VIC FACEM Study Group 18th April 2015 Trauma SAQ`s Question 1
advertisement

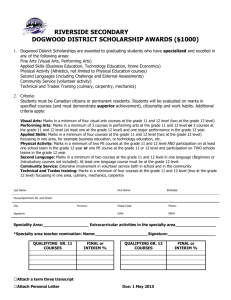
VIC FACEM Study Group 18th April 2015 Trauma SAQ’s Question 1 A 37 year old male presents to your tertiary ED by ambulance after being involved in a high speed motorbike accident. He was the rider and was found on the road 20 metres from his bike. On arrival he is complaining of lower abdominal pain. He was given 2 litres of Normal Saline pre-hospital as well as 10mg IV morphine. He looks pale and his vitals are: SaO2 96% on 8l/ min via Hudson mask HR 110 sinus tachycardia BP 80/60 Temp 34.6ºC FAST scan - negative A pelvic x-ray is performed as part of his primary survey 1. Give an interpretation of the x-ray, providing positive findings (2 marks) ________________________________________________________________________ ________________________________________________________________________ 2. List potential other injuries in this patient (4 marks) ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 3. List the management priorities for his haemodynamic instability (4 marks) ________________________________________________________________________ ________________________________________________________________________ Question 2 A 42 year old male presents to your tertiary ED by ambulance after being involved in a high speed MVA. He was the driver, restrained, and airbags were deployed. On arrival he is awake and alert, complaining of lower abdominal pain and appears to have isolated abdominal injuries. On initial assessment: His vitals are: SaO2 98% on 2L O2 HR 105 BP 90/60 GCS15/15 FAST scan - positive for free fluid in Morrison’s pouch This is a picture of his abdomen: 1. Question List the potential injuries based on the appearance of the image provided and the information above (4 marks) ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 2. You have given him a 500ml crystalloid fluid bolus and his blood pressure is now 105/65. List your management priorities (3 marks) ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 3. List the disposition options for this patient along with the factors that will influence your decision (3 marks) ________________________________________________________________________ ________________________________________________________________________ Question 3: A 29 year old woman is brought to the Emergency Department after an alleged assault by her husband, claiming to have been punched and kicked repeatedly in the abdomen. She is 32 weeks pregnant and has multiple bruises across the anterior abdominal wall. She is alert, with a GCS of 15 and the following vital signs. PR 110 RR 24 BP 90/50 Sats 97% on room air She is complaining of severe abdominal pain. 1: List five (5) complications of blunt abdominal injury in this patient (5 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 2: What are the possible causes for her tachycardia? (5 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 3: List two (2) investigations to assess fetal wellbeing and your rationale for their use (4 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 4: Which clinical features would prompt an immediate obstetric consultation (5 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ Question 4 A 48yo man is brought to the ED after sustaining a single stab wound to the left side of his chest. He is alert, GCS 15, vocalising normally but is pale, diaphoretic, and acutely short of breath. His vital signs are: PR RR BP Sat T 123 24 94/52 88% on 8L via Hudson mask 36 A chest x-ray is taken soon after his arrival: 1. List your immediate management priorities (6 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 2. List 2 benefits and 2 limitations of bedside ultrasound in the assessment of this condition (4 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ 3. What are the indications for urgent transfer to the operating theatre for surgical management of this condition? (3 marks) ______________________________________________________________ ______________________________________________________________ ______________________________________________________________ ANSWERS: QUESTION 1 1.1: Give an interpretation of the image, providing positive findings (2 marks) - Open book pelvis with diastasis of the pubic symphysis - Widening of the right sacroiliac joint 1.2: List potential associated injuries (4 marks) Any 4 of the following: - Closed head injury - Femoral fractures - Thoracic injury - Bladder / GU injury - Abdominal solid organ - Hollow viscus injury - Diaphragmatic injury 1.3: Outline the management priorities for his haemodynamic instability (4 marks) - Apply pelvic binder / external compression using binder / sheets etc to reduce pelvic volume - Haemostatic resuscitation / damage control resuscitation, massive transfusion, with early PRBC, FFP, Platelets targeting coagulopathy of trauma - Correct hypothermia - Tranexamic acid 1g loading followed by 1g over following 8 hours - Seek and treat other causes of blood loss - external compression, splinting of long bone fractures - Early involvement of interventional radiologist / trauma surgeon / orthopaedic surgeon to plan for - Interventional angiographic embolisation - Pre-peritoneal packing - Pelvic stabilisation by external fixation - Remember FAST negative so laparotomy other interventions prioritised above laparotomy - REBOA not yet standard care / evidence based so don’t mention it QUESTION 2 2.1: List the potential injuries based on the appearance of the image provided and the information above (4 marks) - Intra-abdominal solid organ injury - liver / spleen / pancreas - Intra-abdominal hollow viscus injury - small bowel perforation, mesenteric tear - Ruptured diaphragm - Intra-peritoneal rupture of distended urinary bladder - Spinal injury - e.g Chance fracture - Burst fracture lower T spine, L spine - Blunt aortic injury / sternal fractures / clavicle fractures - you may not get marks for this as the questions state - isolated injury 2.2: You have given him a 500ml crystalloid fluid bolus and his blood pressure is now 105/65. List your management priorities (3 marks) - Restrictive approach - permissive hypotension - aim for systolic BP around 90mmHg in order to enhance vasoconstriction and clot stabilisation, whilst maintaining vital end organ perfusion - Analgesia - small aliquots of IV opiate analgesia - e.g 50mcg Fentanyl - Antibiotic prophylaxis if mesenteric injury suspected - Maintain normothermia, correct acidosis, - Prepare patient for CT - NGT - IDC 2.3 List the disposition options for this patient along with the factors that will influence your decision (3 marks) - Unstable haemodynamics plus positive FAST - theatre for laparotomy - If stable, and fluid responsive - CT scan to evaluate intra-abdominal further and to identify other injuries e.g - brain / spine / thoracic / pelvic - Interventional radiology after CT in conjunction with radiologist if contrast blush or extravasation identified on CT. - HDU / ICU post theatre / IR for ongoing supportive management QUESTION 3 3.1 Non pregnancy related 1) Solid organ injury: liver spleen kidney laceration 2) Retroperitoneal haemorrhage (more common in pregnancy) 3) Hollow viscus injury - rare Pregnancy related 1) Placental abruption 2) Uterine rupture 3) Preterm labour 4) Feto-maternal haemorrhage “Fetal death” – not really an answer – need to state from what 3.2 1) 2) 3) 4) 5) May be normal for pregnancy Pain Supine hypotension/IVC compression Hypovolaemia/haemorrhage Other non-abdominal injury eg: tension pneumothorax 3.3 1) Bedside ultrasound: for cardiac activity, movement, presence does not exclude serious injury 2) CTG (minimum 4-6 hours) 3.4 1) 2) 3) 4) 5) 6) 7) 8) uterine contractions/tetany significant uterine tenderness or irritability vaginal bleeding rupture of the amniotic membranes presenting part visible non-reassuring fetal heart rate pattern on CTG no fetal heartbeat seen on bedsideultrasound other serious maternal injury Other potential obstetric trauma questions: Peri-mortem c-section - Everyone’s afraid of it, very hard to write a question on this topic for this type of exam (Remember Don – complex procedures unlikely in OSCE…) - Need to know: - Indication: maternal arrest unresponsive to standard resuscitative treatment and correction of supine hypotension - Ideally decision to act within 4 minutes of arrest, baby out by 10 mins max (EAST guidelines state may go out to 20 mins…) - How you plan to do it: vertical-vertical, or vertical/horizontal incisions. - Post procedure care Indications for anti-D: - See: http://www.transfusion.com.au/disease_therapeutics/fetomaternal/HDN Who should attend a pregnant trauma resuscitation?: - Usual trauma team including anaesthetist - Obstetrician/O&G Reg (if in doubt in exam – get the Consultant) - Midwife - essential - Paediatrician/Paeds Reg (again, if in doubt in exam – get the Consultant) Equipment to prepare prior to an obstetric trauma patient arriving: Mother - Usual resus equipment - US for FAST but also for potential difficult IV access - Airway: Ramp (if spinal precautions not required), short handled laryngoscope - Breathing – no special equipment required, but ICC’s must go in higher (aim 3 rd-4th IC space) - Circulation – nothing special required, be aware of issues related to circulating volume, can give O-negative to pregnant mothers, ideally only 2 units before switching to type-specific or cross matched Baby - Rususcitaire/neonatal resus trolley with warmer - Airway/breathing: Size 3-3.5 ETT, infant BVM or Neo-Puff on Resuscitatire, 5cm H2O PEEP, start 100% O2 - Circulation – 24G IV, potential need for umbilical vein cannulation – best to get paeds to do it, or intra-osseous – very hard in fresh baby, cord clamps x 2 - Equipment for cord blood gas sampling - Disability – warming essential, towels to dry - Drugs: Adrenaline: 10mcg/kg – usually 3kg so 30mcg IV as bolus - Volume: N.Saline or O-Neg blood (if blood loss considered likely), 10-20ml/kg, can repeat Reference: http://www.neoresus.org.au/pages/LM1-8-3.php http://resus.org.au/guidelines/ Scroll down to neonatal resus section – you must download and read these guidelines! 4.1 High flow O2 Large bore IV access x 2 &Fluid bolus. 1-2 L crystalloid whilst arranging urgent O-negative blood Decompression left chest – 28-32Fr ICC underwater seal drain Urgent Thoracic surgical consultation Bedside US for possible tamponade Fully expose for other stab wounds/injuries 4.2 Benefits Sensitivity as good or better than CxR Can diagnose tamponade Limitations View may be obscured by subcut emphysema, swelling/bruising, obesity Operator dependent 4.3 > 1500ml blood in chest drain at insertion > 200ml/h for 3 consecutive hours, or > 100 ml/h for > 6 hours Tamponade