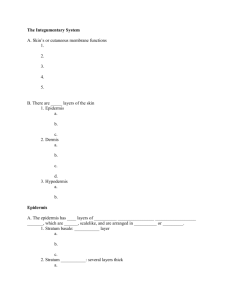
SKIN lecture and lab notes
advertisement

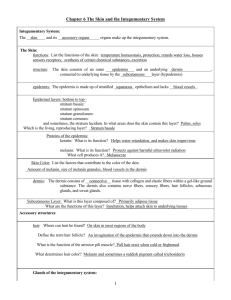
H I S T O L O G Y L E C T U R E INTEGUMENT OBJECTIVES: Upon completion of study of this section the student will be able to: List the barrier, protection and regulatory functions of the skin. Indicate the role of epidermal and dermal components in each function. Distinguish between thick and thin skin. Including location and components found in each type. Describe the 5 strata found in the epidermis. Review the development and organization of each layer. Discuss the origin and role of melanocytes. Trace the development and fate of the granule. Identify the function of Langerhan’s and Merkel’s cells. Describe the organization and functions of the papillary and reticular layers of the dermis. Describe the structure and activities of the hair follicles, sebaceous, eccrine and apocrine sweat glands. Integumentary System refers to the skin plus its appendages. covers the surface of the body and is composed of two layers: epidermis and dermis. The deeper fascial layer, the hypodermis, is not considered part of skin. serves several important functions: protection against injury, desiccation, and infection; the regulation of body temperature; the absorption of UV radiation for synthesis of vitamin D; and the reception of sensory stimuli (tactile, thermal, and pain) from the external environment. epidermis and dermis interdigitate with each other to form an irregular contour. Dermal papillae (ridges) project into the epidermis to produce epidermal ridges (which can be seen on the finger tips with the naked eye). may also be classified as thick or thin, depending on the thickness of epidermis. Skin 1. Appendages of Skin includes sweat glands, hair follicles, sebaceous glands, and nails. General Structural Plan of Skin Epidermis Characteristics a stratified squamous keratinized epithelium, composed of several strata, which forms the superficial layer of skin. is constantly being regenerated by its keratinocytes (every 2 to 4 weeks) via mitotic activity that occurs mostly at night. epithelial layers of the epidermis include the following strata: basale, spinosum, granulosum, lucidum, and corneum: 1. Stratum Basale (germinativum) is the deepest layer of cells, attached directly to the basal lamina by hemidesmosomes. cuboidal to columnar in shape and frequently seen undergoing division. melanocytes (pigment cells) and Merkel cells are also present in this layer. 2. Stratum Spinosum consists of a few layers of polyhedral (prickle) keratinocytes. these cells have extensions, or so-called “intercellular bridges”, where desmosomes attach the cells to each other. cells of this layer are mitotically active. in upper regions of the stratum spinosum are keratinocytes that contain membranecoating granules, which are released into the intercellular spaces and cement the cells together, “waterproofing” the skin. Langerhans cells also present in this layer. 3. Stratum Malpighii refers to the stratum basale and the stratum spinosum grouped together. 4. Stratum Granulosum the layer of the epidermis where cells accumulate keratohyalin granules and bundles of intermediate keratin filaments (tonofilaments) and become flattened. also produce membrane-coating granules. Keratohyalin Granules are not enclosed in a membrane but are composed of histidine- and cystine-rich proteins that appear to bind the keratin filaments together. Cytoplasmic Aspect of the plasmalemma of these keratinocytes is thickened by an electron-dense layer, 10 - 12 nm thick, that reinforces it. is the most superficial layer in which nuclei are present. 5. Stratum Lucidum a clear homogeneous layer, which is often difficult to distinguish in histological sections. nuclei and organelles are not present in this layer, and the cells contain a substance known as eleidin, which is believed to be a transformation product of keratohyalin. 6. Stratum Corneum is the outermost layer of the epidermis. is composed of scale-like dead cells (squames). each squame is a 14-sided polygon surface layers of cells are constantly being desquamated, region being desquamated is sometimes referred to as the stratum disjunctum. 7. Other Cell Types in the Epidermis Melanocytes are present in the stratum basale and derived from the neural crest. synthesize brown melanin pigment in oval organelles called melanosomes. contain tyrosinase, a UV-sensitive enzyme directly involved in melanin synthesis. contain long processes that extend between the cells of the stratum spinosum. by way of these processes, the melanocytes transfer (or inject) melanosomes into keratinocytes in the stratum spinosum. this unique mechanism for the transfer of pigment is known as cytocrine secretion. once melanosomes are within the keratinocytes, they are degraded by lysosomes. number of melanocytes per unit area of skin varies from one part of the body to another but is independent of race. Langerhans Cells are dendritic-shaped