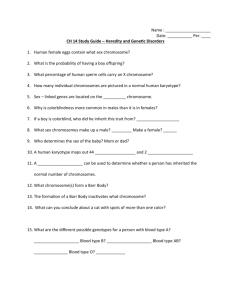
Genetics Ch. 6 [4-20
advertisement

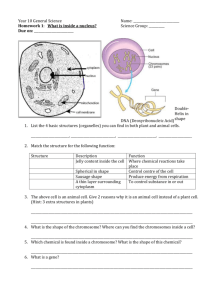
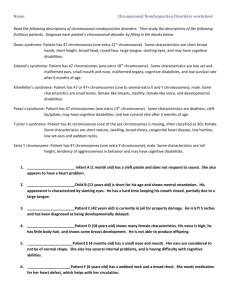
Genetics Ch. 6 Clinical Cytogenesis: The Chromosomal Basis of Human Disease Cytogenetics – study of chromosomes and their abnormalities Chromosome abnormalities – responsible for a significant fraction of genetic diseases (1 of every 150 live births); leading cause of mental retardation and pregnancy loss Karyotype (karyogram) – ordered display of chromosomes according to length Normal female karyotype: 46, XX Normal male karyotype: 46, XY Chromosomes classified by size and position of centromere - Metacentric – centromere occurs near midline of chromosome - Acrocentric – centromere near the tip - Submetacentric – centromere between the middle and the tip Telomere – tip of each chromosome p – short arm of each chromosome (petite) q – long arm of each chromosome Chromosome banding – helps greatly in detection of deletions, duplications, structural abnormalities, helps to identify individual chromosomes - Includes quinacrine, Geimsa, reverse, C and NOR banding Fluorescence in situ Hybridization (FISH) – labeled probe is hybridized to metaphase, prophase, or interphase chromosomes - Can be used to test for missing/additional chromosome material and chromosome rearrangements - Probe undergoes complementary base pairing only with the complementary base DNA sequence at a specific location on one of denatured chromosomes - Normal Patient: probe hybridizes in 2 places, reflecting the presence of 2 homologous chromosomes in somatic cell nucleus - Not Normal Patient: hybridizes to only one of the patients chromosomes indicates deletion on copy of chromosome to which probe fails to hybridize Comparative Genomic Hybridization (CGH) – differentially labeled DNA from test and control sources is hybridized to normal metaphase chromosomes or probes in microarrays, allows the detection of chromosome duplications and deletions, but not balanced rearrangements. - Array CGH can detect deletions/duplications shorter than 100kb and requires only small amounts of DNA Abnormalities of Chromosome Number Polyploidy o Presence of a complete set of extra chromosomes in a cell o Polyploidy conditions that have been observed in humans: Triploidy (69 chromosomes in nucleus of each cell) Estimated 15% chromosome abnormalities Common causes: fertilization of an egg by 2 sperm (dispermy), or meiotic failure (diploid sperm or egg is produced) Tetraploidy (92 chromosomes in each cell nucleus) Much rarer Common causes: mitotic failure (all of the duplicated chromosomes migrate to one of the 2 daughter cells), or from fusion of 2 diploid zygotes Because the number of chromosomes present in each of these conditions is a multiple of 23, the cells are euploid (Greek – “good set”), however surplus gene product causes multiple anomolies such as defects of heart and CNS Autosomal Aneuploidy o Cells that contain additional or missing individual chromosomes (not a multiple of 23) o Usually only one chromosome is affected o Common cause: nondisjunction (failure of chromosomes to disjoin normally during meiosis) o Most clinically important of chromosome abnormalities o Monosomy – only one copy of a chromosome in an otherwise diploid cell o Trisomy – three copies of a chromosome; produce less severe consequences than monosomies – proves the body can tolerate excess genetic material more readily than it can tolerate a deficit of genetic material Trisomy 21 Karyotype: 47, XY, +21 or 47, XX, +21 Low nasal root, palpebral fissures, small overfolded ears, flattened maxillary region, short neck, broad/short hands, deep flexion crease across palms (“Simian crease”), decreased muscle tone Increased frequency of medical problems: obstruction of duodenum or atresia, respiratory infections, structural heart defects, mental retardation 95% cases caused by nondisjunction Extra chromosome donated by mother in 90-95% cases Mosaicism – seen in 2-4% (have some normal somatic cells, some trisomy 21 cell), milder clinical expression of the phenotype There is a maternal age effect (risk increases to 1/400 at age 35, 1/100 at age 40, 1/25 at age 45); mother contributes the extra chromosome in 90% of cases Trisomy 18 Karyotype: 47, XY, +18, also known as Edwards syndrome Second most common autosomal trisomy Small ears, small mouth, short sternum, short halluces, congential heart defects, diaphragmatic hernia, radial aplasia 95% have complete trisomy 18, only a small percentage have mosaicism 90% of cases result of extra chromosome of mother Trisomy 13 Karyotype: 47, XY, +13, also termed Patau syndrome Oral-facial clefts, microphthalmia (small abnormally formed eyes), malformations of CNS, significant mental retardation 80% have full trisomy 13 Most are spontaneously lost during pregnancy Sex Chromosome Aneuploidy o Primarily due to X inactivation o Less severe than those of autosomal aneuploidy Monosomy of X Chromosome (Turner Syndrome) Karyotype: (50%) 45, X, (30-40%) mosaicism 45, X / 46, XX, and less commonly 45, X / 46, XY Short stature, sexual infantilism, triangle shaped face, posteriorly rotated ears, broad “webbed” neck, congenital heart defects, structural kidney defects, most lack ovaries and do not develop secondary sexual characteristics 60-80% derived from absence of paternally derived sex chromosome Specific gene involved: SHOX gene Klinefelter Syndrome Karyotype: 47, XXY Patients