Barker et al. APNM_final_
advertisement

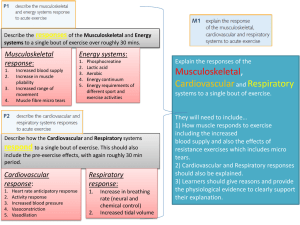
1 1 The effect of priming exercise on V O 2 kinetics, muscle O2 delivery and 2 utilisation, muscle activity and exercise tolerance in boys 3 4 Alan R. Barker, Emily Trebilcock, Brynmor Breese, Andrew M. Jones and Neil Armstrong 5 Children’s Health and Exercise Research Centre, Sport and Health Sciences, University of Exeter, 6 UK. 7 8 Corresponding author: 9 Dr Alan R. Barker 10 Children's Health and Exercise Research Centre 11 School of Sport and Health Sciences 12 University of Exeter 13 Exeter 14 EX1 2LU 15 Tel: 44 (0)1392 262766 16 Fax: 44 (0)1392 264706 17 Email: A.R.Barker@exeter.ac.uk 18 19 20 21 22 23 24 25 2 1 ABSTRACT 2 This study used priming exercise in young boys to investigate: 1) how muscle O 2 delivery and O2 3 O kinetics during exercise, and 2) whether the utilisation, and muscle activity modulate V 2 4 O kinetics following priming exercise can improve exercise tolerance. Seven 11.3 ± accelerated V 2 5 1.6 y old boys completed either a single bout (bout 1) or repeated bouts with 6 min recovery (bout 2) 6 O , muscle oxygenation, muscle of very heavy intensity cycling exercise. During the tests V 2 7 electrical activity and exercise tolerance were measured. Priming exercise most likely shortened the 8 O mean response time (change, ±90% confidence limits; -8.0 s, ±3.0), possibly increased the V 2 9 O amplitude (0.11 L·min-1, ±0.09) and very likely reduced the V O slow component phase II V 2 2 10 amplitude (-0.08 L·min-1, ±0.07). Priming resulted in a likely reduction in iEMG (-24% baseline, ±21 11 O (-0.16, ±0.11 and -0.09, ±0.05) and -25% baseline, ±19) and a very likely reduction in ΔHHb/Δ V 2 12 O response, respectively. A correlation was over the phase II and slow component portions of the V 2 13 present between the change in tissue oxygenation index during bout 2 and the change in the phase II 14 O amplitudes following (r=-0.72, likely negative) and slow component (r=0.72, likely positive) V 2 15 priming exercise, but not for muscle activity. Exercise tolerance was likely reduced (change -177 s, 16 O amplitudes in boys ±180) following priming exercise. The altered phase II and slow component V 2 17 following priming exercise are linked to an improved localised matching of muscle O 2 delivery to 18 O and not muscle electrical activity. Despite more rapid V O kinetics following priming V 2 2 19 exercise, exercise tolerance was not enhanced. 20 21 KEY WORDS 22 Oxidative metabolism, children, warm-up, muscle fibres. 23 24 25 3 1 INTRODUCTION 2 O ) kinetic response during exercise provides a non-invasive insight The pulmonary O2 uptake ( V 2 3 into muscle O2 uptake dynamics (Krustrup et al. 2009). Both cross-sectional and longitudinal studies 4 O kinetics during moderate (Fawkner et al. have demonstrated growth and maturation to slow V 2 5 2002; Breese et al. 2012), heavy (Fawkner and Armstrong 2004; Breese et al. 2010) and very heavy 6 (Breese et al. 2012) intensity exercise. These observations have been linked to age-related changes in 7 intramuscular phosphate dynamics (Barker et al. 2008a), muscle O2 extraction (Leclair et al. 2012), 8 muscle O2 delivery (Leclair et al. 2012) and/or muscle fibre recruitment patterns (Breese et al. 2012). 9 However, such mechanisms have been studied in isolation despite knowledge that these factors 10 O kinetics during exercise (Poole et al. 2008). interact to limit V 2 11 12 O kinetics in children or adolescents offers an alternative Investigating the limiting factors of V 2 13 O kinetics are altered during growth and maturation. In this approach to understanding why V 2 14 regard, a recent study found a bout of ‘priming’ (or prior) very heavy intensity exercise in 9-13 y old 15 O mean response time (MRT), increase the phase II V O amplitude and boys to reduce the V 2 2 16 O slow component amplitude during subsequent very heavy cycling exercise (Barker et reduce the V 2 17 al. 2010). These observations were reasoned to result from an improved muscle O2 availability, as 18 inferred from near infrared spectroscopy (NIRS) derived deoxyhaemoglobin (HHb) kinetics (Koga et 19 al. 2012). However, this study did not examine the dynamic matching of muscle HHb relative to 20 O during the exercise transient, which may provide additional insights into the factors limiting V 2 21 oxidative metabolism. A study on healthy young men found a bout of heavy intensity priming 22 O kinetics during subsequent moderate intensity exercise and this exercise to result in more rapid V 2 23 O ‘overshoot’ was related to an improved muscle O2 delivery as evidenced by an abolished HHb/ V 2 24 O dynamics shortly after the onset of exercise (Murias et al. 2011a). An ‘overshoot’ in the HHb/ V 2 25 O time constant (τ) > shortly after the onset of exercise is present in young adults with a phase II V 2 4 1 21 s, but not in those with more rapid phase II kinetics (Murias et al. 2011b), suggesting the 2 O kinetics may hypothesised ‘tipping point’ (Poole et al. 2008) for an O2 delivery dependency on V 2 3 O τ in the priming study by Barker et reside in this region. Interestingly, the group mean phase II V 2 4 al. (2010) was 22 ± 7 s for 9-13 y old boys, which sits strikingly close to the proposed tipping point 5 O kinetics. It is, however, currently unknown whether children for an O2 delivery dependency on V 2 6 O overshoot at the onset of exercise and if so, whether this can be abolished with display a HHb/ V 2 7 priming exercise. 8 9 In addition to altered muscle O2 delivery, muscle fibre type and motor unit recruitment strategies are 10 O kinetics during exercise (Jones et al. 2011; Barstow et al. 1996), and have known to impact V 2 11 O kinetics in adults (Layec et al. 2009; Burnley et al. 2002). been linked to the priming effect on V 2 12 O kinetics in Changes in muscle activation have been used to explain, in part, the slowing of V 2 13 youth following experimental manipulation of pedal rate (Breese et al. 2011) and baseline metabolic 14 O phase II and slow rate (Breese et al. 2012). It may be predicted therefore, that the altered V 2 15 component amplitudes previously reported by Barker et al. (2010) following priming exercise in 16 youth may be related, in part, to altered muscle activation strategies. This hypothesis, however, 17 remains to be tested. 18 19 O kinetics following priming exercise is consistent with an improved oxidative As the faster V 2 20 contribution to energy turnover and a smaller O2 deficit, an enhanced exercise tolerance may be 21 anticipated (Burnley and Jones 2007). However, a potential enhancement in exercise tolerance is 22 dependent on the recovery of intramuscular high-energy phosphates and fatigue-inducing metabolites 23 (e.g. Pi and H+) (Chidnok et al. 2013), which will be related to both the intensity of the priming bout 24 and the recovery duration between bouts (Bailey et al. 2009). We are, however, not aware of any 25 study that has investigated the potential for priming exercise to improve exercise tolerance in youth. 5 1 The purpose of the present study was to use priming exercise to further our understanding of the 2 O kinetics in boys. Specifically, we were interested in establishing: 1) how limiting factors of V 2 3 O kinetics during very heavy muscle O2 delivery and O2 utilisation, and muscle activity may limit V 2 4 exercise; and 2) whether priming exercise can improve exercise tolerance. We hypothesised that: 1) 5 O amplitudes following priming exercise will be related the altered phase II and slow component V 2 6 O and a blunted increase in muscle to an improved matching of muscle O2 delivery relative to V 2 7 O will enhance exercise tolerance. activity over time, and 2) the priming induced accelerated V 2 8 9 METHODS 10 Participants 11 Seven male participants volunteered to take part in the study (age: 11.3 ± 1.6 y; stature: 1.50 ± 0.13 m 12 and body mass: 42.0 ± 11.1 kg). All participants and their parent(s)/guardian(s) provided informed 13 assent and consent respectively, to partake in the project, which was approved by the institutional 14 ethics committee. The participants were healthy, recreationally active, and showed no 15 contraindications to exercise to exhaustion. 