cells derived from the bone marrow. are present mainly in the stratum spinosum. contain distinct paddle-shaped membrane-bounded granules (Birbeck granules). function in presenting antigen to lymphocytes and thereby play a role in contact allergic responses. Merkel Cells are present in small numbers in the stratum basale, near areas of connective tissue containing blood vessels and nerves. contain small dense-cored granules that are similar in appearance to those in cells of the adrenal medulla. receive afferent nerve terminals and are believed to function as sensory mechanoreceptors. is composed of thin, loosely arranged fibers and cells. Dermis 1. Characteristics layer of skin underlying the epidermis that consists of dense, irregular connective tissue. contains collagen (Type I) fibers in abundance and networks of thick elastic fibers. is divided into a superficial papillary layer and a deeper more extensive reticular layer, but there is no distinct boundary between them. 2. Papillary layer is uneven and forms dermal papillae that interdigitate with the basal surface of the epidermis. is composed of thin, loosely arranged fibers and cells. Meissner’s corpuscles (fine-touch receptors) and capillary loops are located in this layer. 3. Reticular Layer forms the major portion of the dermis and contains thick, dense, irregular arrays of collagen fiber bundles and thick elastic fibers. Encapsulated Nerve Endings consisting of Pacinian corpuscles (pressure receptors) and Krause’s end bulbs (cold and pressure receptors) may be present in the deeper regions of the dermis. Arrector Pili Muscle are bundles of smooth muscle, attached to hair follicles in the dermis, extend superficially to underlie sebaceous glands, and insert into the papillary layer of the dermis. contraction of arrector pili muscle elevates the hair and produces “goose bumps”. deep to the reticular layer is the superficial fascia, or hypodermis, a loose connective tissue, containing many fat cells, that is not considered part of the skin. Two Types of Skin 1. Thick Skin has a thick epidermis that is characterized by a prominent stratum corneum. lines the palms of the hands and the soles of the feet. lacks hair follicles, sebaceous glands, and arrector pili muscle bundles. 2. Thin Skin has a thin epidermis with a less prominent stratum corneum. is present over most of the body surface and contains hair follicles, sebaceous glands, and arrector pili muscle bundles. stratum lucidum and stratum granulosum are seldom seen in thin skin, although individual cells are present that show characteristics of these layers. the dermis is usually thicker in this area than in thick skin. Appendages of the skin 1. Hair Follicle a tubular invagination of the epidermis extending deep into the dermis. shaft of the hair projects above the surface of the epidermis. hair consists of a medulla, cortex and cuticle. root of the hair is embedded in an expanded hair bulb, which is deeply indented by a papilla (of dermis). cells in the hair bulb form the inner epithelial root sheath and the medulla. internal root sheath is an epithelial structure (lying deep to the entrance of the sebaceous gland) composed of Henle’s layer, Huxley’s layer, and the cuticle. outer root sheath is a direct continuation of the stratum Malphighii of the epidermis. the next superficial layer is the glassy (basement) membrane, and the outermost layer is the connective tissue sheath (dermis). 2. Nail is located on the distal phalanx of each finger or toe. is composed of hard keratin lying on a nail bed. eponychium (cuticle) overlies the crescent-shaped whitish lunula. hyponychium (keratinized epithelial layer) is located beneath the free edge. cells in the nail matrix, at the root, are responsible for the growth of the nail. Glands Eccrine Sweat Glands are distributed in skin throughout the body. are simple tubular coiled glands that have a secretory unit composed of three cell types: dark cells, clear cells, and myoepithelial cells. 1. Secretory Unit (of eccrine gland): Dark cells - line the lumen and contain secretory granules Myoepithelial cells - lie on the basal lamina scattered beneath the clear cells Clear cells - passes intercellular canaliculi which extend to the lumen of of the secretory unit - underlie the dark cells and are rich in mitochondria and glycogen 2. Duct of Eccrine Gland is narrow and lined by a stratified cuboidal epithelium. leads from the secretory unit, through the superficial portions of the dermis, to penetrate the interpapillary peg of the epidermis and spiral through its layers to deliver sweat to the outside. cell type lining the narrow lumen of the sweat duct contains many keratin filaments and has a prominent terminal web. in contrast, the basal layer of cells has many mitochondria and prominent nuclei. Apocrine Glands are large specialized sweat glands located in various area of the body, such as the axilla, the areola of the nipple, and the circumanal region. do not begin to function until puberty