incidence, clinical features and treatment
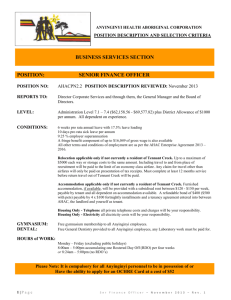
advertisement

Atypical Hyperadrenocorticism: incidence, clinical features and treatment Steve Marsden DVM ND MSOM Lac Dipl.CH CVA AHG Atypical Hyperadrenocorticism (AHAC) Hyperadrenocorticism (pituitary dependent hyperadrenocorticism, PDH, Cushing's disease) arises from benign functional tumors of the pituitary gland that result in hypersecretion of cortisol from the adrenal glands. The clinical presentation of PDH is highly similar between dogs and humans. Characteristic signs for both include abdominal obesity, weight gain, fatigue, muscle atrophy and skin changes. The incidence of pituitary tumors in humans is rare, yet in dogs the rate of incidence is accepted as 1 or 2 cases per 1,000 dogs per year (de Bruin et al, 2009). By comparison, a rule of thumb estimate of the overall rate of cancer incidence in dogs suggests it occurs at about the same rate as humans - 400 cases per 100,000 people per year, or 4 cases per thousand per year. The incidence of Cushing’s disease in dogs is thus potentially as high as half of all other cancer cases combined. Such a high rate of incidence should prompt us to wonder if the disease is being over-diagnosed; but if so, what is the true diagnosis of the dog with apparent PDH? While Cushing’s is rare in humans, hypercortisolism is abundant.. Hypercortisolism is a state of cortisol hypersecretion, hyper-responsiveness to cortisol, or both. The condition produces characteristic signs of Cushing’s disease, to the point of being almost clinically indistinguishable, yet is not at all due to a pituitary tumor. Recent research suggests many dogs diagnosed as having Cushing’s may in fact have hypercortisolism, otherwise known as atypical hyperadrenocorticism (AHAC). Diagnosis of AHAC ACAH is diagnosed in a dog that appears to have Cushing’s disease, yet tests negative for the condition using definitive laboratory testing such as ACTH stimulation and low dose dexamethasone suppression tests. Some authors have speculated the clinical signs are stemming for an over-production of sex steroids, which others have contested. Recent research suggests AHAC dogs do indeed over-produce cortisol, and have bilaterally enlarged adrenal glands (Frank et al, 2015), making differentiation from from Cushing’s disease a potential challenge. Many AHAC cases eventually go on to finally being diagnosed as having Cushing’s disease, leading some authors to suggest AHAC is a precursor state to eventual pituitary adenoma. It is also possible, however, that chance fluctuations in cortisol levels in AHAC patients will simply cross the threshold at which a diagnosis of PDH is rendered, for seldom is the presence of an actual pituitary tumor confirmed in PDH dogs. While overall hourly cortisol and total cortisol secretion in dogs with confirmed pituitary adenomas is higher than in AHAC dogs, there is considerable overlap, with AHAC dogs at times secreting more cortisol than PDH dogs. There was also a trend for adrenal gland size in AHAC dogs to actually be larger than in dogs with PDH (Frank et al, 2015). It is thus easily conceivable that an AHAC patient may be diagnosed as having PDH. Diagnosis of AHAC vs. PDH may one day be easier once more is known about the pharmacodynamics and pharmacokinetics of cortisol in hypercortisolism/AHAC. Unfortunately, after a decade of research, it is still apparently unclear how cortisol metabolism is altered in hypercortisolism. Research suggests changes include any or all of (Björntorp and Rosmond, 2000; Pasquali and Vicennati, 2000): Hyper-responsiveness of the hypothalamic-pituitary-adrenal axis Heightened clearance of cortisol Altered or more frequent patterns of secretion This HPA hyper-responsiveness would theoretically allow AHAC patients to theoretically test false positive for PDH in