Parasites affecting the CVS
advertisement

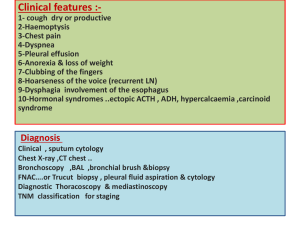
Parasites affecting the CVS Parasitic infections produce a wide spectrum of cardiac manifestations. They may involve various anatomic structures of the heart and are manifested clinically as myocarditis, pericarditis, pulmonary hypertension and hear failure. 1. Trypanosoma cruzi (Protozoa). 2. Trichinosis (Nematode). 3. Visceral larva migrans (Nematode). 4. Hydatid disease (Cestode). 5. Cysticercosis (Cestode). 6. Sparganosis (Cestode). 41 Protozoal infections Hemosomatic flagellates (Hemoflagellates) Genera: Two medically important genera-Trypanosoma and Leishmania. Overview: -Important pathogens of humans and livestock. -All species are transmitted by insects. -All have more or less complex cycles alternating from one morphologic form to another. -Distinguishing structural characteristics-flagellum, kinetoplast. -Basic morphologic stages: 1. Promastigote 2. Epimastigotes. 3. Trypomastigote 4. Amastigote 42 Differences between forms of blood flagellate Differences Promastigote Epimastigote Trypomastigote Amastigote Body Elongated Elongated Elongated rounded Kinetoplast Anteriorly In front of the nucleus. posteriorly Beside the nucleus Undulating membrane Absent short Long Absent Free flagellum Present Present Present Absent Habitat Leishmania assume this form in culture and inside insect vector. Trypanosome Present in the blood assume this form and lymph. inside the body and inside insect vector. vector 43 InR.E.S,some trypanosomes assume this form in tissues American Trypanosomiasis (T.Cruzi) Distribution: South and Central America. Morphology: The parasite takes two forms: 1. Trypomastigote form in the blood, it is commonly C or U shaped with a central nucleus and a large kinetoplast, the posterior end is sharp. It does not multiply in the blood. 2.Amastigote form in the cardiac muscles and reticulo-endothelial cells, (bone marrow, lungs ,spleen and liver), it divides by binary fission. 44 Transmission: 1 Vector: Winged bug-kissing bugs [Triatoma infestans]. 2 Reservoirs: armadillo, dogs and rodents. -The main method is through bugs’ bite, the infective stages are in the feces. -Blood transfusion. -Organ transplantation Life cycle: 1. The winged bug transmits T.cruzi, metacyclic trypanosomes in the feces of the bug contaminating skin abrasion will be engulfed by the skin macrophages (local histiocytes) and transform inside into amastigote forms which multiply by binary fission forming pseudocyst. 2. This produces a swelling in the skin called chagoma, after a period, the amastigote forms passing through a transitory epimastigote stage get metamorphosed into trypomastigote forms which reach the blood stream. 3. The cardiac muscle, R.E.S and the thyroid gland are invaded by the trypanosomes that cause damage to the affected organ. 45 Chagas disease The disease is characterized by: 1. Chagoma in the skin (bite reaction-non pustular, itchy painful swelling). 2. Acute stage , malaise, restlessness, lymphadenitis, hepatomegaly, splenomegaly, acute myocarditis with generalized edema. 3. Contamination of the eye could occur. The trypanosomes proliferate locally and produce unilateral orbital edema with enlargement of the of the ipsilateral lymph nodes. This is called Romana’s sign. 4. Acute stage when affecting the children could end with CNS invasion. 5. Thyroid insufficiency. 6. Cardiac affection with arrhythmia, in chronic phase, cardiomegally 46 and heart failure may develop. 7. Megaoesophagus and megacolon occur in chronic phase due to destruction of the parasympathetic nerve ganglia that leads to organ dilatation. Diagnosis: A) Direct methods: 1. Blood film examined as fresh smear or giemsa stained smear for detection of trypomastigotes. 2. Culture on N.N.N medium. B) Indirect methods: 1. Sero-diagnosis: IHA -ELISA for detection of antibodies against T. cruzi antigens. 2. PCR: for 3. Intradermal test: detection Cruzin test trypanosomes have been tried. Treatment: -Primaquine -Nifurtimox (Lampit). -Beznidazole (Radanil). Prevention and control: -Control of winged bugs. -Treatment of cases. -Destruction of the reservoir hosts. 