.4 (0.0-0.8) 0.4 (0.0-0.8) Pyelonephritis 202,583 1,193,481 149 12.5 (10.5-14.4) 15.7 (12.7-18.7) Meningitis 202,794 1,195,078 * 0.4 (0.1-0.8) 0.4 (0.0-0.7) Pyelonephritis 276,182 1,624,815 124 7.6 (6.3-9.0) 7.6 (6.1-9.1) Meningitis 1,630,588 16 1.0 (0.5-1.5) 0.9 (0.4-1.4) 167,839 Lung 209,207 Breast Pyelonephritis 169,434 Meningitis Prostate Non-cancer 277,120 1 Incidence rate is directly standardized to the age and sex (except for breast and prostate cancer) distribution of colorectal cancer cases. * Cells with counts of 11 or lower are blinded following SEER-Medicare privacy policy 5 Table A3. Survival analysis using different time frames to define concomitant diagnosis of infective endocarditis and stage I-III colorectal cancer* No endocarditis Endocarditis 139,631 142 2-year overall survival, % 73.1 (72.8-73.3) 49.5 (41.0-57.5) 2-year CRC-specific survival, % 85.7 (85.5-85.9) 85.5 (77.5-90.8) HR overall survival Reference 1.60 (1.33-1.93) HR CRC-specific survival Reference 1.30 (0.89-1.89) 139,583 190 2-year overall survival, % 73.1 (72.8-73.3) 48.1 (40.8-55.0) 2-year CRC-specific survival, % 85.7 (85.5-85.9) 85.0 (78.2-89.9) HR overall survival Reference 1.62 (1.39-1.90) HR CRC-specific survival Reference 1.28 (0.92-1.77) Endocarditis between 60 days before and 60 days after cancer diagnosis N Endocarditis between 120 days before and 120 days after cancer diagnosis N *HR: hazard ratio, CRC: colorectal cancer 6 Figure A1. Relationship between diagnostic colonoscopy and admission due to infective endocarditis. 7