Plunket Severity Assessment Code Framework
advertisement
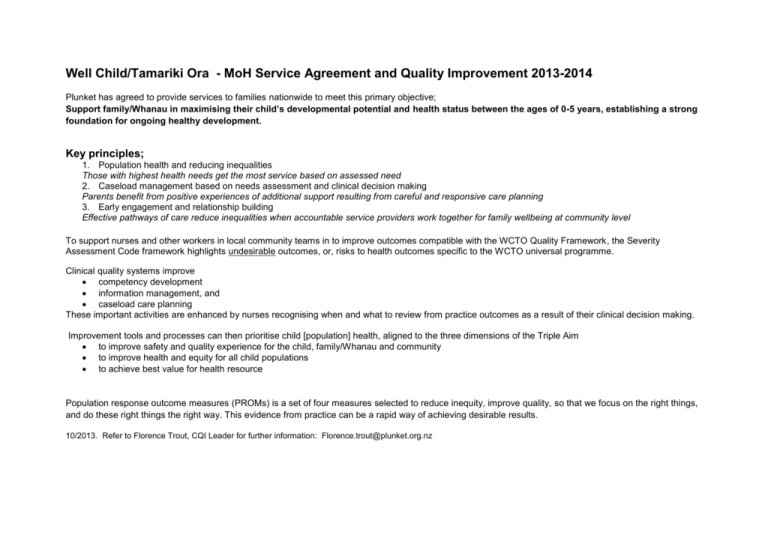
Well Child/Tamariki Ora - MoH Service Agreement and Quality Improvement 2013-2014 Plunket has agreed to provide services to families nationwide to meet this primary objective; Support family/Whanau in maximising their child’s developmental potential and health status between the ages of 0-5 years, establishing a strong foundation for ongoing healthy development. Key principles; 1. Population health and reducing inequalities Those with highest health needs get the most service based on assessed need 2. Caseload management based on needs assessment and clinical decision making Parents benefit from positive experiences of additional support resulting from careful and responsive care planning 3. Early engagement and relationship building Effective pathways of care reduce inequalities when accountable service providers work together for family wellbeing at community level To support nurses and other workers in local community teams in to improve outcomes compatible with the WCTO Quality Framework, the Severity Assessment Code framework highlights undesirable outcomes, or, risks to health outcomes specific to the WCTO universal programme. Clinical quality systems improve competency development information management, and caseload care planning These important activities are enhanced by nurses recognising when and what to review from practice outcomes as a result of their clinical decision making. Improvement tools and processes can then prioritise child [population] health, aligned to the three dimensions of the Triple Aim to improve safety and quality experience for the child, family/Whanau and community to improve health and equity for all child populations to achieve best value for health resource Population response outcome measures (PROMs) is a set of four measures selected to reduce inequity, improve quality, so that we focus on the right things, and do these right things the right way. This evidence from practice can be a rapid way of achieving desirable results. 10/2013. Refer to Florence Trout, CQI Leader for further information: Florence.trout@plunket.org.nz WELL CHILD/TAMARIKI ORA SEVERITY ASSESSMENT CODE (SAC) Consequence Table For Actual And Potential Adverse Events Linked To The Triple Aim Adverse Events Are Rated On Actual Outcome And Near Misses On Quality Outcomes severe Child or other potential or actual death directly related to the service delivery episode Failure to recognise severe and acute health risk with high risk of harm to caregiver and/or child/tamariki Includes child/tamariki abduction from any parenting group/volunteer/clinical activity Example: Unanticipated severe reaction to immunisation process requiring resuscitation SAC 1 QAims1,2,3 major moderate Major permanent loss of function or temporary severe disability related to service delivery episode Failure to recognise need for potential urgent intervention that may result in unanticipated harm to the child/tamariki and/or caregiver Moderate permanent or temporary major loss of function related to service delivery episode Example: Failure to act when immediate care is indicated; acute febrile illness, family violence, or early intervention for physiology / development outside normal range and requiring prompt diagnosis Failure to identify vulnerable children/tamariki in a caseload in the progressive universal surveillance program, resulting in families/whanau missing out on engaging in timely, planned care pathway(s) in early interventions Example: Ineffective prioritisation of child safety interventions from analysis of need minor Temporary moderate impairment or an increased level of care resulting from service delivery Failure to recognise results from child screening that require referral for diagnosis minimal/near miss No harm or increased need for health care from adverse event Child injury requiring only first aid during any planned Plunket activity (no GP visit, A&E nor hospitalisation) Failure to recognise results from adult screening that requires referral for diagnosis Involvement in but not entire responsibility for illness or injury caused through inaction from, or omission of, service Example: Infant hits head on measuring board during length assessment procedure Example: No plan for screen result with potential for delay/harm SAC 2 QAim 1 SAC 3 QAim 2 SAC 4 QAim 3 SAC 4 QAim 1 Improved safety and quality experience Improved health and equity Best value for health system resources Improved safety and quality experience