47 of parasite DNA. using an antigen prepared from cultured Helminthic infections Trichinellosis (Intestinal and tissue nematodes) Infection with Trichinella spiralis is common in countries where pork is eaten raw or insufficiently cooked. Life cycle: Habitat: Small intestine embedded by its anterior part in the mucosa. Definitive host: Man. Intermediate host: Pigs. Reservoir host: Rats. Infective stage: The trichina capsule. Stages in the life cycle: Larva-trichina capsule adult. 48 Trichina Capsule: -It is the larval stage of Trichinella spiralis. -It is common in the striated active muscles as diaphragm, intercostal, deltoid, laryngeal and extra-ocular muscles. -It is ellipsoidal in shape. -Its size is about 0.5 X 0.2 mm. -It contains a larva coiled upon itself. -It becomes infective after 15 days from reaching the muscles. -Trichina capsule becomes calcified within 18 months but the larva inside remains viable for years. 49 Method of infection: Trichina capsule is the infective stage.Eating insufficiently cooked infected pig’s meat (pork) infects man. Life cycle: 1. The adults live in the small intestine of man and animals specially pigs and rats. 2. After fertilization males die and expelled. Females penetrate deeply in the mucosa and lay larva. Each female lays about 1500 larvae in its life span (about 2 months). 3. Larvae find their way to the circulation and passing through the pulmonary filter, they are distributed all over the body. They are found mainly in the skeletal muscles where they are encysted. 4. Larvae coil and encyst, they grow to reach a size of 1 mm taking about two weeks to become infective. 5. Man gets the infection through ingestion of raw or undercooked pork containing the trichina capsule. 6. Ingested larvae are liberated from the cyst in the small intestine where 50 they mature to adults. (Within 5 days after matting the female burrows deep in the mucosa and give birth to larvae. Pathology: 1. Stage of intestinal invasion by adult worms. 2. Stage of migration of the new born larvae: (7-21 days): Damage of the blood vessels occurs resulting in localized edema specially in the face and hands. Headache, fever, skin rash and edema of both eye lids with chemosis of the conjunctiva . 3. Stage of muscular penetration and encystment (after the third week):- The presence of trichina capsule in the muscles causes myositis with muscle tenderness and spasms In heavily infected cases , there is intense muscular pain, difficulty in breathing or swallowing with weakness of pulse The muscular invasion is followed by fibrosis and calcifications, that lead to muscle atrophy and weakness. 4. In heavy infection: myocardial involvement is common and it is considered as an important cause of death in fatal cases. The larvae that disseminate to the myocardium set up multifocal interstitial inflammatory lesions& no true cysts are formed in the cardiac muscle causing myocarditis. Electrocardiographic changes involve sinus tachycardia, prolongation of the P-R interval, primary T-wave changes and low QRS voltage. Various nervous disorders including hallucinations can occur. Diagnosis: 1. Clinical diagnosis: a) Larvae in blood stream (periorbital edema). b) Larvae in blood and the start of muscles' invasion (conjunctivitis-fever and chills-muscle pain-headache-eosinophilia-skin rashes-painful breathing). 51 c) Larvae in myocardium (tachycardia-edema of legs-hypotension-ECG changes and elevated cardiac enzymes. d) Larvae in brain meninges (headache -delirium-apathy or altered consciousness-stiff neck). 