Ref :(1) Collapse of intramuscular free amino acid pools in patients
advertisement

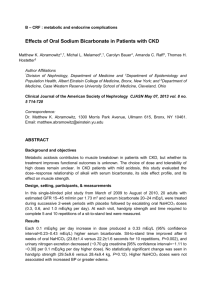
O28 RESISTANCE EXERCISE INCREASES MUSCLE MASS AND PRESERVES INTRAMUSCULAR AMINO ACID CONCENTRATIONS IN PRE-DIALYSIS CKD: A RANDOMISED CONTROLLED TRIAL Watson, E1, Greening, N2, Aulakha, J1, Ruttanaporn, N1, Young, H2, Dungey, M3, Burton, J2, Barratt, J1, Smith, A2,1 1 Department of Infection, Immunity and Inflammation, University of Leicester, 2John Walls Renal Unit, Leicester General Hospital, 3School of Sport, Exercise and Health Sciences, Loughborough University INTRODUCTION: Patients with chronic kidney disease (CKD) suffer from skeletal muscle wasting which is associated with morbidity and mortality and worsens as renal function declines. This loss of muscle mass leads to fatigue and weakness, and can limit the ability to take aerobic exercise which has proven cardiovascular benefits in this very high risk population. In a previous study (1), we found that an aerobic exercise programme failed to increase muscle mass in CKD, and instead resulted in depletion of intramuscular free amino acids. Progressive resistance exercise (PRE) effectively stimulates muscle hypertrophy in the general population, but its ability to overcome the catabolic influences associated with pre-dialysis CKD has not been properly studied. The aim of this randomised controlled trial was to investigate the effects of an 8 week PRE programme in CKD patients stage 3b-4. METHODS: 20 patients (10 males, 63[45-80] years, eGFR 28[15-37] ml/min/1.73m2) were randomised to PRE training consisting of 3 sets of 10-12 leg extensions at 70% 1 repetition maximum, 3 times a week for 8 weeks. 18 patients were randomised to control (13 male, 65.5[45-79] years, eGFR 20.5[15-40] ml/min/1.73m2) and continued with their usual physical activity. Outcome assessments were carried out at baseline and 8 weeks and included rectus femoris anatomical crosssectional area (ACSA) by ultrasonography, isokinetic muscle strength by dynamometry, exercise capacity by endurance shuttle walk test (ESWT), and patient perception of common uraemic symptoms by questionnaire. Rectus femoris muscle biopsies were obtained in the fasted state at baseline and 8 weeks, and intramuscular amino acid concentration determined by high performance liquid chromatography (HPLC). RESULTS: 18 exercisers and 15 controls completed the study. Adherence to PRE was good, with a 92% attendance rate at exercise sessions. No changes were seen in the controls for any outcome measure, except for a decrease in the time walked in the ESWT (P=0.03) indicating reduced exercise capacity. In contrast, patients who undertook the PRE programme had a significant increase in EWST walking performance (9.7±7.7 vs 12.4±8.0min P=0.03), and reported a significant reduction of the impact of uraemic symptoms (p=0.01). The exercise group also had significantly increased ACSA (6.03±2.1 vs 6.6±2.2cm2 P=0.002) and knee extensor strength (95.6±8.2 vs 108.9±8.5Nm, p<0.001), and HPLC analysis of muscle biopsies demonstrated preservation of free amino acid levels (p>0.05 for all 17 amino acids measured) following exercise training. CONCLUSION: 8 weeks of PRE resulted in significant gains in skeletal muscle and strength and maintained intramuscular amino acid concentrations, the depletion of which may limit ability to increase muscle mass in response to exercise. These results indicate that PRE can effectively overcome catabolic influences to preserve or improve muscle mass in CKD. Furthermore, although the exercise programme did not include aerobic training, walking performance significantly improved, suggesting that muscle wasting and weakness is an important limiting factor in physical capacity in CKD. This study demonstrates that PRE is a well-tolerated and effective strategy to maintain muscle mass, physical functioning and quality of life in patients with CKD. Ref :(1) Collapse of intramuscular free amino acid pools in patients with CKD4-5 after 6 months of walking exercise is prevented by alkali supplements, Clapp et al., presented at International Congress on Nutrition and Metabolism in Renal Disease,2010.