stimulation tests. In addition, increased abdominal fat reserves can increase serum cortisol. They contain type 1 11beta-hydroxysteroid dehydrogenase, which converts cortisone to cortisol. Previous publications have dismissed any notion of a diagnostic challenge in differentiating AHAC and PDH. Definitive tests for Cushing’s are reported as normal in AHAC dogs (Behrend and Kennis, 2010). The recently discovered similarities, even overlap, in cortisol secretion between PDH and AHAC suggest, however, that this statement may be presumptive. The dexamethasone suppression test was recently proven inadequate for distinguishing AHAC from Cushing’s in humans, despite the literature asserting otherwise (Lindholm, 2014). As early as 1997, the dexamethasone suppression test in dogs was shown to be only 70% specific for Cushing’s (Van Liew et al, 1997). False positives for the ACTH and dexamethasone suppression tests do exist, and in the case of the suppression test are even commonplace, making confirmation of a pituitary tumor through medical imaging ideal, although impractical (Peterson, 2007). AHAC and Insulin Resistance While metabolism of cortisol in AHAC is as yet unclear, the cause appears to be more defined. Insulin resistance appears to play an important role in the genesis of the condition. Both humans and dogs with AHAC/hypercortisolism demonstrate insulin resistance, and the relationship has long been established (Karnieli et al, 1985; Peterson et al, 1984). Earlier medical literature for both humans and dogs (Hess, 2010) speculated that hypercortisolism causes insulin resistance, rather than the other way around. Hypercortisolism is common in overweight humans, a condition that was speculated to cause so much physiological stress as to spike cortisol levels and drive insulin resistance. Recent studies, however, have documented insulin resistance (IR) as playing a causal role in hypercortisolism, with affected patients demonstrating positive feedback of serum cortisol on further secretion. Patients who are merely obese but who do not have IR have normal negative feedback inhibition of further cortisone secretion (Prpić-Križevac et al, 2012). AHAC Treatment Four Marvels Combination (Si Miao San) All available evidence suggests insulin resistance should be targeted first in any treatment protocol for a dog presumptively diagnosed as having PDH, and in patients with AHAC, so it is surprising that unprocessed low glycemic index diets are never advocated in the literature for either condition. Instead, veterinarians move immediately to the use of drugs that either impair adrenal activity, or destroy the gland altogether. Insulin resistance is effectively permitted to endure and potentially lead to additional pathology. In this context, Chinese herbal medicine, together with diet change, provides a safe and effective means of treating AHAC and presumptive PDH. Herbal treatments can be integrated with drug therapy, or used in its place as long as symptom control is adequate. Perhaps the most important Chinese herbal therapy for the treatment of AHAC and presumptive PDH is Si Miao San (Four Marvels Combination). Si Miao San improves insulin sensitivity by protecting and enhancing insulin signalling (Yang et al, 2014; Liu et al, 2010). Berberine, a plant compound extracted from Phellodendron in Si Miao Sanhas been shown through a systematic review of clinical trials to improve multiple aspects of type II diabetes and insulin resistance, including blood glucose markers such as HbA1c, hyperlipidemia, and hypertension (Lan et al, 2015). Four Marvels Powder (Si Miao San) Cang Zhu Atractylodes rhizome Huai Niu Xi Achryanthes root Yi Yi Ren Coix seed Huang Bo Phellodendron bark Case Example Sensei, a 12 year old female spayed Bichon-Shih-Tzu cross, presented with signs and symptoms compatible with pituitary dependent hyperadrenocorticism