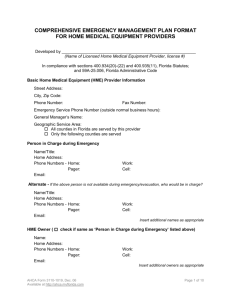
Table 2- Characterization of the studies on the use of heat and
advertisement

Table 2- Characterization of the studies on the use of heat and moisture exchangers as compared with the conventional humidifiers. STUDY/COUNTRY Martin et al., 1990/ SETTING ICU DATA ANALYSIS Quantitative variables STUDY LIMITATIONS were compared using the Student t test. COMPLICATIONS Pneumonia was diagnosed on the basis of Hypothermia in 22% and 12% of purulent secretion. It did not involve the patients belonging to the HME PAV incidence density. and HH groups, respectively (p < OTHER EVIDENCE BENEFITS LEVEL Not reported. 1C Not reported. 1C 1C 0.01). Six and no cases of tube occlusion were reported in the HME and HH groups, respectively (p < 0.01). The study was interrupted after the death of a patient belonging to the HME group due to total obstruction of the endotracheal tube. Roustan et al., 1992 ICU Both groups were compared using Sample size was not calculated. Nine the The randomization procedure was not endotracheal tube occlusion in the described. HME Student t, Mann- Whitney, Chi-square, and Fisher and and no events HH groups, exact tests for differences in respectively. frequency. episodes of atectasis in the HH Regression was conducted for the incidence of nosocomial Nine of and ten and HME groups, respectively. pneumonia, atelectasis, and tube occlusion. Dreyfuss et al., 1995 ICU The Student t test was used for the The randomization procedure was not Report of severe occlusion that The use of HME continuous variables. The Chi- described. required cannula exchange due to reduces costs and square test with Yates correction excluded after randomization. Sample clotting staff working time. was employed for the categorical size calculation was not reported. hematemesis) in the HME group. Various patients were (patients with variables. The Mann-Whitney test Six patients required cannula was exchange due to obstruction by used to compare non- parametric variables. Boots et al., 1997 ICU secretion in the HME group. The patients’ characteristics were The randomization procedure was not compared by paired t test. The described. Not reported. The use of HME 1C reduces costs. PAV rate was evaluated using the log rank test. Kirton et al., 1997 ICU Analysis of variance and non- Non-blinded study. ICU specifically paired Student t test. admitted trauma patients. The HME and HH groups did not The use of HME differ in terms of endotracheal reduces costs. 1C tube obstruction. Kollef et al., 1998 ICU Student t and Wilcoxon tests were The randomization procedure was not Tube obstruction was not detected The use of HME used (according to normal and described. No mention of blinded study. in any of the groups. reduces non-normal distribution). Time elapsed during filter exchange was Chi-square and exact Fisher tests not controlled. were PAV diagnosis criteria did not include employed to compare categorical variables. Results were costs 1C by 50%. bronchoalveolar lavage. confirmed by multiple logistic regression. Memish et al., 2001 ICU The Student t test was employed. The statistical power was not calculated. Not reported. Nursing staff spends 1C less time discarding the condensate that builds up in the circuit. The use of HME reduces costs. Lacherade et al., 2005 ICU The Student t test was employed Differences between the two populations Tube occlusion rates were lower On for continuous variables. The Chi- with respect to HIV infection. Phisicians in the HME group (1 case) as literature studies, the square test was used for the and researchers were not blinded. compared with the HH group (5 paper mentions that cases). the use of HME categorical variables. Multivariate logistic regression was also the basis of 1C reduces costs. performed. Boots et al., 2006 ICU Sample size was determined using Pneumonia was diagnosed according to HME the difference between two ratios. CPIS resistance to airflow than the (Clinical Pulmonary Infection may present higher The use of HME reduces costs. 1C Univariate analysis involved the manufacturer’s Score). use of Student t and Kruskal- specifications after use for 24 h. Wallis tests. The difference in PAV rate among groups was evaluated by Kaplan-Meier and log rank tests. Lorente et al., 2006 ICU Quantitative variables were Temperature and moisture were not compared using the Student t test. monitored. Five risk models proportional to confirmed by tracheal aspirate. After Cox were constructed for PAV randomization, patients under mechanical analysis. ventilation for less than five days were excluded. PAV Sample diagnosis calculation was Not reported. No benefits have been reported for the use of HME. was conducted, but it did not reach a suficiente number of patients. Wide confidence interval. Incidence density was not approached. Immunosuppressed patients were excluded. ICU: Intensive Care Unit; PAV: Pneumonia associated with mechanical ventilation; HME: Heat and moisture exchangers; HH: Heated Humidifiers. 1C