2. Laboratory Diagnosis: A) Blood examination: during the second week blood is examined for migrating larva. B) Muscle biopsy: Biopsy is taken from superficial muscle as the deltoid or intercostal. The excised muscle is examined either by: i) Compression: between 2 slides and examined for trichina capsule. ii) Sectioning and examined for trichina capsule. iii) Digestion in artificial gastric juice and the mixture is examined for the free larvae. C) Intra-dermal test (Bachman’s test): The antigen used is a purified extract of larvae collected by digestion of the infected pig’s meat .Intra-dermal injection of 0.1 ml of the antigen is followed by an immediate reaction in the forearm, a wheel surrounded by erythema appearing within 10-20 minutes. D) Serological tests: As the Bentonite flocculation test, ELISA, IFA and countercurrent electrophoresis. Treatment: 1 2 3 Corticosteroids. Fluids and electrolyte balance. Mebendazole. 52 Prevention and control: Trichinosis is common in countries consuming raw or insufficiently cooked pork. Rats are considered the reservoir hosts while pigs are the only source of infection to man. Visceral arva migrans (Tissue nematodes) It is the invasion of humans' viscera by the larvae of: 1. Dog Ascarides (Toxacara canis). 2. Cat Ascarides (Toxacara cati). Also human Ancylostoma, Ascaris and Strongyloides sterocaralis larvae. Pathology and clinical picture: Visceral larva migrans affects mostly children, probably because they are more likely to come in contact with dogs and cats ascarid eggs. Hypereosinophilia is very common, hepatomegally may be seen. In some cases pulmonary infiltration is seen with cough and fever (loeffler’s syndrome). Ocular larva migrans (granulomatous ophthalmitis) is rare, but its consequences may be severe. Toxocaral granuloma may be misdiagnosed as retinoblastoma. Cardiac involvement could occur with acute myocarditis in early phase and heat failure in chronic latent phase. Diagnosis: 1. Persistent eosinophilia, hepatomegally, loss of weight, joint pain is suspicious. 2. Biopsy from different organs may reveal the granuloma containing the larvae which are the only confirmatory method. 3. Cardiac manifestations and ECG changes. 53 4. Serologic and intradermal tests. Treatment: 1. Diethylcarbamazine (Hetrazan). 2. Thiabendazole (Mintezol). 3. Steroids. 54 Hydatid disease (Hydatidosis-Hydatid cyst) (Tissue Cestode) It is the presence of hydatid cyst (Larval stage of E.granulosus) in the human tissues. Methods of infection: Man is infected with hydatid cyst by swallowing the eggs of Echinococcus granulosus that are voided in the feces of dogs and wolves. Sites of hydatid cyst: Hydatid cysts may be found in any organ. The distribution as 58% in the liver, 27% in lungs and 15% in other organs including the heart. Pathology and clinical manifestations: It depends on its site. 1. Cardiac hydatid cyst: Cardiac hydatid cyst causes myocarditis in early phase, pericarditis with pleural effusion manifested by exertional dyspnea accompanied by a dry cough. Symptoms related to heart failure may develop in latent phase. 2. Hepatic hydatid cyst: discomfort in the right hypochondrium, hepatomegally , indigestion and jaundice. 3. Pulmonary hydatid cys: causes cough, chest pain and hemoptysis. 4. Cerebral hydatid cyst: symptoms of increased intra-cranial tension and epilepsy. 55 5. Osseous hydatid cysts: spontaneous fractures. 6. General: When hydatid cyst ruptures , escape of the fluid leads to allergic manifestations that vary from moderate as urticarial rash to severe anaphylactic shock. Diagnsosis: 1. Clinically by eliciting hydatid thrill and signs and symptoms according to the location. 2. ECG changes in cardiac involvement. 3. Ultrasonography and CT scan. 4. Laboratory techniques Indirect Techniques: A) Intradermal test (Casoni test): The antigen used is prepared from hydatid cysts of sheep. This is performed by intradermal injection of 0.25 ml of the antigen in one arm, in the other arm a control test is done. -The positive reaction is indicated by a wheel surrounded by erythema reaching its maximum width within 10-20 minutes. B) Serological tests as ELISA, complement fixation test andslide flocculation test. Direct Techniques: Biopsy is not preferable due to the fear of rupture of the cyst and the resultant complications'. Left thoracotomy and pericardiotomy are performed through to drain of hydatid fluid in case of pericardial effusion. Treatment: 1. Surgical removal. 2. Medical treatment: Mebendazole or Albendazole. 56