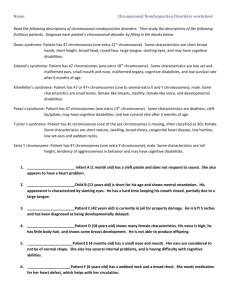
genome chromosomal
advertisement

MS-1 FUND 1: 9:00-10:00 Monday, September 10, 2014 Dr. Nathaniel Robin Chromosome Structure II Transcriber: Alex Paulsen Editor: Hannah Turner Page 1 of 5 Abbreviations: aCGH = array Comparative Genome Hybridization Introductory Comments: This is the second hour of Dr. Robin’s lecture on chromosome structure. Note: timestamps are based on the ECHO recording. I. Clarification of ARS question from previous lecture 03:50 a. Explanation of Robertsonian translocation in response to confusion over ARS question b. Dr. Robin used chalkboard drawings to demonstrate abnormal and normal chromosomes i. In a Robertsonian translocation, all of the necessary genetic information is present, even though in this case only 45 chromosomes are present. ii. Involves acrocentric chromosomes iii. Other answer choice is phenotypically abnormal. Why? 1. One parent could have had balanced 12-16 rearrangement 2. Many other possibilities- could have been error in crossing over iv. Nondisjunction events are the most common genetic abnormality in humans v. Major translocation events are right behind nondisjunctions in frequency (SN: Please see ECHO for his full explanation. It makes much more sense in context with the ARS question (which cannot be transcribed) that is displayed in the recording) II. Chromosomal abnormalities (slide 19) 06:05 a. There are different types of chromosome abnormalities b. Constitutional chromosome abnormalities, or germ line abnormalities, are present in every cell in the body i. Called germ line because at moment of conception, were present in the egg or sperm that formed the child c. Acquired abnormalities (aka somatic events) are present in only a certain number of cells, typically derived from certain tissues i. The genetic abnormality occurred post-conception ii. Ex: One of 64th cells could have a mitotic nondisjunction event 1. Then, all the cells that came from that 64th cell would have that mitotic nondisjunction event, having an extra chromosome 2. Might be significant or might not be 3. Could also be true for a chromosomal rearrangement or single gene mutation 4. This is a common mechanism of cancers (esp. blood type cancers) d. Different types of chromosomal aneuploidy i. Example on slide: Numerical (47, XX, +13) 1. Aneuploidy means not the right number of chromosomes; not diploid a. Could be zero, one, three, four, etc. number of chromosomes when there should be two 2. Numeric aneuploidies a. Ex: extra copy of chromosome 13 3. Question: what [autosomal] chromosome has the least amount of genes on it? a. Answer: Chromosome 21 b. Chromosome 18 is second most common trisomy c. Chromosome 13 is third most common trisomy d. Chromosome 16: won’t see a live birth with this trisomy 4. Chromosome 22 is very gene rich (during fellowship he worked across the hall from 22 Genome Project; he is a big fan of this chromosome) e. Structural abnormalities i. Amount of genetic information is not right, but the number is correct ii. Right number of centromeres, but chromosomes are arranged in a way that is not normal iii. Example on slide: Structural (46, XY [del5p13]) 1. 46 chromosomes, X and Y because it is a boy, deletion of 5p13 and everything beyond p13 to the tip 2. Segmental or structural chromosomal aneuploidy III. Numeric abnormalities (slide 20) 09:46 a. Polyploidy i. Never would see a haploid conceptus ii. Could see triploid conceptuses, where there are 3n DNA instead of 2n DNA (very abnormal) iii. Tetraploid would not come close to being anything normal and viable; more likely to see this sort of thing in tumors b. Aneuploid – an extra or missing individual chromosome (47, XX, +18) c. Mixoploidy i. There is mosaicism – means not all the cells in the body are genetically identical ii. You could be mosaic at the single gene level (half your cells have mutation in a certain gene, half your cells do not) or you could be mixoploid for a structural abnormality MS-1 FUND 1: 9:00-10:00 Monday, September 10, 2014 Dr. Nathaniel Robin Chromosome Structure II Transcriber: Alex Paulsen Editor: Hannah Turner Page 2 of 5 Abbreviations: aCGH = array Comparative Genome Hybridization 1. Remember Trisomy 16 is never viable, although it is the most common nondisjunction chromosome a. The only viable trisomies are 13, 18 (marginally) and 21 b. With a number of other chromosomes, you could see if it is mosaic at a very low level c. Trisomy 12: you wouldn’t see it in every cell in the body, but in a small number of cells i. Children are severely abnormal, lots of birth defects, significant intellectual disabilities ii. Only have extra copy of chromosome 12 in a few cells IV. Karyotype