and AHAC, including: Thinning hair over the dorsum Increased ALP (about five times normal) Hyperlipidemia Hypercholesterolemia Sensei had been eating a heavily processed diet for years (z/d, Hills) in a vain attempt to control chronic pruritis. An abdominal ultrasound showed normal-sized adrenal glands and homogenous hyperechoic changes in the liver consistent with of steroid hepatopathy. An ACTH stimulation test showed normal cortisol levels prior to testing and cortisol levels well above normal after stimulation. A diagnosis of hyperadrenocorticism was rendered. Four Marvels Combination (Natural Path Herb Company) was prescribed in granular extract form, at a dose of 1 gram per 10 lbs (0.2 mg/kg) BID. Additionally, Sensei was prescribed a commercial raw diet supplemented with cooked vegetables and the z/d was discontinued. No pharmaceutical treatment was offered. Within two months, the owner was reporting reduced thinning of Sensei’s haircoat and a 50% reduction in itch. Laboratory testing at that time revealed ALP levels were only 50% above high normal. Treatment with Four Marvels and a low glycemic index diet was continued. In another three months, five months after treatment was initiated, a repeat ACTH stimulation test revealed normal cortisol levels pre- and post-testing. ALP and cholesterol levels were well within normal limits, with mild lipemia being noted in the blood sample. Approximately one year later, a chemistry screen showed ALP to still be well within normal limits. Mild lipemia of the sample was noted. Four Marvels has been continued to the present day, now 2 years later, although another berberine-containing formula (Hoxsey-Like Combination, Natural Path Herb Company) was added at a dose of 1 ml BID (0.1 ml per kg) to achieve better control of recurrent otitis externa and vulvar irritation. Case Discussion Sensei represents a case of presumptive PDH, although no confirmation was made of the presence of a pituitary adenoma. No effect of Four Marvels Combination or its components is reported in the literature on the pituitary gland. A clear, comprehensive, and sustained response to Four Marvels Combination, with its known insulin-sensitizing effects, suggests a diagnosis of AHAC is as likely as PDH. Four Marvels Combination does have the ability to lower cortisol levels directly, however. Phellodendron has been shown to reduce cortisol secretion during stress (Talbott et al, 2013), and stress from obesity was conjectured in the early literature as being the cause of hypercortisolism (Lindholm, 2014). Furthermore Coix, also known as Adlay, has been shown to suppress cortisol release from the adrenal gland itself (Chang et al, 2006). Other herbal formulas also increase insulin sensitivity but do not influence the adrenal cortex or the pituitary gland. A response of a case like Sensei to these formulas would thus provide more direct evidence that: AHAC is caused by insulin resistance Cases diagnosed routinely diagnosed as PDH are likely AHAC patients Wei Ling Tang (Harmonize the Stomach with Poria Five Herb Combination) Wei Ling Tang contains two sub-formulas, Ping Wei San (Harmonize the Stomach Combination) and Wu Ling San (Poria Five Herb Combination). Of the two, only Wu Ling San was traditionally indicated for signs of diabetes including polyuria with unslakable thirst. Research confirms an anti-diabetic effect, both by protecting beta islet cells and improving insulin signalling in insulin resistance (Jung et al, 2012; Han et al, 2013). A shared ingredient with Si Miao San of Wei Ling Tang is Atractylodes, which has been shown to improve several metrics in diabetic patients (Shi et al, 2006). No effect of either of the constituent formulas has been reported on adrenal cortical or pituitary actitivty. Wu Ling San (Poria Five Herb Combination) Harmonize the Stomach (Ping Wei San) Bai