and are responsive to hormonal influences. have a large coiled secretory portion enveloped by scattered myoepithelial cells. empty their viscous secretory products into hair follicles at a location superficial to the entry of ducts from sebaceous glands. are innervated by adrenergic fibers. apocrine implies that a portion of the cytoplasm becomes part of the secretion, but electron micrographs have shown that this is not true. Ceruminous (wax) Glands of the external auditory canal are also included in this category. Sebaceous Glands consist of several sacs (alveoli) that empty into a short duct, which in turn empties into the neck of a hair follicle. cells at the periphery of the alveoli are flattened and inactive, but near the ducts mitosis are common. daughter cells migrate to the alveolus, produce a secretory product and begin to break down, releasing an oily secretion known as sebum. process is known as holocrine secretion (both the disintegrated cells and the secretory material are discharged). C L I N I C A L I N T E G R A T I O N INTEGUMENT INTRODUCTION: Skin is the largest organ in the body. It is made up of epidermis and dermis. Hypodermis is not part of the skin. Epidermis is made of 5 layers of cells. Terms to understand: HYPERKERATOSIS- hyperplasia of the horny layer of the skin (or the cornea). PARAKERATOSIS- retention of nuclei in the stratum corneum of the skin. AUTOIMMUNE- immune response of the body against its own tissues, cells or molecules. ACANTHOLYSIS- loss of intercellular connections resulting in loss of cohesion between keratinocytes ACANTHOSIS- epidermal hyperplasia (S. Spinosum) COMPLEMENT SYSTEM – group of protein that effect lysis of cells & Ag-Ab complexes, and cytokine release. CLINICAL INTEGRATION CASES: Psoriasis Bullous Pemphigoid Pemphigus Vulgaris Albinism Acne Psoriasis: Common chronic inflammatory condition. Worldwide incidence varies, but prevalent in European population, rare in Blacks and American Indians. Affects 2% of US population. Distributed over extensor body surfaces (esp. knee and elbow) scalp and lumbosacral areas. Equal sex distribution . Etiology – autoimmune ( T- cells stimulation -cytokines) Etiology – autoimmune( T- cells stimulation -cytokines) Autoimmune T- cells (cytokines) Histopathogenesis : Increased epidermal turnover (3 – 5days) ---marked epidermal thickening and increase in size of epidermal ridges. Abnormal keratinocyte differentiation: loss of S. granulosum. S. corneum thickening and nuclei retention. Weak junctional complexes in superficial layer ( silvery scales) Bullous Pemphigoid: Chronic autoimmune blistering disease: skin & mucous membranes. Histopathogenesis: Presence of IgG antibodies specific to hemidesmosomes . Autoantibodies (IgG) bind to basement membrane and stimulate leucocytic infiltration. Eosinophils release proteases that degrade hemidesmosomes. Fluid accumulation – blister formation. Subepidermal, nonacantholytic blisters - hard to rupture . PEMPIGHUS VULGARIS Pemphix (blister / bubble). Rare autoimmune disorder affecting epidermis and mucosal epithelium Histopathogenesis: Auto-immune disorders.Body attacks self whereby antibodies target a component of desmosomes (cadherins and desmoplakins). Desmosomes (intercellular bridges) disrupted. Results in acantholysis. Separation of epidermal cells (S. Spinosum). Atrophy of the prickle cell layer. Blisters formation: (easy to rupture) Complications: Side effects of systemic medications. Secondary bacterial,viral, or fungal infection . Spread of infection through the bloodstream (sepsis). Loss of extensive amounts of body fluids & electrolytes.Fatal if untreated . Dysphagia, if in oral cavity. ALBINISM: Genetic , Loss of pigmentation of the skin, hair and eyes. Mutation in genes that regulate melanin synthesis and distribution of melanocytes. More common in Blacks than Whites.Presents in neonates. Melanin : Retinal development (RPE) & optic nerve routing. Types: Ocular + Oculocutaneous Histopathogenesis: Hereditary condition (autosomal recessive). Inability of the melanocytes to pick up tyrosine. Inactivity of the tyrosinase enzyme. tyrosinase Tyrosine DOPA Melanin VITILIGO: Depigmentation disorder. Auto immune.Destruction of melanocytes Types: Focal, Segmental, Generalized distribution in the body. ACNE: Histopathogenesis: Disturbance in the normal secretion and flow of sebum; Increase in sebum secretion (androgenic stimulation) Obstruction of the outflow tract of the sebaceous gland (keratin plugs). Superimposed bacterial infection. Chronic inflammation of the sebaceous gland. CARCINOMAS: SQUAMOUS CELL CARCINOMA: Cancer of the skin arising from the squamous cells (keratinized) Histopathogenesis: Malignant tumor of keratinocytes Exposure to UV with DNA damage (inactivation of P53 gene) Loss of orderly maturation with variability in nuclear size and shape Hyperkeratosis and parakeratosis Types: Superficial or infiltrative Dermis deeply infiltrated by islands and sheets of malignant squamous cells. The