Supplementry Box 1 | Screening and prophylaxis of latent TB TNF is
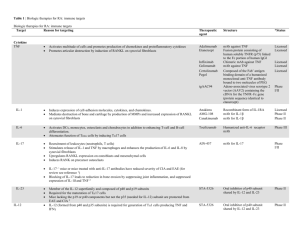
advertisement

Supplementry Box 1 | Screening and prophylaxis of latent TB TNF is important in the control of TB granuloma integrity and function. TNF antagonists increase the risk of reactivation of TB in patients with latent infection, especially in patients with diabetes mellitus or chronic renal disease.S1 Strict screening for latent TB before initiating anti-TNF therapy (with subsequent prophylactic therapy) is supported by studies showing a decrease in the number of active TB cases.S2 IGRA specific for M. tuberculosis (T-Spot.TB® [Oxford Immunotec, UK] and QuantiFERON®[Qiagen, Netherlands]) are now replacing less specific TSTs. TSTs do not distinguish between previous exposure to TB and BCG vaccination.S3–S5 The different pretest probabilities according to different geographic regions should be considered with IGRA.S5 In areas with low rates of TB, false-positive TSTs are a concern, supporting the use of IGRA, whereas in areas of high TB transmission, the risk of false negativity might justify using TSTs.S6 The following conditions need to be fulfilled before initiating prophylactic TB therapy: IGRA should be performed before beginning any immunosuppressive treatment. Any therapy decreasing the activity or number of antigen-presenting cells or T cells can increase the risk of false-negative resultsS7–S10 Patient medical history, including previous active TB, therapies, risk of exposure, origin and residence in TB endemic areas, needs to be carefully reviewed Radiography might be needed If evidence of latent TB, start prophylactic treatment with isoniazid for 9 months (5 mg/kg up to a maximum 300 mg per dose, once daily) or rifampicin for 4 months (10 mg/kg per day: maximum dose of 600 mg per day).S11 Treatment with TNF antagonists can be initiated 1 month after beginning TB prophylaxisS1 In patients previously treated for active TB, prophylaxis is not needed if compliance with prior TB therapy is established Abbreviations: IGRA, IFN-γ release assay; TB, tuberculosis; TST, tuberculin skin test. References s1. Winthrop, K.L., Siegel, J.N., Jereb, J., Taylor, Z. & Iademarco, M.F. Tuberculosis associated with therapy against tumor necrosis factor α. Arthritis Rheum. 52, 2968-2974 (2005). s2. Carmona, L. et al. Effectiveness of recommendations to prevent reactivation of latent tuberculosis infection in patients treated with tumor necrosis factor antagonists. Arthritis Rheum. 52, 1766-1772 (2005). s3. Hsia, E.C. et al. Comprehensive tuberculosis screening program in patients with inflammatory arthritides treated with golimumab, a human anti-tumor necrosis factor antibody, in Phase III clinical trials. Arthritis Care Res. (Hoboken) 65, 309-313 (2013). s4. Mariette, X. et al. Influence of replacing tuberculin skin test with ex vivo interferon γ release assays on decision to administer prophylactic antituberculosis antibiotics before anti-TNF therapy. Ann. Rheum. Dis. 71, 1783-1790 (2012). s5. Kleinert, S. et al. Screening for latent tuberculosis infection: performance of tuberculin skin test and interferon-γ release assays under real-life conditions. Ann. Rheum. Dis. 71, 1791-1795 (2012). s6. Kardos, M. & Kimball, A.B. Time for a change? Updated guidelines using interferon γ release assays for detection of latent tuberculosis infection in the office setting. J. Am. Acad. Dermatol. 