Dr. Ashok Kumar
advertisement

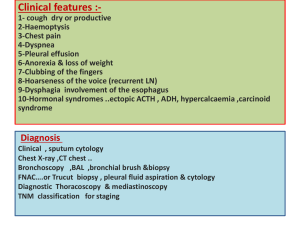
CASE REPORT CASE SERIES REPORT: 3 CASES OF USUAL AND UNSUAL PRESENTATION OF HYDATID DISEASE Sitaram Gothwal, Ashok Kumar, Sanjay Sharma, Mohit Sharma, Pradeep Gupta. 1. 2. 3. 4. 5. Professor. Department of General Surgery, SP Medical College, Bikanar, Rajasthan, India. Assistant Professor. Department of General Surgery, SP Medical College, Bikanar, Rajasthan, India. Assistant Professor. Department of General Surgery, SP Medical College, Bikanar, Rajasthan, India. Post Graduate Resident. Department of General Surgery, SP Medical College, Bikanar, Rajasthan, India. Post Graduate. Department of General Surgery, SP Medical College, Bikanar, Rajasthan, India. CORRESPONDING AUTHOR: Dr. Ashok Kumar, II/11.Nagnechiji Road, I/F S. P. Medical College Ground, Bikanar, Rajasthan. E-mail: drashokraj1@yahoo.co.in ABSTRACT: Hydatid disease (HD) is a zoonotic infection caused by Echinococcus granulosus and rarely by Echinococcus multilocularis. The disease is often manifested by slowly growing cystic masses and continues to be a significant health problem in many sheep-and cattle-raising areas [1]. Although the liver (75%) and lung (15%) are the most commonly involved organs, the disease can be seen anywhere in the body (10%) [2,3]. Hydatid disease (Echinococcus granuloma) is endemic in the middle east and other parts of the world, including India, Africa, South America, New Zealand, Australia, Turkey and South Europe [4-6]. The incidence of splenic involvement has been reported to be from 0.9% to 8% [1]. Primary splenic hydatidosis is quite rare and accounts for less than 2% [7]. It develops secondary to systemic dissemination or intraperitoneal spread from ruptured liver hydatid cysts. Here we are presenting a case series of 3 cases of hepatic and extra hepatic hydatid disease treated in our hospital successfully. Clinical symptoms in patients with hepatic locations of the disease included abdominal pain localized in the epigastrium or right upper quadrant of the abdomen, tenderness, hepatomegaly with palpable abdominal mass, jaundice, fever. Symptoms and surgical treatment for extrahepatic cysts varied according to the location of the cyst. All the patients were treated surgically. KEYWORDS: hydatid cyst, extrahepatic hydatid disease, hydatid disease INTRODUCTION: Hydatid disease is a parasite infection caused by the larval stage of the cestode. Echinococcus granulosus. It is endemic in many parts of the world, including India. Most frequently it affects the liver and lung. Involvement of spleen is uncommon, representing less than 2% to 3.5% of all human infestation by Echinococcus. CASE REPORT: 1. A 38 years female farmer presented with dull aching pain and gradually increasing Lump in Right Hypochondrium, Epigastrium, Left Hypochondrium and Left Lumber region over 11/2 years. There was history of Anorexia, weight loss and anemia. Examination revealed the multiple swelling in abdomen. Hepatosplenomegaly was present. Both liver and spleen were having irregular surface with multiple non-tender mass palpable over the surface. Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 15/ April 15, 2013 Page-2452 CASE REPORT 2. 3. On laboratory investigations revealed hemogram decrease Hb (8 gm%), mild increase in the Eosinophils counts (3%) and raised ESR 40 mm at the end of 1 hour. Liver function and Renal functions were normal, ultra-sound examination showed 7.5 x 8 cm cystic SOL with Internal membrane in postero-superior part of Right Lobe of liver and spleen enlarged up-to umbilicus. Two cystic SOLS internal membrane size 10 x 9.8 cm and 9.1 x 7 cm in spleen. CECT scan of abdomen revealed multiple, well defined cystic lesion-in the abdomen. In the cysts multiple septation suggestive of Hydatid disease. Patient was started on Albendazole 400mg b.d. per oral and prepare for surgery. Abdomen was opened with bilateral subcostal incisions. Splenectomy and excision of cyst from Right lobe of liver done. Peritoneal cavity thoroughly washed with Povidine iodine and normal saline. Post operative period was uneventful, oral Albendazole 400 mg b.d. started from 5th post operative day and was continued. Patient was discharged after 15 days; follow-up period was uneventful. A 18 years old female presented with c/o chronic bronchitis on/off from 3 months, dull aching type pain left upper quadrant on/off 3 months, mild grade fever on/off 3 months. Also h/o dog bite 15 years back. O/E she was anaemic, marked splenomegaly up-to umbilicus with hepatomegaly, b/l air entry decreased in both lower lobes of lungs. LFT/RFT within normal range, ESR 60 , eosinophilia ( 04%). USG abdomen-enlarged spleen 18.7 cm, 11x10 cm thin walled anechoic cystic lesion at upper pole of spleen, 8.7x6.4 cm thin walled anechoic cystic lesion with internal echo seen in lower pole of right lung s/o hydatid cyst. CECT revealed –splenic hydatid with b/l lung hydatid cyst. Albendazole 400 mg b.d. started pre-operatively