VCU EM Journal Club
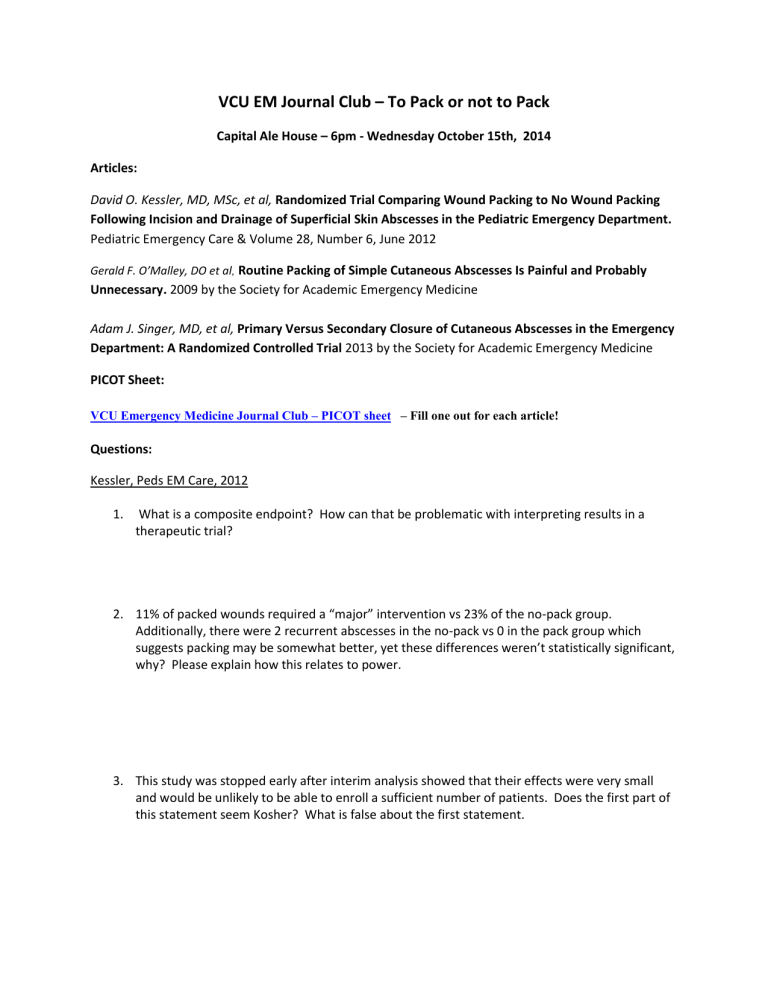
VCU EM Journal Club – To Pack or not to Pack
Capital Ale House – 6pm - Wednesday October 15th, 2014
Articles:
David O. Kessler, MD, MSc, et al, Randomized Trial Comparing Wound Packing to No Wound Packing
Following Incision and Drainage of Superficial Skin Abscesses in the Pediatric Emergency Department.
Pediatric Emergency Care & Volume 28, Number 6, June 2012
Gerald F. O’Malley, DO et al , Routine Packing of Simple Cutaneous Abscesses Is Painful and Probably
Unnecessary. 2009 by the Society for Academic Emergency Medicine
Adam J. Singer, MD, et al, Primary Versus Secondary Closure of Cutaneous Abscesses in the Emergency
Department: A Randomized Controlled Trial 2013 by the Society for Academic Emergency Medicine
PICOT Sheet:
VCU Emergency Medicine Journal Club – PICOT sheet – Fill one out for each article!
Questions:
Kessler, Peds EM Care, 2012
1.
What is a composite endpoint? How can that be problematic with interpreting results in a therapeutic trial?
2.
11% of packed wounds required a “major” intervention vs 23% of the no-pack group.
Additionally, there were 2 recurrent abscesses in the no-pack vs 0 in the pack group which suggests packing may be somewhat better, yet these differences weren’t statistically significant, why? Please explain how this relates to power.
3.
This study was stopped early after interim analysis showed that their effects were very small and would be unlikely to be able to enroll a sufficient number of patients. Does the first part of this statement seem Kosher? What is false about the first statement.
O’Malley, AEM, 2009
1.
Visual analog pain scales (VAS) were used in this study. Is this a valid measurement tool? What type of data does it generate? What is considered a clinically significant difference in VAS?
2.
Again, in this paper they used a composite outcome of need for intervention. Were there any elements of this composite which might be “less clinically relevant” that could hamper interpretation of the outcome?
3.
This study suffered from a significant number of subjects who did not follow-up at 48 hours.
How much does this threaten the validity of their results? How comfortable are you with the phone follow-up at 10-15 days?
4.
This study looked at their primary outcome using “intention-to-treat” principles. What does this mean, how is that different than a per-protocol analysis, and how could ITT analysis paradoxically not give you all the information you need to evaluate their therapy?
Singer, AEM 2013
1.
P-values were noticeably absent from their analysis. Did this bother you? How do you know if the differences observed were statistically significant?
2.
How does the convenience sample affect their study?
3.
The study found healing rates much higher than expected and did not have enough power to support Primary closure over Secondary. The study was powered to detect a 40% difference in healing rate at day 7. Notwithstanding the challenges of doing research, what do you think about choosing a 40% treatment effect?
4.
Overall wound healing at 7 days was 70% 1 0 closure vs 60% 2 0 closure. Similarly failures were
30% 1 0 closure vs 29% 2 0 closure. However, “need” for additional drainage was 22% 1 0 closure vs 14% 2 0 closure (absolute difference 9%, CI -17% – 30%). How must you interpret this