Documentation Tips for General Surgeons Enterotomies If an
advertisement
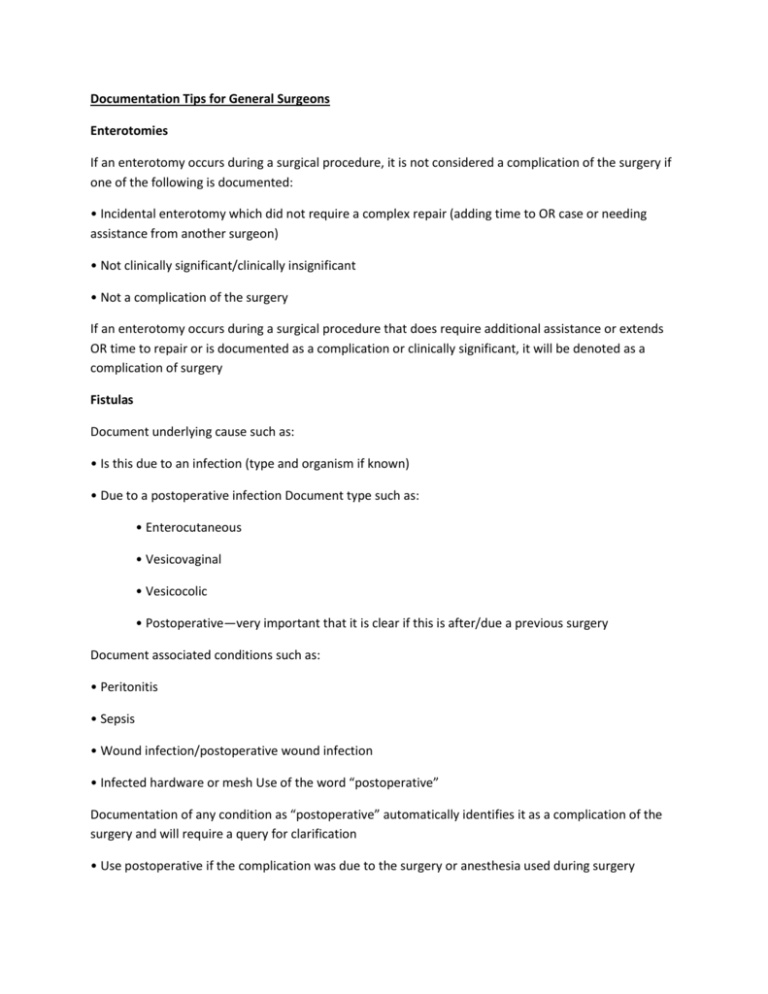
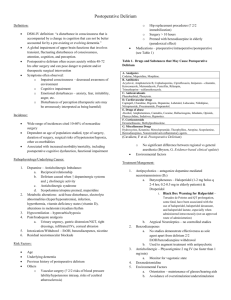
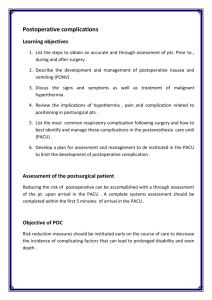
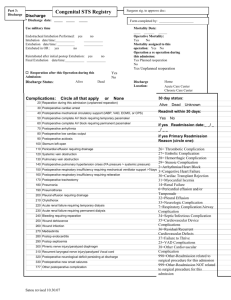
Documentation Tips for General Surgeons Enterotomies If an enterotomy occurs during a surgical procedure, it is not considered a complication of the surgery if one of the following is documented: • Incidental enterotomy which did not require a complex repair (adding time to OR case or needing assistance from another surgeon) • Not clinically significant/clinically insignificant • Not a complication of the surgery If an enterotomy occurs during a surgical procedure that does require additional assistance or extends OR time to repair or is documented as a complication or clinically significant, it will be denoted as a complication of surgery Fistulas Document underlying cause such as: • Is this due to an infection (type and organism if known) • Due to a postoperative infection Document type such as: • Enterocutaneous • Vesicovaginal • Vesicocolic • Postoperative—very important that it is clear if this is after/due a previous surgery Document associated conditions such as: • Peritonitis • Sepsis • Wound infection/postoperative wound infection • Infected hardware or mesh Use of the word “postoperative” Documentation of any condition as “postoperative” automatically identifies it as a complication of the surgery and will require a query for clarification • Use postoperative if the complication was due to the surgery or anesthesia used during surgery • Document all other conditions as “occurring after surgery” or “unrelated to surgery” to avoid an inappropriate complication being assigned or unnecessary query • When any provider uses postoperative this still applies—attending can “undo” this by noting in a subsequent PN and or DC summary that this condition was not a complication of the surgery Note: This tip sheet was donated Audrey G. Howard, RHIA, AHIMA-Approved ICD-10-CM/PCS Trainer, and Cheryl Manchenton, RN, BSN, 3M Consulting, adapted from the 2012 HCPro Inc., audio conference Inpatient Postoperative Complications: Resolve Your Facility’s Documentation and Coding Concerns