16 17 Experimental protocol 18 Participants visited the laboratory on four separate occasions over a 3 week period, with at least 24 19 hours rest provided between visits. All participants arrived at the laboratory in a rested state and were 20 requested to refrain from food and caffeine at least 2 hours prior to testing. The first laboratory 21 O session consisted of basic anthropometrical measures and an exercise test to determine maximal V 2 22 O max) and the gas exchange threshold (GET). During the subsequent three visits, the participants (V 2 23 completed either a single bout or double bouts of very heavy intensity exercise. All tests were 24 performed on an electronically braked cycle ergometer (Lode, Netherlands). 25 6 1 Visit 1: Incremental exercise. A combined ramp and supra-maximal exercise test to exhaustion was 2 O max and the GET (Barker et al. 2011b). The highest 15 s averaged V O employed to determine V 2 2 3 O max. The V O at the GET was identified as during the ramp or supra-maximal test was taken as V 2 2 4 O (Beaver et al. 1986) CO ) relative to V a disproportionate increase in expired carbon dioxide ( V 2 2 5 O and V CO (Wasserman et al. 2005). and verified using the ventilatory equivalents for V 2 2 6 7 Visits 2-4: Square-wave exercise. Each participant completed, in a randomized order, three exercise 8 protocols that consisted of a either a single or double bout of square-wave exercise: 1) 6 min of 9 cycling at 10 W followed by a single 6 min exercise transition to a power output equivalent to 60% ∆ 10 O max), and 2-3) 6 min of cycling at 10 W followed (60% of the difference between the GET and V 2 11 by two 6 min exercise transitions to a power output equivalent to 60% ∆, with 6 min of cycling at 10 12 W used as the recovery between the transitions. To provide a measure of exercise tolerance, the 13 participants were asked to exercise until exhaustion in protocol 1 and during bout 2 in protocol 3. 14 15 Experimental measures 16 Breath by breath gas exchange and ventilation were determined using a metabolic cart (Metalyser 3B 17 Cortex, Biophysik, Leipzig, Germany) that was calibrated prior to each test. Heart rate was recorded 18 using short range radio telemetry (Polar Vantage NV, Polar Electro, Kempele, Finland). 19 20 Changes in the concentrations of O2Hb and HHb of the left leg were measured non-invasively using a 21 commercially available near-infrared spectrometer (NIRO-300, Hamamatsu Photonics KK), as 22 previously described (Barker et al. 2010). The emitter-detector probe was affixed over the vastus 23 lateralis muscle, defined as the midway point between the greater trochanter and lateral epicondyle of 24 the left leg, using double sided adhesive tape and an elastic bandage to prevent movement during data 25 collection. As the relative contribution of haemoglobin and myoglobin to the NIRS signal is currently 26 unknown, the dynamics of O2Hb and HHb were considered to reflect changes in both haemoglobin 7 1 and myoglobin concentrations. The HHb signal is considered to reflect the dynamic (im)balance 2 between muscle O2 supply and O2 utilization and was used to provide a description of muscle O2 3 extraction (Koga et al. 2012). In addition, the tissue oxidation index (TOI) was used to describe the 4 oxygenation of the muscle during exercise. All NIRS variables were collected a 6 Hz, averaged into 5 1s intervals and expressed as a change from baseline, taken after 10 min of seated rest on the cycle 6 ergometer. 7 8 The neuromuscular activity of the vastus lateralis muscle of the right leg was determined using a four 9 channel surface EMG system (ME3000PB Muscle Tester, Mega Electronics), as previously described 10 (Breese et al. 2012). Briefly, following site preparation, graphite snap electrodes (Unilect 40713, 11 Unomedical, Stonehouse, UK) were adhered to the skin surface in a bipolar arrangement with an 12 interelectode distance of 20 mm, at the midway point between the greater trochanter and lateral 13 epicondyle of the right leg. The ground electrode was placed on the rectus femoris muscle of the right 14 leg. Additional experiments demonstrated that the use of the rectus femoris for the ground electrode 15 produced a similar EMG profile during square-wave exercise when compared to the tibial head (data 16 not presented). An elastic bandage was wrapped around the participant’s leg to prevent displacement 17 of the electrodes during cycling. All EMG measurements were sampled at 1000 Hz, between a 18 bandwith of 8-500 Hz with a common mode rejection ratio of 110 dB, gain of 305 and maximum 19 noise of 1.6 µV. The raw EMG signals were amplified (amplifier input impedance > 1 MΩ), collected 20 online and stored on a personal computer using MegaWin software (Mega Electronics) for subsequent 21 analysis. 22 23 Data analysis 24 O for each square-wave exercise bout were analysed using Breath by breath changes in V 2 25 methodology previously described from our laboratory (e.g. Barker et al. 2010; Breese et al. 2012; 26 Fawkner and Armstrong 2004). Following the removal of data lying greater than 3 SD from a local 27 moving mean, the repeat square-wave exercise transitions for bout 1 and bout 2 were interpolated to 1 8 1 O response for bout 1 and bout 2 were baseline s and averaged into 5 s data bins. The averaged V 2 2 O between -60 and -15 s from the exercise response. Following corrected by subtracting the mean V 2 3 removal of phase I (cardio-dynamic) by omitting the initial 15 s of data (Hebestreit et al. 1998), the 4 O response was characterised using the non-linear equation: phase II portion of the V 2 O V 2 5 (t) O A · (1 – e-(t-TD)/τ) = ΔV 2 Equation 1 6 O where V 2 7 O from baseline to its asymptote, time delay and the time constant of the response, respectively. V 2 (t), O A, TD and τ represent the value of V O at a given time (t), the amplitude of ΔV 2 2 8 9 Following the methods of Rossiter et al. (2002), equation 1 was initially fit up to the first 60 s of 10 exercise and then increased iteratively by 5 s to end-exercise (LabView, v 6.1, National Instruments, 11 Newbury, UK). The best fit curve for the phase II portion of the response was established using: 1) a 12 O τ against time, to identify the point at which the influence of the V O slow plot of the V 2 2 13 component lengthened the estimated τ following an initial plateau; and 2) deviation from an optimal 14 fitting of the model as judged by a systematic departure of the model’s residuals. The phase II 15 parameter estimates from equation 1 were then resolved by least-squares non-linear regression 16 O slow component (GraphPad Prism, GraphPad Software, San Diego, CA). The magnitude of the V 2 17 was calculated as the difference between the mean of the final 30 s at 6 min of exercise and the phase 18 O slow component amplitude was also expressed in relative terms using V O II asymptote. The V 2 2 19 at 6 min of exercise. To provide a description of the overall kinetic response (mean response time: 20 MRT), equation 1 with TD constrained to 0 s, was fit from exercise onset to 6 min of exercise. 