islands have undifferentiated cells, resembling basal cells, around the perimeter. Islands show squamous differentiation with formation of squamous pearls or swirls. BASAL CELL CARCINOMA: Carcinoma arises from the stratum basale cells. Histopathogenesis: UV light Involves the basal cells Single arrangement of basal cells surrounding group of tumour cells - (Palisade arrangement) MALIGNANT MELANOMA: Malignant transformation of melanocytes. Causes highest # of skin cancer related deaths in US. More common in whites, Australia / S. Africa Etiology- exposure to sunlight (UV): (acute, intermittent, blistering) Histopathogenesis: Increased number of melanocytes with large atypical morphology and haphazardly arranged at the dermo-epidermal junction. May invade the dermis – metastases – fatal. H I S T O L O G Y L A B O R A T O R Y Integument OBJECTIVES: Upon completion of study or this section the student will be able to: Distinguish between the 5 layers of epidermal cells in thick skin and the differences in these found in thin skin. Describe the organization of the two layer comprising the dermis. Detail the structure and subdivisions of the pilosebaceous follicle. Identity the sweat gland and distinguish the duct from the secretory region. List the cells found in the secretory region and identify the function of each. ANNOTATIONS The skin is comprised of an outer epithelium, the epidermis, and underlying mesenchymal component, the dermis. The epidermis layer is a stratified squamous keratinizing epithelium that possesses a scattered population of melanocytes, Langerhans’ and Merkel’s cells. The dermis is a relatively dense irregular connective tissue, except for a thin cellular zone, the papillary layer, that lies directly beneath the epidermis. The major portion of the dermis, called the reticular layer, contains thick woven bundles of type I collagen and provides a reinforcing physical substrate for the cellular epithelium. Epithelial derivatives of the epidermis include hair follicles, sebaceous glands and sweat glands. These structures descend from the surface epithelium and are contained within the connective tissue of the dermis. There are two types of skin: thick skin and thin skin. Thick skin is normally restricted to the soles (plantar surface) of the feet and palmar surface of the hand, while all other skin is of the thin type. Characteristics of each type are described in the table below: CHARACTERS THICK SKIN THIN SKIN Surface Texture Alternating ridges and grooves Smooth Epidermis/Dermis Interface Interdigitating ridges Epidermal Strata S. Basale, S. Spinosum, S. Granulosum, S. Lucidum, S. Corneum Hairs and Sebaceous Glands None Dermal papillae alternating with epidermal pegs Same as thick skin, except: no S. Lucidum. The corneum, granulosum and spinosum layers are reduced in thickness Regionally variable Sweat Glands Abundant Moderate MICROSCOPIC STUDIES There will be 2 slides used in this exercise: 1. Skin corpuscle (Thick skin) 2. Scalp human I.s 1. Skin Corpuscle (Thick skin): Scan the section at lowest magnification and distinguish epithelium of epidermal surface from the connective tissue in the cut hypodermis region. Starting at apical surface identify the following three layers 1) epidermis - thick epithelial layer which is separated from underlying dermis by the “scalloped” layer of tightly packed cuboidal/low columnar cells that comprise the stratum basale: 2) dermis - is distinguished by the densely woven matrix of collagen bundles and paucity of nucleated cells; 3) hypodermis - is characterized by the clusters of unilocular adipose cells that are “encapsulated” by dense connective tissue matrices. At higher magnification focus upon the epidermis. The stratum corneum is the top and thickest layer. It is comprised of stacks of dead keratinocytes that are actually ghosts of former cells that are filled with tonofibrils (bundles of keratin intermediate filaments) enmeshed in a matrix derived from keratohyaline granules. The fibrils are not evident because they stain the same as the surrounding matrix. In specific regions of the corneum there are columns composed of stacked vesicles. These vessels are interconnected and represent the “ducts” of the sweat glands that penetrate the epidermis and exit at skin surface. As you descend deeper into the epidermis you will encounter a cell layer in which the keratinocytes characteristically possess basophilic keratohyaline granules. This region called the stratum granulosum is comprised of several layers of squamous cells. At the basal surface of the granulosum the cells exhibit a sparse sprinkling of bluish granules and intact nuclei. As you follow this layer toward the lumen the granules increase in size and density also the nuclei begin to show signs of degeneration (i.e., they become pyknotic). Through a process of autolysis, Iysosomes degrade the cytoplasmic components leaving only the tonofibrils, keratohyaline matrix and a lipid intracellular cement. When degeneration is