66, 148-152 (2012). s7. Jung, J.Y. et al. Questionable role of interferon-γ assays for smear-negative pulmonary TB in immunocompromised patients. J. Infect 64, 188-196 (2012). s8. Martyn-Simmons, C.L., Mee, J.B., Kirkham, B.W., Groves, R.W. & Milburn, H.J. Evaluating the use of the interferon-γ response to Mycobacterium tuberculosis-specific antigens in patients with psoriasis prior to antitumour necrosis factor-α therapy: a prospective head-to-head cross-sectional study. Br. J. Dermatol. 168, 1012-1018 (2013). s9. Mori, T. Usefulness of interferon-γ release assays for diagnosing TB infection and problems with these assays. J. Infect. Chemother. 15, 143-155 (2009). s10. Sanduzzi, A. et al. Screening and monitoring of latent tubercular infection in patients taking tumor necrosis factor-alpha blockers for psoriatic arthritis. J. Rheumatol. 89, 82-85 (2012). s11. No authors listed. Targeted Tuberculin Testing and Treatment of Latent Tuberculosis Infection. American Thoracic Society and CDC Statement Committee. MMWR Recomm. Rep. 49, 1-51 (2000). Supplementary Table 1 | Biologic agents used to treat rheumatic and immunological disorders Target Biologic agent (commercial name) Structure Dose* T1/2 Indications mAb (IgG4κ) Route of adminis tration IV α4-integrin (CD49d) Natalizumab§ (Tysabri®) 300 mg every 4 weeks 11 days Belimumab (Benlysta®) mAb (IgG1) IV 19 days CD20 Rituximab (MabThera®) mAb (IgG1) IV 22 days RA, AAV CD80 Abatacept (Orencia®) CTLA-4–IgG1-Fc IV 15 days RA, JIA IL-1Rα and IL-1β IL-1β Anakinra (Kineret®) Canakinumab (Ilaris®) recombinant IL-1Ra mAb (IgG1κ) SC 5 hours RA, CAPS 26 days CAPS IL-1β Gevokizumab (XOMA-052) mAb (IgG2) SC 22 days IL-1α, IL-1β and IL-1Ra IL-6Rα Rilonacept (Arcalyst®) Tocilizumab (RoActemra®) sIL-1R–IgG1-Fc SC 9 days Noninfectious posterior uveitis, Behçet uveitis CAPS mAb (IgG1) IV 12 days RA, JIA IL-17RA Brodalumab (AMG 827) mAb (IgG2) SC NA Psoriasis╪ IL-17A Ixekizumab (LY2439821) mAb (IgG4) SC NA Psoriasis╪ IL-17A Secukinumab (AIN457) mAb (IgG1κ) IV 28 days Psoriasis╪ p40 subunit of IL-12 and IL-23 TNF Ustekinumab (Stelara®) mAb (IgG1κ) SC 21 days Psoriasis Adalimumab (Humira®) mAb (IgG1) SC 15 days TNF Certolizumab pegol (Cimzia®) PEG-Fab’ (IgG1) SC RA, JIA, AS, Crohn disease, psoriasis Crohn disease, RA TNF and lymphotoxin-β Etanercept (Enbrel®) TNFR2–IgG1-Fc SC TNF Golimumab (Simponi®) mAb (IgG1) SC TNF Infliximab mAb (IgG1) IV 10 mg/kg every 4 weeks 4×375 mg/ m2 or 2×500– 1000 mg 500– 1000 mg every 4 weeks 100 mg every day 150 mg every 8 weeks 60 mg every 4 weeks 160 mg every week 4–8 mg/kg every 4 weeks 140 mg every 2 weeks 80 mg every 4 weeks 10 mg/kg every 3 weeks 45 mg every 12 weeks 40 mg every 2 weeks 200– 400 mg every 2– 4 weeks 2×25 mg every week or 1×50 mg every week 50–100) mg every 4 weeks 3– Relapsing remitting multiple sclerosis, Crohn disease SLE BAFF SC 14 days 4 days RA, JIA, AS, Crohn disease, psoriasis 14 days RA, AS, psoriatic arthritis 9 days RA, JIA, AS, (Remicade®) 10 mg/kg Crohn disease, every 4– ulcerative colitis, 8 weeks psoriasis *Dose is only exemplary and does not replace consultation of the pharmaceutical package insert. Indications are approved for rheumatic and immunological disorders, except those marked ╪. §Natalizumab was temporarily withdrawn from the market in 2004 and reintroduced in 2006. Abbreviations: AAV, anti-neutrophil cytoplasmic antibody-associated vasculitis; AS, ankylosing spondylitis; BAFF, B-cell-activating factor; CAPS, cryopyrin-associated periodic syndrome; CTLA-4, cytotoxic T lymphocyte antigen 4; IL-1Ra, IL-1 receptor antagonist; IL-6Rα, IL-6 receptor α; IV, intravenous; JIA, juvenile idiopathic arthritis; mAb, monoclonal antibody; NA, not available; PEG-Fab’, pegylated Fab’ fragment; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; SC, subcutaneous; sIL-1R, soluble IL-1 receptor; TNFR2, TNF receptor 2;