21 22 The muscle HHb profiles were averaged into 5 s data bins, time aligned to exercise onset, and 23 ensemble averaged to yield a single response for the control and primed exercise conditions. The HHb 24 kinetics (primary and slow component phases) were modeled in a similar fashion to the procedures 25 O above, but with some slight modifications. The exponential-like increase in HHb described for V 2 9 1 after the onset of exercise occurred after a discernible delay. The time at which the exponential-like 2 increase in HHb commenced was identified as the point of a 1SD increase above baseline (DeLorey et 3 al. 2003). Equation 1 was then applied to resolve the HHb TD and τ following removal of the data 4 preceding the exponential-like increase. The HHb MRT was calculated by summing TD and τ to 5 provide an overall description of the kinetics in the primary phase. Changes in TOI were described at 6 baseline and 6 min of exercise. 7 8 O was calculated using two different methods, as described by Murias et al. The ratio of HHb to V 2 9 (2011a), to investigate the impact of priming exercise on the matching of O2 delivery to O2 utilization. 10 O (HHb/ V O ) was calculated at baseline, the primary Firstly, the absolute ratio of HHb and V 2 2 11 O (ΔHHb/Δ amplitude and at 6 min of exercise. Secondly, the ratio of the index of ΔHHb to Δ V 2 12 O ) was determined by normalizing the respective response profiles with 0% and 100% V 2 13 O signals were time representing baseline and 6 min of exercise respectively. The ΔHHb and Δ V 2 14 O data to account for phase I. The mean ΔHHb/Δ V O aligned by deleting the initial 15 s of the V 2 2 15 O kinetic response for each was calculated over the phase II and slow component phases of the V 2 16 O ratio of 1.00 represents an equivalent matching individual. At any given time a ΔHHb/Δ V 2 17 between muscle O2 delivery and O2 utilization to that observed at 6 min of exercise. Conversely, a 18 O ratio >1.00 or <1.00 theoretically represents either an increase or decrease in O 2 ΔHHb/Δ V 2 19 O compared to that observed at 6 min of exercise. extraction respectively, for a given V 2 20 21 The raw EMG data were analysed within MegaWin software (Mega Electronics). The EMG signal 22 was initially filtered using a high and low pass of 20 Hz and 500 Hz respectively. A second-order 23 Butterworth filter was then employed to remove contamination from movement artifacts, rectified and 24 integrated over a 15 s time bin. The iEMG signal was then time aligned to exercise onset and 25 ensemble averaged to yield a single response for the control and primed exercise conditions. The 10 1 iEMG data were expressed as a percentage change from the amplitude recorded whilst cycling at 10 2 W during bout 1 prior to the square-wave exercise transition. The iEMG response was then analysed 3 O slow by calculating the mean iEMG amplitude between baseline and the onset of the V 2 4 O slow component to 6 min of exercise. In addition, the change in component, and from the V 2 5 O slow component to 6 min was quantified using linear iEMG over time from the onset of the V 2 6 regression (GraphPad Prism, GraphPad Software, San Diego, CA) as previously described (Breese et 7 al. 2012). 8 9 Statistical analyses 10 In line with recent statistical recommendations (Hopkins et al. 2009), we used 90% confidence limits 11 (CL) to calculate probabilistic magnitude based inferences for the observed effect of priming exercise 12 O kinetics, muscle HHb and iEMG dynamics, and exercise tolerance. Using a published on V 2 13 spreadsheet (Hopkins 2007), the mean difference between the physiological variables in bout 1 and 14 bout 2 were calculated with a 90% CL to represent the uncertainty of the true effect. In the absence of 15 data concerning the smallest worthwhile change for the physiological outcomes reported in the current 16 study, Cohen’s (1988) standardised mean of 0.2 was employed, as recommended by Batterham and 17 Hopkins (2006). Based on the smallest worthwhile change, the probability that the observed effect 18 was beneficial, trivial or harmful was calculated using the spreadsheet. The following probability 19 thresholds were used to inform these decisions: <0.5%, most unlikely; 0.5-5%, very unlikely; 5-25%, 20 unlikely; 25-75%, possibly; 75-95%, likely; 95-99.5%, very likely; >99.5%, most likely (Batterham 21 and Hopkins 2006; Hopkins et al. 2009). An effect was deemed trivial when the majority (>50%) of 22 the 90% CL lay between beneficial and harmful. Conversely, an effect was deemed unclear when the 23 likelihood of a beneficial and harmful effect was >5%. Pearson’s correlation coefficients and their 24 O kinetics and mechanistically 90% CL were used to explore the relationship between changes in V 2 25 important variables (e.g. muscle TOI) following priming exercise. Probabilistic based inferences for 26 the smallest worthwhile correlation were calculated, as described above for the changes in means. 11 1 Descriptive statistics were calculated using SPSS (version 19.0, Chicago, USA) and presented as 2 mean ± SD. 3 4 RESULTS 5 Ramp and supra-maximal exercise 6 O max, maximal heart rate and peak power output was 2.12 ± 0.56 L·min-1, 192 ± The group mean V 2 7 O of 1.20 ± 0.28 L·min-1 8 beats·min-1 and 170 ± 57 W, respectively. The GET occurred at a V 2 8 O max. The mean power output at 60% ∆ was 124 ± 47 W. which represented 59 ± 16% V 2 9 10 O kinetics V 2 11 O response during the control and primed cycling exercise bouts is shown in The group mean V 2 12 O kinetic response parameters. Baseline Figure 1. Table 1 provides the inferential statistics for the V 2 13 O was possibly lower in bout 2 compared to bout 1 (ES=-0.21). The influence of priming exercise V 2 14 on the phase II τ (ES=-0.35) and TD (ES=-0.17) was unclear but the phase II amplitude (ES=0.23) 15 and gain (ES=0.74) were possibly and very likely higher respectively, in bout 2 compared to bout 1. 16 O responses and was lower both in absolute (likely, ES=A slow component was manifest in all V 2 17 O MRT was 0.92) and relative terms (very likely, ES=-1.17) in bout 2 compared with bout 1. The V 2 18 most likely reduced in bout 2 (ES=-1.07). 19 20 Muscle oxygenation kinetics 21 The group mean HHb and TOI response profiles during bout 1 and bout 2 are shown in Figure 2 with 22 the HHb kinetic parameters presented in Table 2. Bout 2 was associated with a very likely reduced 23 HHb (ES=-0.62) and a very likely higher TOI (bout 1: 66.8 ± 2.9 vs. bout 2: 71.5 ± 3.7; change, 24 95%CL: 4.7, ±2.4, ES=1.23) at baseline. The HHb TD was very likely reduced in bout 2 (ES=-0.99), 25 although priming exercise had an unclear effect on HHb τ (ES=0.04) and MRT (ES=-0.44). The 26 primary amplitude for HHb was likely higher (ES=0.31) in bout 2 but priming exercise had an unclear 12 1 effect on the HHb slow component (ES=0.11). End-exercise HHb was possibly lower in bout 2 but 2 the increase in HHb above baseline was possibly higher in bout 2 (bout 1: 8.2 ± 4.3 vs. bout 2: 9.4 ± 3 3.6; change: 1.3, ±1.1, ES=0.28). End TOI (bout 1: 52.4 ± 4.5 vs. bout 2: 54.2 ± 4.5; change: 1.8, 4 ±1.8, ES=0.35) was likely higher in bout 2. Baseline TOI in bout 2 had a likely positive relationship 5 O amplitude following priming exercise (r=0.57, ±0.54) but an with the change in the phase II V 2 6 O slow component amplitude (r=-0.47, ±0.59). The unclear relationship with the change in the V 2 7 delta change in TOI from baseline to 6 min during bout 2 had a likely negative relationship with the 8 O amplitude (r=-0.72, ±0.43) and a likely positive relationship with the change in the phase II V 2 9 slow component (r=0.72, ±0.43) amplitude, following priming exercise (Figure 3). 