from inviable pregnancy (slide 21) 11:34 a. 69XXX, not associated with a viable pregnancy <ARS 12:04-12:54> V. Structural abnormalities (segmental aneuploidy) (slide 22) 12:55 a. Two types of deletions: i. Cytogenetically visible 1. Cytogenetically visible deletions mean that you are missing 5-10 million base pairs of DNA at a minimum (that’s a boatload) ii. Microscopically visible (microdeletions) that require additional tests b. Duplication – small segment of DNA is duplicated i. Much more difficult to detect via conventional methods; need more advanced methods that we will talk about later c. Insertion – segment of DNA breaks off and is inserted i. Do not get hung up on why/how this occurs d. Translocation – can be balanced or unbalanced e. Inversions – a segment of genetic information is flipped i. Alleles ABCDE flipped to EDCBA ii. This is deleterious when crossing over occurs in that segment 1. Can lead to deletions and duplications iii. Don’t need to know details; know that consequence of inversion in individual causes no problems; risk is a reproductive risk (segmental aneuploidy in offspring following crossing over event) iv. Inversions that do not involve the centromere are more benign 1. Chromosomes with none or two centromeres are not viable; nonviable offspring; miscarriage likely (more benign than alternative – imbalances in offspring with inversions involving centromere) f. Isochromosome i. Have a duplication of a long arm on itself ii. Example: Chromosome 21 : isochromosome 21 would be 21q and 21q and no 21p iii. This would be abnormal; something you can see with Down’s syndrome g. Ring chromosome i. Remember, telomeres are important because they cap the chromosomes (like tips of shoelaces) ii. If telomere is lost or abnormal, chromosomes can bend back and fuse on themselves in a ring chromosome iii. Rings tend to be very unstable, and when they break you lose meaningful genetic information iv. Remember, subtelomeric region is relatively gene rich, so a ring chromosome means there has likely been a deletion of genetic information that contained important genes in that subtelomeric region VI. Translocation diagram (slide 23) 17:22 a. Balanced rearrangement (20 and 4 swap information) b. Risk is for unbalanced version in offspring <ARS 17:40-19:03> VII. Robertsonian translocations (slide 24) 19:04 a. Involve acrocentric chromosomes (13,14,15,21,22) b. Total number of chromosomes is reduced in healthy carriers c. Carrier rate is not trivial: 1 in 500 individuals are carriers for Robertsonian translocation i. It presents itself with infertility or abnormal birth d. Three “flavors” of Down Syndrome i. 1.5% are mosaic or translocation of abnormal chromosome compliment involving 21 ii. 94.5% are free standing 21’s iii. 3.5% involve a translocation that is typically a Robertsonian translocation iv. Example: baby with Down’s syndrome 1. Mom is 39 years old 2. If karyotype shows that baby has 46 chromosomes, and a 14-21 translocation causing the extra 21, then it was not related to mom’s advanced age a. This kind of scenario will likely show up on test VIII. Karyotype example (slide 25) 20:32 a. 13-14 balanced Robertsonian (“super chromosome”) MS-1 FUND 1: 9:00-10:00 Monday, September 10, 2014 Dr. Nathaniel Robin Chromosome Structure II Transcriber: Alex Paulsen Editor: Hannah Turner Page 3 of 5 Abbreviations: aCGH = array Comparative Genome Hybridization b. Bigger chromosome dominates the meiosis picture, in general IX. Reproductive risks for Robertsonian translocation carriers (slide 26) 20:54 a. Monosomy i. All incompatible with liveborn ii. Infertility, recurrent spontaneous loss b. Trisomy i. 14, 15, 22 are incompatible with life ii. 13, 21: well known, abnormal conditions and abnormal newborns iii. 15: big risk is imprinting disorders; we will talk about this in more detail in future class X. Carrier cartoon (slide 27) 21:27 a. Dr. Robin said is basically the same thing we just talked about in a cartoon XI. Reproductive risk examples (slide 28) 21:31 a. 45,XX, der(14;21)(q10;q10) i. Females – risks are 8, 10-12% for an abnormal live born ii. Note: nowadays, can go to a website and get empiric number risk via a calculator for a particular balanced rearrangement b. 45,XY, der(14;21)(q10;q10) i. Risk for male with 14-21 is very low (1%) ii. Risk when males carry balanced rearrangement is exceptionally low, never over 1-2% c. 45,XY, der(21;21)(q10;q10) i. Risk for male with 21-21 (which is very rare) ii. Risk would be 100% for Down’s syndrome iii. Negligible chance of having a healthy newborn d. 45,XX, der(14;14)(q10;q10) i. Essentially zero risk 1. Almost no chance of having a child at all 2. That child would not be normal 3. 