Psychopathology of Child Soldiers
advertisement

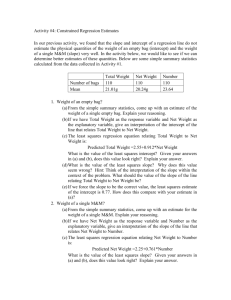
1 Supplementary Material Title: Risk and protective factors for the development of depressive symptoms in children and adolescents: results of the BELLA longitudinal study Journal: Journal of European Child and Adolescent Psychiatry Authors: Fionna Klasen, Christiane Otto, Levente Kriston, Praveetha Patalay, Robert Schlack, Ulrike Ravens-Sieberer & the BELLA study group Corresponding author: Fionna Klasen, University Medical Center Hamburg-Eppendorf, Department of Child and Adolescent Psychiatry, Psychotherapy, and Psychosomatics, Martinistrasse 52, D - 20246 Hamburg, Germany, email: f.klasen@uke.de 2 Calculation and evaluation of latent growth models For calculating LGMs, robust maximum-likelihood (MLR) estimation method was used, which is a full-information maximum-likelihood technique. Since intervals between points of data assessment were one year each, equidistant time scores were set in LGMs (the slope quantifies the amount of change in the corresponding variable over one year). Further, we assumed linear growth in each model, but we additionally tested for potential improvement including a quadratic term. To compare models with and without additional shape factor, model fit according to the Akaike information criterion (AIC) [1], the correlation between intercept and slope, as well as residual variances were used. For final LGMs means and variances of intercepts and slopes were calculated and the fit was evaluated according to the Root Mean Square Error of Approximation (RMSEA) [2] and the Comparative Fit Index (CFI) [3]. Analyses revealed that the inclusion of an additional shape factor lead to no substantial improvement in model fit (please see Supplementary Table 2; e.g. for the SCL-S-9 the linear growth model had an AIC of 4,987.63 and the model with additional shape factor had an AIC of 4,980.59). Correlations between intercepts and slopes as well as residual variances also differed only marginally, if at all, comparing models with linear growth to models with additional shape factor (e.g. for SCL-S-9 models correlations between intercept and slope were -0.014 versus -0.015, residual variances hardly differed). For final LGMs, intercepts for all variables had significant means and variances (see Supplementary Table 3). For the slopes average change was significant for all variables, but the variance in depressive symptoms (p=.095) or parental mental health problems (p=.283) was not significant. The fit of the model for depressive symptoms was good considering both indices (Chi²<0.001; p=0.9916; Degrees of Freedom (df)=1; RMSEA<0.001; 90%-Confidence interval (90%-CI) for RMSEA=0.000-0.000; CFI~1.000). For parental mental health problems, model fit was nearly acceptable considering the Confidence interval for the RMSEA, but clearly acceptable according to the CFI (Chi²=10.172; p=0.0014; df=1; RMSEA=0.075; 90%-CI for RMSEA=0.038-0.119; CFI=0.984). For self-efficacy model fit was good due to both indices (Chi²=0.096; p=0.7564; df=1; RMSEA<0.001; 90%-CI for RMSEA=0.000-0.000; CFI~1.000), but for family climate an acceptable fit due to the RMSEA and a good fit based on the CFI were found (Chi²=1.519; p=0.2178; df=1; RMSEA=0.018; 90%-CI for RMSEA=0.000-0.071; CFI=0.999). For social support, model fit was close to acceptable, slightly beyond the limits reported for the estimate of the RMSEA and the CFI (Chi²=12.023; p=0.0005; df=1; RMSEA=0.082; 90%-CI for RMSEA=0.045-0.126; CFI=0.973). Overall, the fit of the LGMs used in the present study ranged from nearly acceptable to good. 3 Supplementary Table 