Zhu White Atractylodes rhizome Cang Zhu Atractylodes rhizome Fu Ling Poria Chen Pi Citrus peel Ze Xie Alisma tuber Hou Po Magnolia bark Zhu Ling Polyporus Da Zao Jujube Gui Zhi Cinnamon twig Gan Cao Licorice root Sheng Jiang Ginger rhizome Case Example Emma, a 2 year old female spayed Pomeranian, presented in 2010 with a chief complaint of thinning hair coat. She weighed approximately 5 lbs. through the course of treatment. Testing for hyperthyroidism revealed low circulating T3 and an ACTH test response test indicated hyperadrenocorticism. About a year after treatment was initiated, an ultrasound revealed bilateral adrenal gland enlargement One of the owner’s top goals was for the alopecia not to progress. Treatment with trilostane was thus initiated at a dose of 1 mg/lb (suggested dose range for the drug is 1-3 mg/lb). Treatment with trilostane continued until November of 2014, at doses varying between 0.5 – 1 mg/lb. Additionally, for much of that period, and in particular the first and last eight months, Emma also received Wei Ling Tang. Emma’s diet was a commercial raw food diet. Treatment results are shown in the figure below: 1200 1000 800 600 400 200 Pre 1-Oct-14 1-Jul-14 1-Apr-14 1-Jan-14 1-Oct-13 1-Jul-13 1-Apr-13 1-Jan-13 1-Oct-12 1-Jul-12 1-Apr-12 1-Jan-12 1-Oct-11 1-Jul-11 1-Apr-11 1-Jan-11 1-Oct-10 1-Jul-10 1-Apr-10 1-Jan-10 0 Post Figure 1. ACTH Stimulation test results for Emma The most ACTH stimulation test results are not shown in the chart above, but were normal. At that time, Emma had been off trilostane for two months. Hairloss did progress to bilateral truncal alopecia with Emma, but then improved to involve primarily just the caudal aspect of the hind limbs. No other significant laboratory abnormalities were noted over the course of treatment. Case Discussion The red horizontal line in the chart above indicates high normal for cortisol levels post-ACTH stimulation testing, and the bottom line indicates high normal for pre-stimulation testing. Apart from at the start of treatment, Emma remained within the normal range for both, including the last two to three months, when the dog was no longer on trilostane. Concomitant use of a low glycemic index raw diet and Wei Ling Tang appears to have allowed low to sub-normal doses of trilostane to be used throughout treatment, and for the drug to be withdrawn with impunity at the conclusion of treatment. Given that the main treatment effect of both herbs and diet was through insulin-sensitization, the PDH diagnosed in Emma is perhaps more likely to be a form of ACAH. Conclusions Hypercortisolism, or AHAC, appears to be occurring in dogs to an unappreciated degree. It is typically suspected only when a dog with consistent clinical findings does not test positive for PDH in stimulation tests. Given its association with insulin resistance, however, it should probably be suspected when a low glycemic diet and insulin sensitizing herbs effect clinical improvements or resolution. There is also nothing about what is known about AHAC to preclude affected animals testing positive on stimulation tests, as with humans. If many PDH dogs actually have AHAC, symptomatic treatment through reliance upon drugs toxic to the adrenal glands is far less optimal a treatment option than insulin sensitization through diet change, with or without herbal supplementation. Herbal medicines and unprocessed diets that improve insulin sensitivity are more definitive and safe treatment approaches, and will prevent drug side effects, progression to hypoadrenocorticism, and the progression of untreated insulin resistance. Where pharmaceuticals are elected for use, they should ideally be supplemental to an insulin sensitizing protocol. Concomitant herbal medicine can reduce the required dose to manage patients, helping limit side effects and sequelae of drug use, and perhaps obviate the need for drug use long term. References Behrend EN, Kennis R. Atypical Cushing's syndrome in dogs: arguments for and against. Vet Clin North Am Small Anim Pract. 