10 11 O Matching of HHb to V 2 12 O ratio was lower in bout 2 compared to bout 1 at baseline The magnitude of the absolute HHb/ V 2 13 (very likely, ES=-0.74), the primary phase (likely, ES=-0.33) and 6 min (likely, ES=-0.29) of exercise 14 O are shown in Figure 4 and show a (Table 2). The group mean normalized dynamics of ΔHHb/Δ V 2 15 O in bout 1 (A) compared to bout 2 (B). This profoundly altered adjustment of ΔHHb relative to Δ V 2 16 O response (Figure 4C). The mean normalized ΔHHb/Δ was captured in the normalized ΔHHb/Δ V 2 17 O response was likely higher (‘overshoot’, ES=0.88) than unity in bout 1 and very likely lower V 2 18 O region. At 6 min of exercise, the than unity (‘undershoot’, ES=-1.33) in bout 2 over the phase II V 2 19 O ratio remained likely higher than unity for bout 1 (1.02 ± 0.02, ES=0.81) normalized ΔHHb/Δ V 2 20 O was very but was unclear for bout 2 (1.00 ± 0.02, ES=-0.18). The mean normalized ΔHHb/Δ V 2 21 likely reduced in bout 2 compared to bout 1 over both the phase II (bout 1: 1.08 ± 0.11 vs. bout 2: 22 0.92 ± 0.07; change: -0.16, ±0.11, ES=-1.47) and slow component (bout 1: 1.05 ± 0.04 vs. bout 2: 23 0.96 ± 0.05; change: -0.09, ±0.05, ES=-1.64) phases. 24 25 iEMG 13 1 The group mean iEMG response during bout 1 and bout 2 is presented in Figure 5. The mean iEMG 2 response in bout 2 was likely reduced at baseline (bout 1: 100 ± 0 vs. bout 2: 82 ± 24%; change -18, 3 O slow component (bout 1: 253 ± 55 vs. bout 2: 229 ± ±18, ES = -0.91), up until the onset of the V 2 4 O slow component to 6 min of 79%; change -24, ±21, ES = -0.30) and from the onset of the V 2 5 exercise (bout 1: 251 ± 60 vs. bout 2: 227 ± 80%; change, 90% CL: -25, ±19, ES = -0.31). The 6 O slow component portion of the response was appearance of a linear slope for iEMG over the V 2 7 unclear for bout 1 (0.07 ± 0.17, ES=0.34) and bout 2 (-0.03 ± 0.08, ES=-0.28). Likewise, the linear 8 O slow component to 6 min of exercise was unclear between iEMG slope from the onset of the V 2 9 bouts (bout 1: 0.07 ± 0.17 vs. bout 2: -0.03 ± 0.08%; change: -0.09, ±0.14, ES = -0.61). The 10 O slow component and the change in iEMG over the slow component relationship between the V 2 11 region was unclear for bout 1 (r=-0.31, ±0.64) and bout 2 (r=0.02, ±0.68). The change in the iEMG 12 amplitude between bout 1 and 2 shared an unclear relationship with the change in the phase II 13 O amplitudes. (r=0.22, ±0.66) and slow component (r=-0.16, ±0.67) V 2 14 15 Exercise tolerance 16 Priming exercise resulted in a likely reduction in exercise tolerance (bout 1: 739 ± 248 vs. bout 2: 562 17 ± 181 s; change: -177, ±180, ES=-0.71), with an impaired exercise tolerance observed in all but one 18 participant. 19 20 DISCUSSION 21 In agreement with our earlier study (Barker et al. 2010), priming exercise resulted in a speeding of the 22 O MRT due to an increase in the phase II V O amplitude and a reduced V O slow component. V 2 2 2 23 O τ were unclear. However, the present study has revealed the following Changes in the phase II V 2 24 novel findings in young boys: 1) priming exercise increased baseline muscle TOI and caused subtle 25 adjustments to the dynamics of HHb by reducing the HHb TD; changes in the HHb primary τ and 26 O ratio by abolishing the MRT were unclear; 2) priming exercise reduced the normalized ΔHHb/Δ V 2 14 1 ‘overshoot’ that was present in bout 1 and causing an ‘undershoot’ in bout 2; 3) priming exercise 2 reduced muscle activity as inferred by a lower iEMG amplitude in bout 2 compared to bout 1; 4) large 3 relationships between indices of enhanced muscle O2 availability (e.g. baseline TOI, delta TOI) during 4 O phase II and slow component amplitudes following priming bout 2 and the change in the V 2 5 exercise were found. In contrast, changes in iEMG following priming exercise did not correlate with 6 O response; and 5) exercise tolerance was reduced by ~ 24% on average following the altered V 2 7 priming exercise. Collectively, these findings suggest that localized changes in both muscle O 2 8 O delivery and muscle O2 utilization, and not muscle activity, play an important role in limiting V 2 9 kinetics during very heavy exercise in youth. However, despite the more rapid adjustment of oxidative 10 metabolism brought about by priming exercise, this did not improve exercise tolerance. 11 12 Poole et al. (2008) have proposed that a ‘tipping point’ may exist with regard to the dependence of the 13 O τ on muscle O2 delivery. In this regard, it has been suggested that when the phase II phase II V 2 14 O τ > 21 s, the V O kinetic response becomes, in part, muscle O2 delivery dependent (Murias et V 2 2 15 O ratio al. 2011b; Murias et al. 2011a). This is based on the finding that the normalized ΔHHb/Δ V 2 16 O τ > 21 s, suggesting a greater demonstrated an ‘overshoot’ in adult participants with a phase II V 2 17 O , possibly due to a reduced microvascular rate of change in fractional O2 extraction relative to V 2 18 O2 delivery (Murias et al. 2011b). It is therefore interesting that in bout 1 of the current study the 19 O τ was 25.5 s and an overshoot in the normalized ΔHHb/Δ V O ratio (1.08) was mean phase II V 2 2 20 O region. This overshoot is identical to (1.08) that previously reported observed over the phase II V 2 21 in young adults with similar phase II kinetics (Murias et al. 2011a) and may suggest that the phase II 22 O τ is, in part, limited by muscle O2 delivery in young people. In support of this reasoning is V 2 23 O τ in children during cycling exercise during hypoxia (15% O2) evidence of a slowed phase II V 2 24 O τ during conditions (Springer et al. 1991). However, evidence of a speeding of the phase II V 2 15 1 when muscle O2 delivery is elevated is needed to fully support the view that muscle O2 availability 2 O kinetics in youth. limits V 2 3 4 In the current study the priming intervention elevated muscle O2 availability during bout 2, as 5 evidenced by the increased TOI at baseline and throughout exercise. In addition, as recently shown in 6 O young healthy adults (Murias et al. 2011a), priming exercise reduced the normalized ΔHHb/Δ V 2 7 O to 0.92 on average, suggesting a better matching of localized muscle O2 ratio during phase II V 2 8 delivery to O2 utilization during the exercise transient, implying that a reduced rate of O2 extraction 9 O . However, despite this elevated muscle O2 availability in was required to meet the increased V 2 10 O τ was found, which is in bout 2, an unclear effect for priming exercise on the phase II V 2 11 agreement with an earlier study from our laboratory using the same priming intervention in 9-13 y old 12 O τ in young boys (Barker et al. 2010). This finding therefore supports the notion that the phase II V 2 13 boys is principally limited by intramuscular metabolic factors, likely related to the creatine kinase 14 mediated splitting of muscle PCr and/or the activity of rate limiting oxidative enzymes (Poole et al. 15 2008; Kindig et al. 2005; Meyer 1988). Such a conclusion is indirectly supported by the similar 16 O and muscle PCr at the onset and offset of exercise in young people (Barker kinetics for phase II V 2 17 et al. 2008b). 