complete, the cells have a glassy appearing cytoplasm and eosinophilic peripheral margin. These cells (4-5 layers) comprise the stratum lucidum that lies between the granulosum and overlying corneum. Beneath the granulosum is the malpighian layer, the cells of which express mitotic cell divisions (the layer responsible for “growth” of the epidermis). The basal surface of the malpighian layer is thrown up into folds which form the epidermal ridges that interdigitate with the underlying dermal ridges. The malpighian layer is actually comprised of two strata, the stratum spinosum and the stratum basale. The s. spinosum is multilayered and it’s cells characteristically exhibit large numbers of desmosomes around their periphery. The desmosomes provide a spiny or prickle appearance which accounts for the nomenclature of this stratum. Most of the spiny or prickle layer in your sections do not reveal this character, SO, scan the section until you find a region where individual keratinocytes possess a “moat-like” clear zone between themselves and adjacent cells. In these regions you may be able to identify the spines which represent the macula adherens junctions. The variable thickness of the Malpighian layer that accounts for the epidermal al ridges is due to variations in thickness of the s. spinosum. The bottom cell layer which sits upon the basement membrane, the stratum basale, is only one cell thick. The basale cells are cuboidal or low columnar, tightly packed and tightly adherent to the underlying basement membrane via hemidesmosomes. The variable thickness of the malpighian layer that accounts for the epidermal ridges is due to variations in thickness of the s. spinosum. The bottom cell layer which sits upon the basement membrane, the stratum basale, is only one cell thick. The basale cells are cuboidal or low columnar, tightly packed and tightly adherent to the underlying basement membrane via hemidesmosomes. Scan the basale layer and find regions in which the keratinocytes contain accumulations of brownish melanin granules. In these regions melanocytes are found between the basale cells and the basement membrane. The melanocytes are not readily distinguishable since they contain less pigment than the adjacent keratinocytes. Remember that as melanin is synthesized, the melanosomes are “injected” into adjacent keratinocytes via a process called cytocrine secretion. The underlying dermis is thrown up into ridges which serve to increase the adhesiveness of the epidermis to the dermis by creating a greater surface area. The dermis is composed of very thick bundles of collagen I that are interwoven into an irregular matrix. Interspersed among the collagen bundles is a well developed meshwork of elastic fibers. There are relatively few fibroblasts scattered among the collagen bundles. The zone directly beneath the epidermis, called the papillary layer, should contain many more cells and blood vessels than the lower and thicker acellular region of the dermis called the reticular layer. Cellular structures that cross the dermis by extending between the epidermis and hypodermis include the blood vessels and a number of epithelial sweat gland ducts. The sweat glands are simple tubular glands derived from the epidermis that penetrate the dermis as straight epithelial tubes and become highly coiled at the dermis-hypodermis interface. The sweat gland ducts are lined by a 2 cell-thick stratified cuboidal epithelium. In the coiled secretory regions the ducts also contain two layers, but these are not well presented in your sections. The secretory regions contain dark cells (glycoprotein [mucoid secreting cells), clear cells (electrolyte transporting cells) and a number of myoepithelial cells that sit upon the basement membrane. The darker staining and narrower ducts are easily distinguished from the secretory regions. Below the dermis is the hypodermis, which is not part of the skin but is a component of the superficial fascia. The hypodermis characteristically contains pads of unilocular adipose (panniculus adiposus) interspersed with dense connective tissue septa. Identify and check-off each of the following: Epidermis Hypodermis S. Lucidum S. Spinosum Malpighian layer Reticular layer of dermis Melanosomes (In keratinocytes) Sweat gland ducts Epidermal ridges Dermis Stratum corneum S. Granulosum S. Basale Papillary layer of dermis Fat pads Keratohyaline granules Sweat gland secretory regions 2. Scalp Human l.s: The scalp is lined by thin skin. Compare the structure and organization of the epidermis with that of the thick skin in the previous slide. You should observe that the stratum corneum is greatly reduced in thickness and that there is no visible stratum lucidum. The granulosum and spinosum layers are also significantly reduced in thickness. Could the basal layer also be reduced in thickness? Rather than the weII-developed ridges between the epidermis and dermis, thin skin exhibits a scattered population of epidermal pegs (knob-like cellular