Anaesthetics-MCQs-Phillip-Bembridge
advertisement
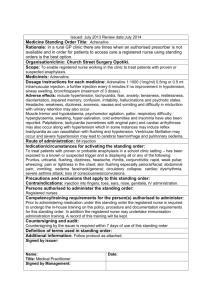
SINGLE BEST ANSWERS 1. You are an FY1 and are called to see a collapsed 28 yr old man, previously fit and well (ASA1) with a documented penicillin allergy. He took Co-amoxiclav orally 30 minutes ago. He has a marked rash, facial swelling, audible wheeze and stridor. Initial observations: HR 150/min, RR 40/min and BP 70/35 mm Hg. Oxygen has been administered and help summoned. The most appropriate immediate treatment is: A. B. C. D. E. Chlorphenamine 10 mg IM Hydrocortisone 200 mg IM Epinephrine (Adrenaline) 50 mcg IV titrated to effect Epinephrine (Adrenaline) 500 mcg IM Salbutamol 5 mg nebulised. Correct Answer: D. This is life threatening Anaphylaxis in a patient who has a known penicillin allergy and has been given a penicillin containing drug. A. and B. These are treatments to be given after initial resuscitation. C. IM administration of adrenaline is the route of choice for most healthcare professionals. (IV adrenaline would generally only be used by anaesthetists that have used it before.) D. Bronchodilators may be considered as part of management, but not first line treatment and this patient is not a known asthmatic (ASA1). It is worth knowing that Adrenaline will also cause bronchodilation. Ref: “Emergency Treatment of Anaphylactic Reactions”: Resuscitation Council 2008. ASA grades: American Society of Anesthesiologists’ physical status classification system. 2. At the end of a laparoscopic cholecystectomy on a 50kg patient (ASA 1) the general surgeon asks to use a local anaesthetic for wound infiltration to provide postoperative analgesia. The patient has no known drug allergies. An appropriate dose of local anaesthetic would be: A. B. C. D. E. Bupivacaine 0.25% 30mls Levobupivacaine 0.5% 30mls Lidocaine 0.5% 40mls Lidocaine 1% with adrenaline (1 in 200,000) 40mls Lidocaine 2% 10mls Correct Answer: A. All of these dilutions are available, however this patient’s weight is a limiting factor for local anaesthetic toxicity. Derivation of this answer relies on the correct use of maths and the knowledge of maximum recommended doses of commonly used local anaesthetics. Maximum recommended doses of local anaesthetics are to be found in BNF and any standard anaesthetic text: Lidocaine 3mg/kg (plain) and 7mg/kg with adrenaline. Bupivacaine/Levobupivacaine 2mg/kg. Adrenaline 4mcg/kg, maximum concentration 1 in 200,000 1ml of a 1% solution contains 10mg/ml 1 in 1000 solution contains 1mg/ml Further reading: A nomogram for calculating the maximum dose of Local Anaesthetic. D J Williams, J D Walker. Anaesthesia 2014, 69, 847-853. 3. A patient presents to the emergency department with sudden onset tachycardia 160/min and a blood pressure of 100/50 mm Hg. There are no other symptoms. An ECG shows no ischaemic changes, a QRS complex duration less than 0.12s and a regular R-R interval. Appropriate pharmacological treatment is: A. Adenosine 6mg B. Amiodarone 300mg D. Digoxin 0.5mg E. Esmolol 100 mg F. Verapamil 2.5 mg Answer: A Resuscitation council guidelines (2010) for the management of Narrow Complex Tachycardia in a stable patient recommends Adenosine, if vagal manoeuvres fail. Digoxin tries to rhythm control atrial fibrillation. Esmolol is for rate control of atrial fibrillation. Verapamil or diltiazem can be used for chronic tachycardia treatment if adenosine works initially. People often get confused with atropine, adenosine and amiodarone. Amiodarone stabilises the myocardium, and therefore it is used in VT or VF. Remember: M for Myocardium. (Check the shockable arm of the resuscitation guidelines.) Adenosine is used in narrow complex tachycardia, if it doesn’t work, or if the patient is unstable they need shocking back into a normal rhythm with DC synchronised cardioversion. Remember: DS for DC synchronised. (Check the ALS tachycardia algorithm.) Atropine is used in bradycardias if the patient is unstable, if there is no satisfactory response, transcutaneous pacing can be used (other drugs can be tried too, see the ALS bradycardia algorithm). Remember: TP for transcutaneous pacing. 4. You are asked to see a previously fit and well 60 year old ASA1 patient (70kg) on the ward who underwent a laparotomy for small bowel obstruction 12hrs ago. He has an epidural in situ for postoperative pain, containing 0.1% levobupivacaine with Fentanyl 2mcg/ml, running at 4ml/hr. His observations are BP 70/40 mmHg, HR 90/min and his urine output for the previous hour is 10mls. He tells you that he is feeling unwell. Initial management should be: A. B. C. D. E. Administer a broad spectrum antibiotic Administer high flow oxygen Give 500mls 0.9% NaCl Perform a 12 lead ECG Stop the epidural infusion Answer: B This patient is hypotensive and his urine output is low. He is in shock, which could be hypovolaemic, cardiac, septic or distributive (vasodilatation from epidural). However, the assessment and management should always follow the ABC approach – ensure an adequate airway, then give high flow oxygen and assess breathing. Ref: BTS Emergency Oxygen Guideline Group, Guidelines for emergency oxygen use in adult patients (2008). British Thoracic Guidelines. Thorax 63(sVI). https://www.brit-thoracic.org.uk/document-library/clinicalinformation/oxygen/emergency-oxygen-use-in-adult-patientsguideline/emergency-oxygen-use-in-adult-patients-guideline/ (This has a flow chart for use of emergency oxygen.)