18 19 An interesting finding in the current study was the presence of a reduced HHb TD following priming 20 exercise. This is likely to reflect an earlier mismatch between muscle O2 delivery and utilization 21 during bout 2, suggesting an enhanced O2 extraction early (initial ~ 5 s) in the exercise transient. This 22 occurred despite an elevated muscle O2 availability during the baseline of bout 2, and may reflect a 23 more rapid activation of oxidative metabolism, possibly due to an increased activity of rate-limiting 24 oxidative enzymes, such as pyruvate dehydrogenase (Gurd et al. 2009), and/or activation of the 25 mitochondrial electron transport chain (Gandra et al. 2012). Following the HHb TD, however, HHb 26 rose with exponential-like kinetics but the resulting HHb τ and MRT (TD + τ) was found to have an 16 1 unclear effect following priming exercise, suggesting the overall dynamic balance between muscle O 2 2 delivery and O2 utilization during the primary phase was unaltered by priming exercise. While this 3 finding agrees with previous studies in adults (DeLorey et al. 2007; Murias et al. 2011a), it contrasts 4 the recent work form our laboratory showing no changes in the HHb profile (TD, τ or MRT) following 5 priming exercise in young boys (Barker et al. 2010). Such inter-study differences in HHb dynamics 6 have also been reported across similar adult studies (DeLorey et al. 2007; Gurd et al. 2009; Murias et 7 al. 2011a), and may be explained by the heterogeneity in the HHb response dynamics that is observed 8 across the quadriceps muscle (Koga et al. 2007). 9 10 In agreement with earlier investigations in children and adults (Bailey et al. 2009; Barker et al. 2010; 11 O amplitude was elevated following Burnley et al. 2002; Burnley et al. 2001), the phase II V 2 12 O phase II gain. As shown previously in adults priming exercise, resulting in an increase in the V 2 13 O (Burnley et al. 2001), this was independent of an elevated baseline metabolic rate, as baseline V 2 14 during bout 2 had returned to, and was possibly lower than bout 1. Based on unchanged HHb (muscle 15 O2 extraction) dynamics and an increase in bulk blood flow (Q), we recently interpreted this to be 16 caused by an improved muscle O2 delivery (Barker et al. 2010). The current study extends this 17 O amplitude following priming exercise was positively interpretation as the change in the phase II V 2 18 correlated with bout 2 baseline TOI (r=0.57) and negatively with the delta change in TOI during bout 19 2 (r=-0.72). However, in addition to a potential role for muscle O2 delivery, the elevated phase II 20 O amplitude following priming exercise has been linked to an increase in muscle activation V 2 21 (Burnley et al. 2002; Layec et al. 2009). For example, Burnley et al. (2002) reported an elevated 22 iEMG during heavy intensity cycling following priming exercise, which was proportional to the rise 23 O amplitude. In the current study, however, we observed a reduced iEMG in the phase II V 2 24 O portion of the response, which according to previous amplitude during the phase II V 2 25 interpretations in adults (Burnley et al. 2002; Layec et al. 2009; Bailey et al. 2009), suggests a 26 reduction in motor unit recruitment. Unlike indices in muscle O2 availability, however, the reduction 17 1 O amplitude following priming in iEMG did not correlate with the increase in the phase II V 2 2 exercise. This finding does not support a mechanistic role for muscle activation in altering the phase II 3 O amplitude in young boys following priming exercise, which is in agreement with the adult data V 2 4 of Scheuermann et al. (2001). Rather, coupled with the elevated muscle O2 availability at the onset of 5 exercise, priming exercise may have increased the distribution of O2 to the active muscle fibres, with 6 O amplitude. the outcome being an elevated phase II V 2 7 8 O amplitude in the current study could relate An alternative explanation for the increased phase II V 2 9 to the possibility that muscle efficiency was reduced following priming exercise. For example, Sahlin 10 O amplitude following high-intensity priming exercise et al. (2005) reported an elevated phase II V 2 11 under conditions of elevated muscle and blood lactate and reduced muscle PCr, which remained until 12 end exercise (10 min). These authors and others (Jones et al. 2008) have suggested that residual 13 muscle fatigue from the initial priming bout may reduce muscle efficiency. However, not all data 14 support this notion (Layec et al. 2009), and it is pertinent to note that the increased O2 cost of exercise 15 in the present study was abolished by 6 min of exercise (see Figure 1), suggesting that if exercise 16 efficiency was altered in the present study, it was confined to the earlier portion of the bout. 17 18 O slow component during high-intensity exercise has been shown to originate Over 80% of the V 2 19 from the exercising limbs (Poole et al. 1991) with the progressive recruitment of muscle fibres, 20 specifically high-order type II fibres, considered to be the main mechanism (Endo et al. 2007; 21 Krustrup et al. 2004; Barstow et al. 1996). In this context it is pertinent to note that during bout 1 or 22 O slow component bout 2 we did not observe a meaningful linear rise in iEMG over time over the V 2 23 region. Furthermore, while priming exercise reduced both the relative (56%) and absolute (58%) 24 O slow component amplitude in the current study, this was not correlated with iEMG, despite the V 2 25 reduced iEMG amplitude in bout 2. This lack of a association between changes in iEMG and the 26 O slow component corroborates some (Scheuermann et al. 2001) but not all (Bailey et al. 2009; V 2 18 1 Burnley et al. 2002) previous adult work, and provides support for the notion that the progressive 2 O recruitment of muscle fibres per se, is not mechanistically linked to the development of the V 2 3 slow component in young boys. Our study cannot, however, discount the possibility that the metabolic 4 cost associated with the recovery of previously active muscle fibres (e.g. Vanhatalo et al. 2011) plays 5 O slow component in young people. an important role in the development of the V 2 6 7 O slow component amplitude in the current study may An alternative explanation for the reduced V 2 8 be related to an elevated bulk O2 delivery and/or the matching of muscle O2 availability to O2 9 utilization (DeLorey et al. 2007; Gurd et al. 2009; Murias et al. 2011a). We recently reported in young 10 O slow component following priming exercise was observed with an elevated boys that a reduced V 2 11 O ratio, although it could not be concluded that the elevated cardiac output (bulk blood flow) to V 2 12 bulk blood flow resulted in an increased muscle O2 availability (Barker et al. 2010). The present study 13 extends this work and provides evidence that an increase in muscle O2 availability was related to the 14 O slow component amplitude. Firstly, we observed a correlation between the reduction in the V 2 15 O slow component following priming exercise and TOI at baseline of bout 2 (r=change in the V 2 16 0.47) and the change in TOI from baseline to 6 min of exercise in bout 2 (r=0.72). Secondly, the 17 O over the slow component region was markedly reduced from mean normalized ratio of ΔHHb/Δ V 2 18 1.05 to 0.96 with priming exercise, suggesting a better matching of localized muscle O2 delivery to 19 O . It has been proposed that the enhanced muscle O2 availability afforded by priming exercise V 2 20 reduces the rate of fatigue development, presumably by reducing the muscle metabolic perturbation 21 (e.g. fall in PCr and increase in Pi and H+) (Hogan et al. 1999), and the requirement to recruit 22 additional (high-order) muscle fibres during high-intensity exercise (Jones et al. 2011). This may 23 account for the reduced iEMG amplitude reported following priming exercise in the present study, but 24 as mentioned earlier, no meaningful correlation was observed between changes in iEMG and the 25 O kinetic response. V 2 19 1 2 O kinetics, and presumably a reduction in the muscle O2 deficit Despite observing faster overall V 2 3 following priming exercise, we observed a 24% reduction in time to exhaustion (likely reduced), with 4 six out of the seven participants having a reduced exercise tolerance. This finding