1. Descriptive data of used measures in the analysed sample Baseline n Socio-economic data Gender 1-year follow-up n % (n) [mean (SD)] 2-year follow-up n % (n) [mean (SD)] 1,643 Female 50.6 (832) Age (in years) 1,643 Socio-economic status2 1,643 [13.92 (2.003)] Low 24.1 (396) Middle 49.8 (819) High 26.0 (428) Depressive symptoms Participants with depressive symptoms3 Depressive symptoms Risk factor Parents with mental health problems4 % (n) [Mean (SD1)] 1,617 16.9 (273) [9.85 (6.913)] 1,220 15.2 (185) [9.39 (6.908)] 1,188 13.7 (163) [9.13 (7.42)] 1,625 8.2 (133) 1,257 8.4 (106) 1,220 6.1 (75) Parental mental health problems [0.61 (0.531)] [0.59 (0.532)] [0.51 (0.511)] Protective factors Self-efficacy 1,616 [2.13 (0.382)] 1,217 [2.15 (0.436)] 1,188 [2.17 (0.406)] Family climate 1,627 [1.83 (0.530)] 1,181 [1.84 (0.522)] 992 [1.80 (0.528)] Social support 1,625 [3.12 (0.742)] 1,185 [3.30 (0.669)] 997 [3.32 (0.647)] 1 SD=standard deviation; 2 The Winkler-index was used to categorise participants into groups with low (scores from 3 to 8), middle (9 to 14) or high (15 to 21) socio-economic status (Winkler et al.[4], Lange et al. [5]); 3 The sum-score of the CES-DC ranging from 0-60 was used to differentiate between participants with and without depressive symptoms using the published cutoff of 16 and above suitable to screen for major depressive disorder (Fendrich et al. [6]); 4 The mean of the SCL-S-9 ranging from 0 to 4 was used to differentiate between participants with or without parental mental health problems according to published reference data using the cutoff of the mean of the reference sample plus two standard deviations or a higher score as indicator for given mental health problems (Klaghofer et al. [7]). 4 Supplementary Table 2. Comparison of models with linear growth to models with additional shapefactor Models with linear growth AIC2 Construct Depressive symptoms Risk factor Parental mental health problems Protective factors Self-efficacy Family climate Social support 1 correlation residual variances models with additional shape factor1 AIC correlation of intercept of intercept and slope and slope residual variances 2,6373.57 -1.978 19.530/22.183/24.092 2,6375.57 -1.981 19.526/22.188/24.077 4,987.63 -0.014 0.084/0.107/0.090 4,980.59 -0.015 0.084/0.107/0.089 3,301.77 4,828.26 7,269.57 -0.014 -0.026 -0.045 0.048/0.097/0.029 0.089/0.098/0.042 0.243/0.207/0.125 3,303.67 4,828.75 7,256.50 -0.014 -0.026 -0.045 0.048/0.097/0.029 0.090/0.098/0.042 0.243/0.204/0.126 Including a quadratic term with a variance of 0; 2 Akaike information criterion [1]. 5 Supplementary Table 3. Intercepts and slopes of latent growth models Intercept slope Construct Measure [range of raw scores] mean variance mean variance Depressive symptoms CES-DC1 [0–60] 9.845*** 28.214*** -0.313** 3.014 SCL-S-92 [0-4] 0.615*** 0.198*** -0.048*** 0.009 Self-efficacy GSE3 [0-3] 2.135*** 0.098*** 0.019*** 0.024*** Family climate FCS4 [0-3] 1.836*** 0.192*** -0.020** 0.038*** Social support SSS-short5 [0-4] 3.139*** 0.296*** 0.099** 0.046*** Risk factor Parental mental health problems Protective factors Latent growth models were calculated assuming linear growth; ** p≤.01; *** p≤.001; 1 CES-DC=Center for Epidemiologic Studies Depression Scale (Radloff et al. [8], Barkmann et al. [9]); 2 SCL-S-9=Symptom-Check List Shortversion-9 (Klaghofer et al. [7]); 3 GSE=General Self-Efficacy Scale (Schwarzer et al. [10,11]); 4 FCS=Family Climate Scale (Schneewind et al. [12]); 5 SSS-short=Eight items of the Social Support Survey (Donald et al. [13]). 