are taller than average, disproportionately long arms and legs, small testes, low testosterone levels, gynecomastia, sparse body hair, predisposition for learning disabilities Extra X chromosome derived maternally in about 50% of Klinefelter cases, increases in advanced maternal age, mosaicism seen in 15% cases Degree of mental deficiency / physical abnormality increases with each additional X chromosome Trisomy X Karyotype: 47, XXX Females suffer from sterility, menstrual irregularity, mild mental retardation 90% cases due to nondisjunction in mother, incidence increases in older mothers 47, XYY Syndrome Karyotype: 47, XYY Males tend to be taller than average, reduced IQ, redisposition to violent criminal behavior Chromosome Abnormalities and Pregnancy Lost - 1/3 of pregnancies lost after implantation - Chromosome abnormalites leading cause of pregnancy loss - 50% chromosome abnormalities = trisomies; 20% = monosomies, 15% = triploids; remainder tetraploids / structural abnormalities Abnormalities of Chromosome Structure - Unbalanced rearrangement causes a gain or loss of chromosome material - Balanced rearrangement does not produce a loss or gain of chromosome material - Translocations – interchange of genetic material between nonhomologous chromosomes, 2 basic types: o Reciprocal translocations – caused by 2 breaks on different chromosomes, subsequent exchange of material o Robertsonian translocations – occur when the long arms of 2 acrocentric chromosomes fuse at the centromere; carrier can produce conceptions with monosomy or trisomy of the long arms of acrocentric chromosomes Common example – chromosomes 14 and 21 - Deletions – caused by a chromosome break, subsequent loss of genetic material o Example: Cri-du-chat syndrome – deletion of distal short arm of chromosome 5 o Example: Wolf-Hirschhorn syndrome – deletion of distal short arm of chromosome 4 - Microdeletion Syndromes o Example: Prader-Willi syndrome due to imprinting, inheritance of a microdeletion of the paternal chromosome 15 material produces Prader-Willi syndrome; microdeletion of the maternally derived chromosome 15 produces Angelman’s syndrome - Subtelomeric Rearrangements – involve deletions or duplication of DNA in the gene-rich regions near telomeres - Uniparental Disomy – a condition in which one parent has contributed 2 copies of a chromosome, and the other parent has contributed no copies - Duplications – arise from unequal crossover, or they can occur among the offspring of reciprocal translocation carriers; produce less serious consequences than do deletions of the same region - Ring chromosomes – when deletions occur at both tips of a chromosome, chromosome ends can then fuse, form a ring - Inversions – result of 2 breaks on a chromosome followed by reinsertion of the intervening fragment at its original site, but in inverted order - Isochromosomes – chromosome that has 2 copies of one arm but no copies of the other Chromosome abnormalities and Clinical Phenotypes Most chromosome abnormalities are associated with developmental delay in children and mental retardation in older persons reflects large number of genes involved in CNS development Most chromosome syndromes involve alterations of facial morophogenesis patient resembles other patients with same disorder Growth delay seen in autosomal syndromes Congenital malformations occur with increased frequency in most autosomal chromosome disorders Cancer Cytogenetics - Chronic Myelogenous Leukemia (CML) – caused by reciprocal translocation between chromosome 22 and the long arm of chromosome 9 (Philadelphia chromsome) o Proto-oncogene ABL moved from normal position on 9q to 22q o Alters ABL gene product, causes increased tyrosine kinase activity leads to malignancy in hematopoietic cells - Burkitt Lymphoma – reciprocal translocation involving chromosomes 8 and 14, moves the MYC proto-oncogene from 8q24 to 14q32 Clinical Commentaries 1. Health Supervision in Children with Down Syndrome a. Most common congenital heart defect: AV canals, surgical correction appropriate before 1 year b. Strabismus = deviation of eye from normal visual axis and other eye problems should be examined by physician regularly c. Hypothyroidism is common thyroid levels measured regularly d. Sensorineural and conductive hearning loss routine hearing tests e. Instability of 1st and 2nd vertebrae can lead to spinal cord injuries f. Referral to preschool programs to provide intervention for developmental disabilities 2. Genetic Basis of Sex Determination a. SRY = sex determining region on the Y b. By bending DNA, protein is thought to promote DNA-DNA interactions; this trigger events leaving to male differentiation; also protein of SRY acts antagonistically with DAX1 (which represses differentiation into male) c. In absence of SRY, DAX1 continues to repress these genes, female embryo is created 3. DiGeorge Sequence, Velocardiofacial Syndrome, and Microdeletions of Chromosome 22 - DiGeorge sequence – characterized by structural or functional defects of thymus, conotruncal heart defects, hypoparathyroidism, and secondary hypocalcemia - Children with this sequence were found to have deletion of long arm of chromosome 22 - Velocardiofacial Syndrome (VCF) – palatal abnormalities, characteristic facial appearance, heart malformations, learning disabilites - Some persons with VCF have all features of DiGeorge sequence - Suggests the two are related, caused by abnormalities on chromosome 22