agrees with some 5 previous adult studies which have reported an impaired exercise tolerance following very heavy 6 intensity priming exercise (Ferguson et al. 2007; Carter et al. 2005). However, others have reported 7 either an unchanged (Koppo and Bouckaert 2002) or enhanced exercise tolerance (Bailey et al. 2009) 8 following priming exercise. It is well established that the tolerable duration of high-intensity exercise 9 is well described by a hyperbolic function of time, the asymptote of which is termed critical power 10 (CP), and the curvature constant (W’) which describes a finite amount of work that can be completed 11 above CP (Jones et al. 2010). In adults (Poole et al. 1988), but not children (Barker et al. 2011a), 12 O max due to constant work-rate exercise above CP until exhaustion occurs with the attainment of V 2 13 O slow component. Consequently, the kinetics of V O , V O max, CP and W’ the presence of the V 2 2 2 14 all have the potential to determine exercise tolerance during high-intensity exercise (Burnley and 15 O max (Ferguson et al. 2007; Jones 2007). However, as priming exercise does not alter CP or V 2 16 O slow component was attenuated following priming exercise Vanhatalo and Jones 2009), and the V 2 17 in the current study, our observed reduction in exercise tolerance is likely to be explained by an 18 altered W’. Indeed, a recent study has suggested that the restoration of muscle metabolic status (e.g. 19 PCr, H+) towards baseline levels is likely to be of importance in determining exercise tolerance above 20 CP (Bailey et al. 2009), and has recently been confirmed experimentally in humans (Chidnok et al. 21 2013). In the context of the present study it is likely that the 6 min recovery duration employed was 22 insufficient for sufficient recovery of W’ (related to restoration of muscle PCr and H+) prior to the 23 second bout of exercise. Therefore, although children are reportedly characterized with a more rapid 24 muscle metabolic recovery following high-intensity exercise compared to adults (Ratel et al. 2006), 25 the 6 min recovery duration used between the exercise bouts in the current study is unlikely to have 26 been sufficient to restore muscle PCr and H+ back to baseline prior to the second bout of exercise. A 20 1 recovery period of ≥ 6 min, is therefore likely to be needed to realize an enhancement in high- 2 intensity exercise tolerance following priming exercise of an intensity (60% Δ) and duration (6 min) 3 used in the current study. 4 5 Considerations and limitations 6 The findings in the present study should be viewed in relation to the following considerations. Firstly, 7 O ratio is typically expressed relative to the steady-state responses the normalized ΔHHb/Δ V 2 8 achieved during moderate intensity exercise (Murias et al. 2011a; Murias et al. 2011b). As a steady- 9 O state is not observed during very heavy exercise (i.e. > CP) in youth, the normalized ΔHHb/Δ V 2 10 ratio was expressed relative to the amplitudes obtained at 6 min of exercise. Despite this different 11 O over the phase II region was approach, the magnitude of the overshoot in normalized ΔHHb/Δ V 2 12 similar to that previously reported in young adults (Murias et al. 2011b), and was meaningfully 13 blunted following priming exercise, which is also consistent with previous adult work during 14 moderate exercise (Murias et al. 2011a; De Roia et al. 2012). Secondly, similar to previous studies 15 O (De Roia et al. 2012; DeLorey et al. 2007; Murias et documenting changes in HHb relative to V 2 16 al. 2011b), we obtained the HHb signal from a single probe positioned over the vastus lateralis 17 muscle. As large variations in the HHb response dynamics, and by inference the matching of muscle 18 O2 delivery to utilization, exist both within and between the quadriceps muscle (Koga et al. 2007; 19 O . Finally, Koga et al. 2011), this may limit the fidelity in relating HHb dynamics to whole body V 2 20 muscle activity in the present study was quantified using surface iEMG over the vastus lateralis 21 muscle, which is in accord with previous adult research in this area (Scheuermann et al. 2001; Bailey 22 et al. 2009). Although the vastus lateralis muscle is progressively recruited throughout very heavy 23 exercise, at least in adults (Endo et al. 2007), it cannot be discounted that the use of a single site 24 iEMG measure in the current study may have resulted in an incomplete picture with regard to changes 25 in muscle activity following priming exercise. For example, some adult studies have undertaken a 26 more comprehensive measure of muscle activity (gluteus maximus, vastus lateralis, vastus medialis) 21 1 O following priming exercise and observed an increase in iEMG amplitude over the phase II V 2 2 portion of the response (Burnley et al. 2002). However, it should be noted that the iEMG data in the 3 O slow current study are consistent with a recent study documenting an increase in iEMG over the V 2 4 component region in men but not boys (Breese et al. 2012). 5 6 CONCLUSIONS 7 The present study employed simultaneous measurements of muscle O2 delivery, O2 utilization and 8 O kinetics and muscle activity following priming exercise to better understand the factors limiting V 2 9 O high-intensity exercise tolerance in youth. Priming exercise resulted in more rapid overall V 2 10 O response returning closer to mono-exponentiality due to an increased phase II kinetics with the V 2 11 O amplitude and a reduction in the V O slow component. Mechanistically these changes were V 2 2 12 O as evidenced by a reduction related to an improvement in the matching of muscle O2 delivery to V 2 13 O and an association with an elevated TOI before and during the second bout of in ΔHHb/Δ V 2 14 exercise. While muscle activity, as measured using iEMG, was reduced following priming exercise, 15 O kinetics. Finally, despite the enhanced aerobic energy this did not correlate with the altered V 2 16 provision following the priming intervention, exercise tolerance was reduced by 24% on average, 17 possibly due to an insufficient recovery period between exercise bouts that did not permit adequate 18 recovery of the muscle metabolic status towards baseline. 19 20 ACKNOWLDGEMENTS 21 We would like to thank the participants for their time and commitment to this project. We also 22 acknowledge the laboratory support provided by Mr David Childs and Mr Owen Tomlinson. 23 24 REFERENCES 25 26 27 Bailey, S.J., Vanhatalo, A., Wilkerson, D.P., Dimenna, F.J. and Jones, A.M. 2009. Optimizing the "priming" effect: influence of prior exercise intensity and recovery duration on O2 uptake kinetics and severe-intensity exercise tolerance. J. Appl. Physiol. 107:1743-1756. 22 1 2 3 4 Barker, A.R., Bond, B., Toman, C., Williams, C.A. and Armstrong, N. 2011a. Critical power in adolescents: physiological bases and assessment using all-out exercise. Eur. J. Appl. Physiol. 112: 1359-1370. 5 6 7 8 9 10 11 Barker, A.R., Jones, A.M. and Armstrong, N. 2010. The influence of priming exercise on oxygen uptake, cardiac output, and muscle oxygenation kinetics during very heavy-intensity exercise in 9- to 13-yr-old boys. J. Appl. Physiol. 109:491-500. 12 13 14 Barker, A.R., Welsman, J.R., Fulford, J., Welford, D., Williams, C.A. and Armstrong, N. 2008b. Muscle phosphocreatine and pulmonary oxygen uptake kinetics in children at the onset and offset of moderate intensity exercise. Eur. J. Appl. Physiol. 102:727-738. 15 16 17 18 19 Barker, A.R., Williams, C.A., Jones, A.M. and Armstrong, N. 2011b. Establishing maximal oxygen uptake in young people during a ramp cycle test to exhaustion. Br. J. Sports. Med. 45:498-503. 