6 Supplementary Table 4. Self-efficacy moderating the association between parental mental health problems and depressive symptoms of children and adolescents Regression Model A11 regression Model B12 predicting initial depressive predicting change in depres- symptoms sive symptoms b β p b <.001 -0.330 β p Constant 9.191 <.001 Female 1.300 .146 <.001 0.030 .021 .385 Age (in years at baseline) 0.309 .139 <.001 -0.007 -.021 .393 Socio-economic status (at baseline) -0.058 -.055 .013 0.008 .046 .059 2.107 .189 <.001 0.127 .070 .012 0.999 .053 .055 0.002 .001 .979 -1.467 -.210 <.001 0.018 .003 .922 Change in parental mental health problems (slope) by change in self-efficacy (slope) 3.018 .018 .494 Initial parental mental health problems (intercept) by change in self-efficacy (slope) -0.127 -.008 .773 Change in parental mental health problems (slope) by initial self-efficacy (intercept) 2.363 .033 .241 Risk factor Initial parental mental health problems (intercept) Change in parental mental health problems (slope) Protective factors Initial self-efficacy (intercept) -5.950 -.356 <.001 Change in self-efficacy (slope) Interactions between risk and protective factors Initial parental mental health problems (intercept) by initial self-efficacy (intercept) 1 0.514 Linear regression Model A1 (n=1,643); model fit: R²=.230; F=81.270; 2 linear regression Model B1 (n=1,643); model fit: R²=.053; F=8.233; b=unstandardized regression coefficient; β=standardized regression coefficient .012 .568 7 Supplementary Table 5. Family climate moderating the association between parental mental health problems and depressive symptoms of children and adolescents Regression Model A21 regression Model B22 predicting initial depressive predicting change in depres- symptoms sive symptoms b β p b <.001 -0.342 β p Constant 9.171 <.001 Female 1.332 .150 <.001 0.045 .031 .206 Age (in years at baseline) 0.213 .096 <.001 -0.006 -.016 .516 Socio-economic status (at baseline) -0.044 -.041 .069 0.007 .040 .107 1.905 .171 <.001 0.110 .061 .034 0.810 .043 .127 -0.022 -.012 .654 -0.708 -.117 <.001 -0.281 -.064 .026 Change in parental mental health problems (slope) by change in family climate (slope) 2.408 .016 .550 Initial parental mental health problems (intercept) by change in family climate (slope) -0.274 -.018 .509 Change in parental mental health problems (slope) by initial family climate (intercept) -1.198 -.025 .401 Risk factor Initial parental mental health problems (intercept) Change in parental mental health problems (slope) Protective factors Initial family climate (intercept) -3.259 -.277 <.001 Change in family climate (slope) Interactions between risk and protective factors Initial parental mental health problems (intercept) by initial family climate (intercept) 1 2 0.007 Linear regression Model A2 (n=1,643); model fit: R²=.176; F=58.177; linear regression Model B2 (n=1,643); model fit: R²=.024; F=3.701; b=unstandardized regression coefficient; β=standardized regression coefficient .000 .991 8 Supplementary Table 6. Social support moderating the association between parental mental health problems and depressive symptoms of children and adolescents Regression Model A31 regression Model B32 predicting initial depressive predicting change in depres- symptoms sive symptoms b β p b <.001 -0.342 β p Constant 8.830 <.001 Female 2.019 .227 <.001 0.047 .033 .194 Age (in years at baseline) 0.370 .167 <.001 -0.010 -.029 .235 Socio-economic status (at baseline) -0.037 -.035 .123 0.008 .044 .075 2.006 .180 <.001 0.114 .063 .027 0.762 .040 .153 -0.072 -.044 .100 -0.928 -.138 <.001 -0.207 -.057 .043 Change in parental mental health problems (slope) by change in social support (slope) -1.727 -.011 .706 Initial parental mental