14 is an imprinted chromosome; the genetic information on 14 is differentially expressed depending on whether it comes from mom or dad (will talk more about in a later class) XII. Cytogenetic testing (slide 29) 23:08 a. Looking at chromosomes; very old school but still done b. Relatively cheap in the context of medical tests: $600 (bargain) c. Detection rate depends on who you’re studying; ~2% i. Woman with 3+ miscarriages, 3-5% chance that you’ll find the translocation ii. Child with intellectual disability and birth defects, slightly higher chance that you’ll find the chromosomal abnormality iii. Child comes in looking like they have trisomy 13, pretty darn likely you’ll find the chromosomal abnormality XIII. FISH for 22q11 deletion (DiGeorge probe) image (slide 30) 24:02 a. Chromosome analysis is really good because you don’t need to know what you’re looking for b. Example: baby in clinic i. You may think baby has Down’s syndrome, Dr. Robin says doesn’t look like Down’s syndrome, chromosome analysis shows that kid has Wolf-Hirschhorn Syndrome (missing piece of chromosome 4) 1. Main point: doesn’t matter if you don’t know what you’re doing – chromosome analysis is a screening test ii. Downside of chromosome analysis: need 5-10 million basepairs minimum missing or extra to be detected iii. Only need one base pair messed up to cause serious genetic problems iv. FISH testing was done to look for missing pieces that are too small to be visible via microscopy c. DiGeorge syndrome (Velocardiofacial Syndrome or now known as 22q1 deletion syndrome) - the most common sub-microscopic chromosome abnormality known (1 in 2,000 to 1 in 4,000 children born with this) i. Tiny piece of chromosome 22 is missing ii. Researchers identified it and developed a probe to look for it 1. Probe has a fluorescent dye 2. Stick probe onto patient’s chromosomes a. If you get two signals for each sister chromatid, it is intact i. In this case, can see two red signals indicating that region of chromosome 22 ii. Green signals tell you it is chromosome 22 1. With FISH testing, hard to tell the different chromosomes apart iii. Red signals are disease probes MS-1 FUND 1: 9:00-10:00 Monday, September 10, 2014 Dr. Nathaniel Robin Chromosome Structure II Transcriber: Alex Paulsen Editor: Hannah Turner Page 4 of 5 Abbreviations: aCGH = array Comparative Genome Hybridization 1. In image, can see that red signal is not lighting up, nothing for it to bind to, therefore it is missing and this patient has a deletion so has diGeorge syndrome. (SN: Dr. Robin points out nomenclature for this (listed on slide): 46,XY, ish del(22)(q11.2q11.2)(TUPLE1-)) XIV. Contiguous gene syndrome (genetic ladder) (slide 31) 26:41 a. Will talk more about this later b. Some genetic conditions have multiple genes missing, and phenotype you see can be attributable and characterized by extent of deletion i. Trichorhinophalangeal syndrome 1. Tricho – sparse, abnormal hair 2. Rhino – very characteristic nose 3. Phalangeal – particular finger abnormalities 4. Autosomal dominant condition caused by a single gene mutation on chromosome 8 ii. Type II Trichorhinophalangeal syndrome 1. Phenotype (physical appearance) of type I; additionally have intellectual disabilities and multiple exostoses (tumors on the bone) c. Trichorhinophalangeal syndrome type II caused by a deletion of chromosome 8 that includes the trichorhinophalangeal gene and the neighboring genes that are involved in intellectual disability and in the bone growth, and their absence causes multiple exostoses d. Each step on the ladder can be attributed to particular characteristic of your patient XV. Neurofibromatosis (slide 32) 28:13 a. Another example is Type 1 neurofibromatosis b. Common disorder, and we are one of the leading centers in the world (his boss is world expert) c. Condition caused by a mutation on neurofibromin gene on chromosome 17q11 i. (From slide) Most cases are caused by point mutations in the NF1 gene. These are not visible by routine chromosome study, but are detectable by FISH. ii. Small number of affected people have intellectual disability 1. Many of these patients have, not a point mutation in NF1 gene, but a segment of chromosome 17 missing <ARS 29:01-29:41> XVI. Limitations of FISH analysis (slide 33) 29:42 a. FISH is great but unlike chromosome analysis, with FISH you need to know something b. Clinic example revisited i. You think it is 22q11 deletion syndrome in clinic, but Dr. Robin says it is Prader-Willi syndrome deletion. So the FISH test you order for 22q11 probe might be the best FISH test in the world for that deletion, but since the child didn’t have that it would not have mattered. You have to know what you are looking