20 21 Batterham, A.M. and Hopkins, W.G. 2006. Making meaningful inferences about magnitudes. Int. J. Sports. Physiol. Perform. 1:50-57. 22 23 Beaver, W.L., Wasserman, K. and Whipp, B.J. 1986. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 60:2020-2027. 24 25 26 27 28 29 30 31 32 33 34 Breese, B.C., Armstrong, N., Barker, A.R. and Williams, C.A. 2011. The effect of pedal rate on pulmonary O(2) uptake kinetics during very heavy intensity exercise in trained and untrained teenage boys. Respir. Physiol. Neurobiol. 177:149-154. 35 36 Burnley, M., Doust, J.H., Ball, D. and Jones, A.M. 2002. Effects of prior heavy exercise on VO(2) kinetics during heavy exercise are related to changes in muscle activity. J. Appl. Physiol. 93: 167-174. 37 38 Burnley, M., Doust, J.H., Carter, H. and Jones, A.M. 2001. Effects of prior exercise and recovery duration on oxygen uptake kinetics during heavy exercise in humans. Exp. Physiol. 86:417-425. 39 40 Burnley, M. and Jones, A.M. 2007. Oxygen uptake kinetics as a determinant of sports performance. Eur. J. Sport. Sci. 7:63-79. 41 42 43 Carter, H., Grice, Y., Dekerle, J., Brickley, G., Hammond, A.J. and Pringle, J.S. 2005. Effect of prior exercise above and below critical power on exercise to exhaustion. Med. Sci. Sports. Exerc. 37:775781. Barker, A.R., Welsman, J.R., Fulford, J., Welford, D. and Armstrong, N. 2008a. Muscle phosphocreatine kinetics in children and adults at the onset and offset of moderate-intensity exercise. J. Appl. Physiol. 105:446-456. Barstow, T.J, Jones, A.M., Nguyen, P.H. and Casaburi, R. 1996. Influence of muscle fiber type and pedal frequency on oxygen uptake kinetics of heavy exercise. J. Appl. Physiol. 81:1642-1650. Breese, B.C., Barker, A.R., Armstrong, N., Jones, A.M. and Williams, C.A. 2012. The effect of baseline metabolic rate on pulmonary O(2) uptake kinetics during very heavy intensity exercise in boys and men. Respir. Physiol. Neurobiol. 180:223-229. Breese, B.C., Williams, C.A., Barker, A.R., Welsman, J.R., Fawkner, S.G. and Armstrong, N. 2010. Longitudinal changes in the oxygen uptake kinetic response to heavy-intensity exercise in 14- to 16year-old boys. Pediatr. Exerc. Sci. 22:69-80. 23 1 2 3 4 5 6 Chidnok, W., Fulford, J., Bailey, S.J., Dimenna, F.J., Skiba, P.F., Vanhatalo, A. and Jones, A.M. 2013. Muscle metabolic determinants of exercise tolerance following exhaustion: relationship to the 'critical power'. J. Appl. Physiol. doi:japplphysiol.00334.2013. 7 8 9 10 11 12 13 14 15 16 17 De Roia, G., Pogliaghi, S., Adami, A., Papadopoulou, C. and Capelli, C. 2012. Effects of priming exercise on the speed of adjustment of muscle oxidative metabolism at the onset of moderate-intensity step transitions in older adults. Am. J. Physiol. Regul. Integr. Comp. Physiol. 302:R1158-1166. 18 19 20 21 22 23 24 Endo, M.Y., Kobayakawa, M., Kinugasa, R., Kuno, S., Akima, H., Rossiter, H.B., Miura, A. and Fukuba, Y. 2007. Thigh muscle activation distribution and pulmonary VO2 kinetics during moderate, heavy, and very heavy intensity cycling exercise in humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 293:R812-820. 25 26 Fawkner, S.G., Armstrong, N., Potter, C.R. and Welsman, J.R. 2002. Oxygen uptake kinetics in children and adults after the onset of moderate-intensity exercise. J. Sports. Sci. 20:319-326. 27 28 29 30 31 32 33 34 35 36 37 38 39 40 Ferguson, C., Whipp, B.J., Cathcart, A.J., Rossiter, H.B., Turner, A.P. and Ward, S.A. 2007. Effects of prior very-heavy intensity exercise on indices of aerobic function and high-intensity exercise tolerance. J. Appl. Physiol. 103:812-822. 41 42 Hogan, M.C., Richardson, R.S. and Haseler, L.J. 1999. Human muscle performance and PCr hydrolysis with varied inspired oxygen fractions: a 31P-MRS study. J. Appl. Physiol. 86:1367-1373. 43 44 Hopkins, W.G. 2007. A spreadsheet for deriving a confidence interval, mechanistic inference and clinical inference from a P-value. Sportscience. 11:16-20. 45 46 Hopkins, W.G., Marshall, S.W., Batterham, A.M. and Hanin, J. 2009. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports. Exerc. 41:3-13. Cohen, J. 1988. Statistical Power Analysis for the Behavioural Sciences. 2nd edn. Lawrence Erlbaum, Mahwah, NJ. DeLorey, D.S., Kowalchuk, J.M., Heenan, A.P., Dumanoir, G.R. and Paterson, D.H. 2007. Prior exercise speeds pulmonary O2 uptake kinetics by increases in both local muscle O2 availability and O2 utilization. J. Appl. Physiol. 103:771-778. DeLorey, D.S., Kowalchuk, J.M. and Paterson, D.H. 2003. Relationship between pulmonary O2 uptake kinetics and muscle deoxygenation during moderate-intensity exercise. J. Appl. Physiol. 95:113-120. Fawkner, S.G. and Armstrong, N. 2004. Longitudinal changes in the kinetic response to heavyintensity exercise in children. J. Appl. Physiol. 97:460-466. Gandra, P.G., Nogueira, L. and Hogan, M.C. 2012. Mitochondrial activation at the onset of contractions in isolated myofibres during successive contractile periods. J. Physiol. 590:3597-3609. Gurd, B.J., Peters, S.J., Heigenhauser, G.J., LeBlanc, P.J., Doherty, T.J., Paterson, D.H. and Kowalchuk, J.M. 2009. Prior heavy exercise elevates pyruvate dehydrogenase activity and muscle oxygenation and speeds O2 uptake kinetics during moderate exercise in older adults. Am. J. Physiol. Regul. Integr. Comp. Physiol. 297:R877-884. Hebestreit, H., Kriemler, S., Hughson, R.L. and Bar-Or, O. 1998. Kinetics of oxygen uptake at the onset of exercise in boys and men. J. Appl. Physiol. 85:1833-1841. 24 1 2 3 4 5 6 Jones, A.M., Fulford, J. and Wilkerson, D.P. 2008. Influence of prior exercise on muscle [phosphorylcreatine] and deoxygenation kinetics during high-intensity exercise in men. Exp. Physiol. 93:468-478. Jones, A.M., Grassi, B., Christensen, P.M., Krustrup, P., Bangsbo, J. and Poole, D.C. 2011. Slow component of VO2 kinetics: mechanistic bases and practical applications. Med. Sci. Sports. Exerc. 43:2046-2062. 7 8 9 Jones, A.M., Vanhatalo, A., Burnley, M., Morton, R.H. and Poole, D.C. 2010. Critical power: implications for determination of VO2max and exercise tolerance. Med. Sci. Sports. Exerc. 42:18761890. 10 11 12 Kindig, C.A., Howlett, R.A., Stary, C.M., Walsh, B. and Hogan, M.C. 2005. Effects of acute creatine kinase inhibition on metabolism and tension development in isolated single myocytes. J. Appl. Physiol. 98:541-549. 13 14 15 16 17 18 19 Koga, S., Kano, Y., Barstow, T.J., Ferreira, L.F., Ohmae, E., Sudo, M. and Poole, D.C. 2012. Kinetics of muscle deoxygenation and microvascular PO(2) during contractions in rat: comparison of optical spectroscopy and phosphorescence-quenching techniques. J. Appl. Physiol. 112:26-32. 20 21 22 23 24 25 Koga, S., Poole, D.C., Fukuoka, Y., Ferreira, L.F., Kondo, N., Ohmae, E. and Barstow, T.J. 2011. Methodological validation of the dynamic heterogeneity of muscle deoxygenation within the quadriceps during cycle exercise. Am. J. Physiol. Regul. Integr. Comp. Physiol. 301:R534-541. 26 27 28 29 30 31 32 Krustrup, P., Jones, A.M., Wilkerson, D.P., Calbet, J.A. and Bangsbo, J. 2009. Muscular and pulmonary O2 uptake kinetics during moderate- and high-intensity sub-maximal knee-extensor exercise in humans. J. Physiol. 587:1843-1856. 33 34 35 36 37 38 39 Layec, G., Bringard, A., Le Fur, Y., Vilmen, C., Micallef, J.P., Perrey, S., Cozzone, P.J. and Bendahan, D. 2009. Effects of a prior high-intensity knee-extension exercise on muscle recruitment and energy cost: a combined local and global investigation in humans. Exp. Physiol. 94:704-719. 40 41 Meyer, R.A. 1988. A linear model of muscle respiration explains monoexponential phosphocreatine changes. Am. J. Physiol. 254:C548-553. 