incursions) that interdigitate with upward projections of the dermis called dermal papillae. In your slides, the papillary layer of the dermis is only evident by a difference in the coarseness of the collagen bundles, they are finer but are also more tightly packed. Distinguish the papillary layer from the reticular layer. The interface between the dermis and hypodermis is quite distinct in the scalp because of the amount of adipose in the superficial fascia. Penetrating from the epidermis into the hypodermis are a large number of pilosebaceous follicles comprised of hair and sebaceous glands. Scan the section to get the best (i.e., most complete sagittal) view of a hair follicle. Since the hairs run so obliquely, it is difficult to see a complete follicle, so study several sections and generate mental image of the complete structure. At the base of the follicle, distinguish the dermal papilla that induces growth of the hair in the overlying keratinocytes. The epidermis descends into the dermis as a stratified epithelium that comprises the external root sheath. Near the apical end of this tubular “gland”, the epithelium bulges and forms alveolar outpocketings that become the sebaceous glands. Down the epithelial sleeve near the base of the follicle, the hair evolves from epidermal cells that lie above the dermal papilla. The cells in this vicinity are frequently loaded with melanin from melanocytes in the epidermis above the dermal papilla. The center of the hair is composed of large polygonal epidermal cells that provide for the medulla. Medullary cells and surface epidermal cells contain a soft keratin. Keratinization of the hair occurs a short distance up the shaft from the papilla. The epidermis cells surrounding the medulla form the densely packed, spindle-shaped cells of the thicker cortex. Cortex cells synthesize hard keratin. The outer most layer of the hair is comprised of epidermal cells that form the cuticle. Near the base of the follicle the cuticle cells form a simple cuboidal sleeve around the cortex. As you ascend the hair the cutical cells become more columnar in appearance, with their long axes perpendicular to the shaft. Further up the shaft the cuticle cells reorganize and form heavily keratinized shingle-like cells that are oriented with their long axes aligned with that of the hair. The cuticle, the last of the hair layers to differentiate, creates a hydrophobic barrier which resists infiltration of the histological embedding media. Consequently, in many sections the cortex and medullary regions of the hair “fall out” of the sections during preparation. The epithelial cells surrounding the hair are the root sheath layers. The external root sheath runs from the skin’s surface to the dermal papilla. The internal root sheath only extends from the base to about half way up the shaft where the cells degenerate and create a space between the hair and surrounding external sheath. The dermis surrounding the root sheath forms a thin dense connective tissue sheath. Bundles of smooth muscle, the arrector pili muscles, extend from the upper dermis to the connective tissue sheath near the middle of the follicle. Contraction of these muscles causes the hair to stand more vertically in relation to the skin’s surface. This process produces the infamous “goose bumps’’ which arise in regard to either fluctuations in environmental temperatures or emotional rushes. The latter may be elicited by extremes in inputs that range from those pleasures derived from a sensual caress to those of uncontrollable fear as might occur in the taking of an histology exam. Have you realized yet that the physiological experiences of “rushes” are the same despite whether they are derived from pleasure or from pain. The sebaceous glands are simple alveoli that are lined squamous keratinocytes. As the cells divide they stratify and enlarge, increasing the diameter of the gland. As the cells mature toward the center of the gland they acquire large sebum inclusions (lipids, which are washed out during preparation). Near the center of the alveoli, the cells degenerate releasing a mixture of sebum and cytoplasm. This is an example of holocrine secretion. Interspersed among the hair follicles are sweat glands. They are fewer in number to those present in thick skin. ln this preparation the cells within the secretory region are better preserved than in the previous slide. Staining differences, though close, can be used to distinguish dark (mucoid) cells from the clear (transporting) cells. The eosinophilic layer at the base of the epithelium in the secretory region primarily reflects the cytoplasm of flattened myoepithelial cells. Which side of the basement membrane are they on? Identify and check-off each of the following: Epidermis Hypodermis Hair Melanin Hair cortex External root sheath Arrector Pili muscle Sweat gland secretory unit Dermis Pilosebaceous follicle Dermal Papilla Hair medulla Hair cuticle Dermal sheath around hair Sebaceous gland Sweat gland duct