2010 Mar;40(2):285-96 Björntorp P, Rosmond R. Obesity and cortisol. Nutrition. 2000 Oct;16(10):924-36. Chang LL, Wun AW, Hung CT, Hsia SM, Chiang W, Wang PS. Effects of crude adlay hull acetone extract on corticosterone release from rat zona fasciculata-reticularis cells. Naunyn Schmiedebergs Arch Pharmacol. 2006 Nov;374(2):141-52 de Bruin C, Meij BP, Kooistra HS, Hanson JM, Lamberts SW, Hofland LJ. Cushing's disease in dogs and humans. Horm Res. 2009 Jan;71 Suppl 1:140-3. Frank LA, Henry GA, Whittemore JC, Enders BD, Mawby DI, Rohrbach BW. Serum cortisol concentrations in dogs with pituitary-dependent hyperadrenocorticism and atypical hyperadrenocorticism. J Vet Intern Med. 2015 Jan;29(1):193-9. Góth M, Hubina E, Korbonits M. Correlations between the hypothalamo-pituitary-adrenal axis and the metabolic syndrome. Orv Hetil. 2005 Jan 9;146(2):51-5. Han Y, Jung HW, Bae HS, Park YK. Wen-pi-tang-Hab-Wu-ling-san, a Polyherbal Medicine, Attenuates ER Stress in 3T3-L1 Preadipocytes by Promoting the Insulin Signaling Pathway. Evid Based Complement Alternat Med. 2013 Hess RS. Insulin resistance in dogs. Vet Clin North Am Small Anim Pract. 2010 Mar;40(2):309-16. Jung HW, Jung JK, Ramalingam M, Yoon CH, Bae HS, Park YK. Anti-diabetic effect of Wen-pi-tang-HabWu-ling-san extract in streptozotocin-induced diabetic rats. Indian J Pharmacol. 2012 Jan;44(1):97-102. Islam A, Chen Y, Poth M, Smith ZP, Deuster PA. Glucocorticoid receptor density correlates with health risk factors and insulin resistance in Caucasian and African American subjects. Exp Clin Endocrinol Diabetes. 2012 Sep;120(8):477-81 Lan J, Zhao Y, Dong F, Yan Z, Zheng W, Fan J, Sun G. Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. J Ethnopharmacol. 2015 Feb 23;161:69-81 Lindholm J. Cushing's disease, pseudo-Cushing states and the dexamethasone test: a historical and critical review. Pituitary. 2014 Aug;17(4):374-80. Liu K, Luo T, Zhang Z, Wang T, Kou J, Liu B, Huang F. Modified Si-Miao-San extract inhibits inflammatory response and modulates insulin sensitivity in hepatocytes through an IKKβ/IRS-1/Akt-dependent pathway. J Ethnopharmacol. 2011 Jul 14;136(3):473-9. Pasquali R, Vicennati V. Activity of the hypothalamic-pituitary-adrenal axis in different obesity phenotypes. Int J Obes Relat Metab Disord. 2000 Jun;24 Suppl 2:S47-9. Peterson ME. Diagnosis of hyperadrenocorticism in dogs. Clin Tech Small Anim Pract. 2007 Feb;22(1):211. Peterson ME, Altszuler N, Nichols CE. Decreased insulin sensitivity and glucose tolerance in spontaneous canine hyperadrenocorticism. Res Vet Sci. 1984 Mar;36(2):177-82. Prpić-Križevac I, Canecki-Varžić S, Bilić-Ćurčić I. Hyperactivity of the hypothalamic-pituitary-adrenal axis in patients with type 2 diabetes and relations with insulin resistance and chronic complications. Wien Klin Wochenschr. 2012 Jun;124(11-12):403-11 Shi J, Hu Y, Wang Q. Fufang cangzhu tang for treatment of senile obesity or overweight complicated with impaired glucose tolerance --a clinical observation in 32 cases. J Tradit Chin Med. 2006 Mar;26(1):33-5. Talbott SM, Talbott JA, Pugh M. Effect of Magnolia officinalis and Phellodendron amurense (Relora®) on cortisol and psychological mood state in moderately stressed subjects. J Int Soc Sports Nutr. 2013 Aug 7;10(1):37 Van Liew CH, Greco DS, Salman MD. Comparison of results of adrenocorticotropic hormone stimulation and low-dose dexamethasone suppression tests with necropsy findings in dogs: 81 cases (1985-1995). J Am Vet Med Assoc. 1997 Aug 1;211(3):322-5. Yang JL, Wang JL, Huang F, Liu K, Liu BL. Modified Si-Miao-San inhibits inflammation and promotes glucose disposal in adipocytes through regulation of AMP-kinase. Chin J Nat Med. 2014 Dec;12(12):9119.