Preconditioning in patients undergoing esophagectomy: A ra
advertisement

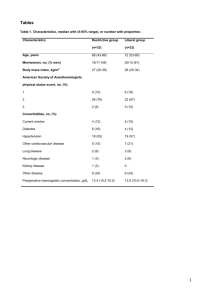
Preconditioning in patients undergoing esophagectomy: A randomized controlled pilot study H. Heynen1, C. de Jonge1, J. Willms2, H. Kerkkamp1, M.N. Sosef1 1 Dept. of Surgery, Atrium Medical Centre, Heerlen, The Netherlands, 2Dept. of Physical Therapy , Atrium Medical Centre, Heerlen, The Netherlands Esophagectomy in combination with neoadjuvant therapy is considered to be the optimal curative treatment for esophageal cancer. However, this treatment is associated with high morbidity and mortality rates. Optimizing cardiopulmonal status preoperatively by inspiratory muscle training has already been shown to significantly reduce the incidence of postoperative pulmonary complications and duration of hospital stay in patients undergoing coronary bypass graft surgery. This pilot study examines whether preconditioning in patients suffering from esophageal cancer, who are scheduled for esophagectomy, is feasible and will lead to better postoperative outcomes. Patients were randomly assigned to intervention or control group. The intervention group received daily inspiratory muscle training at home, supervised physical therapy twice a week, nutritional support once a week and psychological support if necessary. The intervention took place in the period between chemoradiation therapy and surgery. The control group received care as usual. Main outcome measures are feasibility, progression in general muscle strength, inspiratory muscle strength, nutritional status and quality of life. Secondary outcome measures are postoperative outcomes. A total of 20 patients was included, 11 in the control and 9 in the intervention arm. Two controls and 1 intervention patient withdrew from the study soon after randomization. One control subject started his own training program, similar to our intervention. There was a significant improvement in maximal inspiratory pressure in the entire group (paired t-test, p: 0,050), differences between the groups were not significant. The intervention group seemed to show less postoperative pulmonary complications, shorter duration of hospital stay and improved knee extensor and elbow flexor strength, although not significant . Bodyweight significantly reduced in the entire group (paired ttest, p: 0,011), but not significantly between the groups. Analysis of the psychological intervention and quality of life is still in progress. Conclusions: In our study we have found the organization of a preconditioning program to be feasible; patients were very eager to participate in the rehabilitation program and they noticed much improvement with regard to physical fitness. Although the results are mostly not significant, probably due to a low number of patients and available data, there seems to be a trend towards better outcomes in favour of the intervention group. We conclude that a large randomized trial is warranted.