for. XVII. Subtelomere studies (slide 34) 30:22 a. Subtelomere assay was a baby step to improve on this b. They look at all the subtelomeric regions at once using FISH studies c. This improved detection rate dramatically of undiagnosed cases of intellectual disability or multiple birth defects XVIII. Array Comparative Genome Hybridization (CGH) (slide 35) 30:43 a. Subtelomere assay was a baby step to where we are today b. Next step up in cytogenetic testing is array CGH: an incredibly powerful test that looks for copy number variation i. Not looking at small segments of DNA (10s of thousands of base pairs) in the right number of segments c. We have a tremendous amount of variability in not just certain letters of our genetic information but whole segments of our genetic information – tiny segments we can’t see under a microscope but this test can show us i. Many of these segments associated with disease d. Picture a FISH test (for DiGeorge syndrome, was one probe looking for one specific region of DNA) i. Array CGH uses same technology plus or minus, but using 64,000 probes spanning genome ii. The technology is very simple 1. Take a control DNA (notice not a “normal DNA”- doesn’t exist) and patient’s DNA 2. Label control DNA red and patient DNA green, put them together 3. Run a scanner over it; should see yellow (means equal amounts of red and green) a. If scanner sees red, there is too much control DNA compared to patient, means that patient has a deletion b. If scanner sees green, too much patient DNA relative to control, so patient has a duplication <ARS 33:39-35:13> XIX. Array CGH in clinical testing (slide 36) 35:14 a. Benefits: way more sensitive, way better to detect things b. Takes about two months to come back, so not really that fast of a turnaround time MS-1 FUND 1: 9:00-10:00 Monday, September 10, 2014 Dr. Nathaniel Robin Chromosome Structure II Transcriber: Alex Paulsen Editor: Hannah Turner Page 5 of 5 Abbreviations: aCGH = array Comparative Genome Hybridization c. Requires DNA, not living cells (compared to chromosomes, where you need live cells) d. Two limitations that are major: i. More expensive (although in the context of medical tests, couple thousand dollars is still a bargain) ii. Variance of uncertain significance 1. We often detect variations that we do not know clinical significance of 2. Karyotype with extra copy of chromosome 21: Dr. Robin can tell you what it means, prognosis, management a. However, many rearrangements that the array will detect, we have no idea if they are clinically significant or not b. Furthermore, most common way to figure that out is to test parents (if healthy parent has same rearrangement as child has, determine it is benign variant) c. However, with array level abnormalities, many of them may cause no problems in one person and lots of problems in another person (no idea why) 3. These things are difficult to explain to patients; complicated process XX. Example of array CGH output (slide 37) 37:17 a. Said he would not ask us about this; 32K versus newest ones are 64K (old technology) XXI. CGH array read out (slide 38) 37:29 a. What CGH array looks like when it is read out b. Scatter around zero, can see two darker areas c. Ignore random scattering d. Look for a number in the same area that are signaling missing or extra information i. At the tip of chromosome 4, can see a deletion, missing markers (SN: see slide) ii. Chromosome 11 - duplication XXII. Molecular ladder, continued (slide 39) 38:19 a. Now we know the probes that were used, and thanks to the Human Genome Project we know what genes were on those probes b. On genetic level, now we can say specifically which genes you are missing/have extra of and what that will cause c. Now we know which exact genes are missing or extra and their functions, and so can predict clinical consequences d. Array CGH: Xp11.4 deletion on previous slide i. Patient has ornithine transcarbamylase (OTC) deficiency 1. Not presenting with typical X-linked form, but a much less common version of it due to missing chromosomal piece XXIII. aCGH vs. cytogenetics vs. FISH (slide 40) 39:31 a. Summarizes big picture differences between these tests (SN: He skipped over this slide; I have included bullet points below) i. aCGH 1. (+) Do NOT need clinical suspicion; increased detection; much more detailed; does NOT need dividing cells 2. (-) Expensive and slow; does not detect balanced rearrangements ii. Cytogenetics 1. (+) Do NOT need clinical suspicion; cheaper and faster; will detect balanced rearrangements 2. (-) Relatively poor detection rate; need dividing cells iii. FISH 1. (+) Diagnostic test – need clinical suspicion No student questions. <END OF LECTURE 42:39>