health problems (intercept) by change in social support (slope) -1.006 -.063 .026 Change in parental mental health problems (slope) by initial social support (intercept) 0.808 .019 .481 Risk factor Initial parental mental health problems (intercept) Change in parental mental health problems (slope) Protective factors Initial social support (intercept) -3.230 -.318 <.001 Change in social support (slope) Interactions between risk and protective factors Initial parental mental health problems (intercept) by initial social support (intercept) 1 2 0.329 Linear regression Model A3 (n=1,643); model fit: R²=.197; F=66.868; linear regression Model B3 (n=1,643); model fit: R²=.032; F=4.890; b=unstandardized regression coefficient; β=standardized regression coefficient .015 .518 9 Supplementary References 1. Darling N, Steinberg L, Akaike H (1987) Factor analysis and AIC. Psychometrika 52:317332 2. Steiger JH (1990) Structural model evaluation and modification - an interval estimation approach. Multivar Behav Res 25 (2):173-180. doi:10.1207/s15327906mbr2502_4 3. Bentler PM (1990) Comparative fit indexes in structural models. Psychol Bull 107 (2):238246. doi:10.1037/0033-2909.107.2.238 4. Winkler J, Stolzenberg H (1999) Der Sozialschichtindex im Bundes-Gesundheitssurvey (Social class index in the Federal Health Survey). Gesundheitswesen 61:178-183 5. Lange M, Kamtsiuris P, Lange C, Schaffrath Rosario A, Stolzenberg H, Lampert T (2007) Messung soziodemographischer Merkmale im Kinder- und Jugendgesundheitssurvey (KiGGS) und ihre Bedeutung am Beispiel der Einschatzung des allgemeinen Gesundheitszustands (Sociodemographic characteristics in the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) - operationalisation and public health significance, taking as an example the assessment of general state of health). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50 (5-6):578-589. doi:10.1007/s00103-007-0219-5 6. Fendrich M, Weissman MM, Warner V (1990) Screening for depressive disorder in children and adolescents: validating the Center for Epidemiologic Studies Depression Scale for Children. Am J Epidemiol 131 (3):538-551 7. Klaghofer R, Braehler E (2001) Konstruktion und teststatistische Prüfung einer Kurzform der SCL-90-R (Construction and validation of a short form of the SCL-90-R). Z Klin Psychol Psychiatr Psychother 49 (2):115-124 8. Radloff LS (1977) The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1 (3):385-401. doi:10.1177/014662167700100306 10 9. Barkmann C, Erhart M, Schulte-Markwort M, Group BS (2008) The German version of the Centre for Epidemiological Studies Depression Scale for Children: psychometric evaluation in a population-based survey of 7 to 17 years old children and adolescents - results of the BELLA study. Eur Child Adolesc Psychiatry 17 (Suppl. 1):116-124. doi:10.1007/s00787008-1013-0 10. Schwarzer R, Jerusalem M (1995) Generalized self-efficacy scale. In: Weinman J, Wright S, Johnston M (eds) Measures in health psychology: A user’s portfolio. Causal and control beliefs. NFER-NELSON, Windsor, UK, pp 35-37 11. Schwarzer R, Jerusalem M (1999) Skalen zur Erfassung von Lehrer- und Schülermerkmalen. Dokumentation der psychometrischen Verfahren im Rahmen der wissenschaftlichen Begleitung des Modellversuchs Selbstwirksame Schulen. Freie Universität Berlin, Institut für Psychologie, 12. Schneewind K, Beckmann M, Hecht-Jackl A (1985) Familienklima-Skalen. Bericht 8.1 und 8.2. Ludwig Maximilians Universität, Institut für PsychologiePersönlichkeitspsychologie und Psychodiagnostik, München 13. Donald CA, Ware JE (1984) The measurement of social support. Res Community Ment Health 4:325-370