42 43 44 45 Murias, J.M., Spencer, M.D., Delorey, D.S., Gurd, B.J., Kowalchuk, J.M. and Paterson, D.H. 2011a. Speeding of VO2 kinetics during moderate-intensity exercise subsequent to heavy-intensity exercise is associated with improved local O2 distribution. J. Appl. Physiol. 111:1410-1415. Koga, S., Poole, D.C., Ferreira, L.F., Whipp, B.J., Kondo, N., Saitoh, T., Ohmae, E. and Barstow, T.J. 2007. Spatial heterogeneity of quadriceps muscle deoxygenation kinetics during cycle exercise. J. Appl. Physiol. 103:2049-2056. Koppo, K. and Bouckaert, J. 2002. The decrease in VO(2) slow component induced by prior exercise does not affect the time to exhaustion. Int. J. Sports. Med. 23:262-267. Krustrup, P., Soderlund, K., Mohr, M. and Bangsbo, J. 2004. The slow component of oxygen uptake during intense, sub-maximal exercise in man is associated with additional fibre recruitment. Pflugers. Arch. 447:855-866. Leclair, E., Berthoin, S., Borel, B., Thevenet, D., Carter, H., Baquet, G. and Mucci, P. 2012. Faster pulmonary oxygen uptake kinetics in children vs adults due to enhancements in oxygen delivery and extraction. Scand. J. Med. Sci. Sports. doi:10.1111/j.1600-0838.2012.01446.x. 25 1 2 3 Murias, J.M., Spencer, M.D., Kowalchuk, J.M. and Paterson, D.H. 2011b. Muscle deoxygenation to VO(2) relationship differs in young subjects with varying tauVO(2). Eur. J. Appl. Physiol. 111:31073118. 4 5 Poole, D.C., Barstow, T.J., McDonough, P. and Jones, A.M. 2008. Control of oxygen uptake during exercise. Med. Sci. Sports. Exerc. 40:462-474. 6 7 8 Poole, D.C., Schaffartzik, W., Knight, D.R., Derion, T., Kennedy, B., Guy, H.J., Prediletto, R. and Wagner, P.D. 1991. Contribution of exercising legs to the slow component of oxygen uptake kinetics in humans. J. Appl. Physiol. 71:1245-1260. 9 10 Poole, D.C., Ward, S.A., Gardner, G.W. and Whipp, B.J. 1988. Metabolic and respiratory profile of the upper limit for prolonged exercise in man. Ergonomics. 31:1265-1279. 11 12 Ratel, S., Duche, P. and Williams, C.A. 2006. Muscle fatigue during high-intensity exercise in children. Sports. Med. 36:1031-1065. 13 14 15 Rossiter, H.B., Ward, S.A., Kowalchuk, J.M., Howe, F.A., Griffiths, J.R. and Whipp, B.J. 2002. Dynamic asymmetry of phosphocreatine concentration and O(2) uptake between the on- and offtransients of moderate- and high-intensity exercise in humans. J. Physiol. 541:991-1002. 16 17 18 19 20 21 22 Sahlin, K., Sorensen, J.B., Gladden, L.B., Rossiter, H.B. and Pedersen, P.K. 2005. Prior heavy exercise eliminates VO2 slow component and reduces efficiency during submaximal exercise in humans. J. Physiol. 564:765-773. 23 24 Springer, C., Barstow, T.J., Wasserman, K. and Cooper, D.M. 1991. Oxygen uptake and heart rate responses during hypoxic exercise in children and adults. Med. Sci. Sports. Exerc. 23:71-79. 25 26 27 28 29 30 31 32 33 34 35 36 Vanhatalo, A. and Jones, A.M. 2009. Influence of prior sprint exercise on the parameters of the 'allout critical power test' in men. Exp. Physiol. 94:255-263. 37 38 39 40 41 42 43 44 45 46 Scheuermann, B.W., Hoelting, B.D., Noble, M.L. and Barstow, T.J. 2001. The slow component of O(2) uptake is not accompanied by changes in muscle EMG during repeated bouts of heavy exercise in humans. J. Physiol. 531:245-256. Vanhatalo, A., Poole, D.C., Dimenna, F.J., Bailey, S.J. and Jones, A.M. 2011. Muscle fiber recruitment and the slow component of O2 uptake: constant work rate vs. all-out sprint exercise. Am. J. Physiol. Regul. Integr. Comp. Physiol. 300:R700-707. Wasserman, K., Hansen, J., Sue, D., Stringer, W. and Whipp, B. 2005. Principles of Exercise Testing and Interpretation. Including Pathophysiology and Clinical Application. 4th edn. Lippincott Williams & Wilkins, Philiadelphia. 26 1 2 Table 1. Oxygen uptake kinetics during bout 1 and bout 2 Variable 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Bout 1 Mean ± SD 0.74 ± 0.09 Bout 2 Mean ± SD 0.72 ± 0.10 Effect, 90% CL -0.02, ±0.04 Inference O Possibly lower Baseline V 2 (L·min-1) Phase II τ 25.5 ± 2.2 23.5 ± 6.4 -1.9, ±3.5 Unclear (s) Phase II TD 9.8 ± 2.9 9.3 ± 2.0 -0.5, ±1.7 Unclear (s) O amplitude 0.93 ± 0.34 1.04 ± 0.45 0.11, ±0.09 Possibly higher Phase II V 2 (L·min-1) Phase II gain 9.2 ± 0.9 10.1 ± 1.2 0.9, ±0.6 Very likely higher (mL·min-1·W-1) O slow component onset 159 ± 60 187 ± 40 29, ±36 Likely higher V 2 (s) O slow component 0.12 ± 0.10 0.05 ± 0.02 -0.08, ±0.07 Likely lower V 2 amplitude (L·min-1) O slow component relative 6.3 ± 3.4 2.8 ± 1.3 -3.5, ±2.6 Very likely lower V 2 amplitude (%) O 1.80 ± 0.49 1.81 ± 0.50 0.01, ± 0.04 Trivial End-exercise V 2 -1 (L·min ) O gain 10.3 ± 1.0 10.6 ± 1.3 0.3, ±0.3 Possibly higher End-exercise V 2 (mL·min-1·W-1) O mean response time 45.1 ± 7.4 37.1 ± 5.4 -8.0, ±3.0 Most likely faster V 2 (s) Effect, represents the magnitude of the change by subtracting bout 2 from bout 1. 90% CL, represents the uncertainty of the observed effect. The 90% CL of the true effect can be established by adding and subtracting the 90% CL to the effect. Inference, represents the probabilistic inference that the magnitude of the observed effect is different from the smallest worthwhile change using Cohen’s standardized effect of 0.2 (see methods for details). 27 1 2 Table 2. Muscle oxygenation kinetics during bout 1 and bout 2 cycling conditions Variable 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 Bout 1 Mean ± SD -4.6 ± 2.8 Bout 2 Mean ± SD -6.9 ± 3.5 Effect, ±90% CL -2.2, ±0.9 Inference HHb baseline Very likely lower (a.u.) HHb primary TD 9.0 ± 2.8 6.2 ± 2.1 -2.8, ±1.6 Very likely lower (s) HHb primary τ 14.7 ± 6.1 15.0 ± 3.1 0.2, ±3.9 Unclear (s) HHb primary MRT 23.7 ± 6.1 21.2 ± 3.7 -2.6, ±3.9 Unclear (s) HHb primary amplitude 7.0 ± 2.9 8.1 ± 3.3 1.1, ±0.9 Likely higher (a.u.) HHb slow component 1.2 ± 1.6 1.3 ± 0.5 0.1, ±1.1 Unclear amplitude (a.u.) HHb slow component 9.0 ± 16.6 14.8 ± 7.2 5.9, ±15.7 Unclear amplitude (%) HHb at 6 min 3.6 ± 3.7 2.6 ± 3.6 -1.0, ±0.9 Possibly lower (a.u.) O baseline -6.07 ± 3.23 -9.23 ± 4.11 -3.16, ±1.24 Very likely lower HHb/ V 2 (a.u./ L·min-1) O primary 1.47 ± 1.57 0.75 ± 2.19 -0.72, ±0.58 Likely lower HHb/ V 2 (a.u./ L·min-1) O at 6 min 2.06 ± 1.95 1.36 ± 2.24 -0.70, ±0.47 Likely lower HHb/ V 2 (a.u./ L·min-1) Effect, represents the magnitude of the change by subtracting bout 2 from bout 1. 90% CL, represents the uncertainty of the observed effect. The 90% CL of the true effect can be established by adding and subtracting the 90% CL to the effect. Inference, represents the probabilistic inference that the magnitude of the observed effect is different from the smallest worthwhile change using Cohen’s standardized effect of 0.2 (see methods for details). 28 1 FIGURE CAPTIONS 2 O profile during bout 1 (○) and bout 2 (●). The onset of exercise is illustrated by Figure 1. Mean V 2 3 O amplitude and the reduced V O slow the vertical dotted line. Note the increased phase II V 2 2 4 component amplitude in bout 2. 5 6 Figure 2. Mean HHb (A) and TOI (B) dynamics during bout 1 (○) and bout 2 (●). The vertical dotted 7 line signifies the onset of exercise. Note that in bout 2 the TOI is elevated at baseline and throughout 8 the exercise transition. 9 10 Figure 3. The relationship between the change in tissue oxidation index (TOI) from baseline to 6 min 11 O amplitudes of exercise in bout 2 to the change in the phase II (A) and slow component (B) V 2 12 following priming exercise. 13 14 O (●) dynamics during bout 1 (A) and bout 2 (B). Figure 4. Group mean normalised HHb (○) and V 2 15 O ) for bout 1 (□) and bout 2 (■). Note that a Panel C expresses these changes as a ratio (ΔHHb/Δ V 2 16 O ‘overshoot’ is present in bout 1, but this is abolished to an ‘undershoot’ in bout 2. ΔHHb/Δ V 2 17 18 Figure 5. Mean iEMG during bout 1 (○) and bout 2 (●). The vertical dotted line signifies the onset of 19 exercise. 20 21 22