and patient was prepared for OT. After all general evaluation patient was operated, left lung cyst was excised by left thoracotomy, cavity was washed with normal saline and Betadine and splenectomy was done by upper midline abdominal incision. ICDT and Abdominal drain was put, removed on post operative 5th day. Histo-pathologic reports confirmed the diagnosis. Post operative Albendazole started. Post-op recovery was uneventful and discharged Post-op 13th day. Follow-up also uneventful. This patient is further planned for right thoracotomy. A 22 years old female presented with c/o chronic bronchitis, dull aching type pain with heaviness in upper abdomen from 6 month and mild grade fever from last 20 days, h/o having pet dogs earlier. O/E she was anaemic, marked hepatosplenomegaly, air entry decreased right lower lobe of lung, LFT mildly raised, ESR-75, USG –enlarged spleen 16.8 cm, thin walled anechoic lesion approx 10x9.5 cm present at upper pole of spleen, right lung-10x10 cm, liver-13x8 cm, s/o hydatid cyst. CECT confers the USG reports. Treatment regime was same as in previous case i.e. pt was on Albendazole pre-operatively. She was operated by right thoracotomy and laparotomy by mid line incision. Splenectomy done with excision of hepatic and thoracic cyst. ICDT and abdominal drain no. 28 put into respective cavities and removed on post-op 5th day as in previous cases. HPR confirmed the diagnosis, post-op recovery was un-eventful. Follow-up also uneventful. DISCUSSION: Echinococcus granulosus, which is the causative agent of cystic hydatid disease (or cystic echinococcosis, CE); and Echinococcus multilocularis, which causes alveolar echinococcosis, AE [1,2] Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 15/ April 15, 2013 Page-2453 CASE REPORT The diagnosis of CE is based on the patient's history, clinical findings, haematological and serum biochemical profiles, and serological testing, which may be negative in 10% to 20% of cases. Efforts to improve diagnostic accuracy have led to integration of a range of imaging techniques into the diagnostic armamentarium. The radical surgical removal of the cystic lesion remains the mainstay of treatment with a high success rate. Chemotherapy, with benzimidazole compounds has also been used with some success to sterilize the cyst, decrease the chance of anaphylaxis, and reduce the complications and recurrence rate post-operatively. In recent years, Interventional radiologists and gastroenterologists have used minimal invasive procedures such as PAIR (puncture, aspiration, injection, re-aspiration) [8-10] and PEVAC (percutaneous evacuation of cyst content)[11] for treating hepatic echinococcosis and is indicated for patients who cannot undergo surgery. The study suggests that treatment of this benign disease should be the less radical surgical technique combined with pre-and postoperative anthelmintic administration. The surgical treatment should be combined with careful use of scolicidal fluids. REFERENCES: 1. Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. RadioGraphics 2003; 23:475–494; quiz 536–537 2. Engin G, Acunas B, Rozanes I, Acunas G. Hydatid disease with unusual localization. Eur Radiol 2000; 10:1904–1912 3. Gossios KJ, Kontoyiannis DS, Dascalogiannaki M, Gourtsoyiannis NC . Uncommon locations of hydatid disease: CT appearances. Eur Radiol 1997; 7:1303–1308 4. Altinors N, Senveli E, Donmez T, et al. Management of problematic intracranial hydatid cysts. Infection 1995;23:283-7. 5. Brown RA, Millar AJW, Steiner Z, et al. Hydatid cyst of the pancreas: a case report in a child. Eue J Pediatr Surg 1995;5:121-4. 6. Goel MC, Agarwal MR, Misra A. Percutaneous drainage of renal hydatid cyst: Early results and follow-up. Br J Urol 1995;75:724-8. 7. Durgun V, Kapan S, Kapan M, Karabicak I, Aydogan F, Goksoy E. Primary splenic hydatidosis. Dig Surg 2003; 20:38–41 8. Akhan O, Ozmen MN , Dincer A, Sayek I, Gocmen A: Liver hydatid disease: long-term results of percutaneous treatment. Radiology 1996, 198:259-264. 9. Brunetti E, Filice C, Macpherson C, Meslin F, Vuitton D, et al.: PAIR: Puncture, Aspiration, Injection, Re-aspiration. An option for the treatment of Cystic Echinococcosis. http://whqlibdoc.who.int/hq/2001/WHO_CDS_CSR_APH_2001.6.pdf] webcite WHO/ EMC web site Accessed on January 10, 2007 10. Smego RA Jr, Bhatti S, Khaliq AA, Beg MA: Percutaneous aspiration injectionreaspiration drainage plus albendazole or mebendazole for hepatic cystic echinococcosis: a meta-analysis. Clin Infect Dis 2003, 37:1073-1083. 11. Schipper HG, Lameris JS, van Delden OM , Rauws EA, 281 Kager PA: Percutaneous evacuation (PEVAC) of multivesicular echinococcal cysts with or without cystobiliary fistulas which contain non-drainable material: first results of a modified PAIR method. Gut 2002, 50:718-723. Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 15/ April 15, 2013 Page-2454 CASE REPORT CASE-1 CASE-2 CASE-3 Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 15/ April 15, 2013 Page-2455