View/Open - Hasanuddin University
advertisement

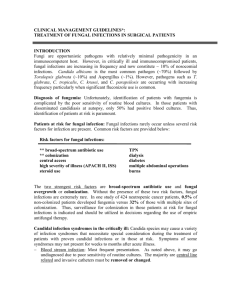
IS THERE ANY CHANGE IN THE SPECTRUM OF CANDIDIASIS DUE TO THE RISE AND EPIDEMIOLOGICAL SHIFTS OF NON-ALBICANS CANDIDA spp? drg. Erni Marlina, Sp.PM*, drg. Ali Yusran, M.Kes, drg. Zohra Nazaruddin Abstract Background : angular cheilitis most commonly caused by secondary infection of candida mainly candida albicans, bacteria ie s.aureus, or mixed infection of both microorganism. Recently some reports suggest that a shift has rise in the distribution of infection with non-albicans candida spp. Aim : to identify candida spp in isolate obtained from angular cheilitis. Material and method : 30 angular cheilitis patients age range 6-12 years. Lesion occur 2 – 14 days before. Angular cheilitis swab with cotton roll then put in Stuart Transport Medium. After 48 hours incubation isolate carried to sabouroud dextores agar and nutrient agar for next 48 hours incubation. Then isolate carried to Manitol Salt Agar (MSA) for next incubation. If there were not any growth,it suggested as candida spp, and if there were, it suggested as staphylococcus. For species identification biochemical test was performed for bacteria and microscopic examination for candida morphology. Result and conclusion : s.aureus was isolated from 10 (33,3%), s.epidermidis 8 (26,6%), s.saproficus 5 (16,6%), streptococcus spp 3 (10%) , negative basil 3 (10%), and candida tropicalis 1 (3,3%) This interesting result show that there was a shift in pathogens of non-albicans candida which must be considered in therapeutic for candidiasis. Key words : candida albians, non-albicans candida, sabouroud broth. Background Angular cheilitis most commonly caused by secondary infection of candida mainly candida albicans, bacteria ie s.aureus, or mixed infection of both microorganism. Ohman and partner, in 1986 performed clinical microbiology research for angular cheilitis that show result 20% of candidiasis, 20% bacteria infection and 60% mixed infection. 1 Bacteria identified was streptococcus aureus, and Candida albicans being the most prevalent.2 Recently some reports suggest that a shift has rise in the distribution of infection with non-albicans candida spp.2-7 This has been rise interest because some non candida albicans species infection is highly mortality and resistance with antifungi.2,8 Based on our clinical therapy that use miconazole as gold standart for angular cheilitis therapy than it is advisable to determine the distribution and the pattern of epidemiological shift in angular cheilitis. Therefore, we try to performed a research which purpose to examine the distribution and to draw epidemiological shift of candida species in angular cheilitis lesion to provide some insight into the management of this lesion. Material and method This study performed on 30 angular cheilitis patients age range 6-12 years. This patients selected from all individual attended to Hasanuddin University Dental Hospital at department Oral Medicine from February to October 2011. All this patient unremarkable health histories from anamnesis, and clinical sign and excluded angular cheilitis because of denture wearing. The patient were enrolled after providing informed verbal and written concent. For microbiology examination, the modification of Kleinegger et al was used. Briefly angular cheilitis swab with cotton roll then put in Stuart Transport Medium. After 48 hours incubation isolate carried to sabouroud dextores agar and nutrient agar for next 48 hours incubation. Then isolate carried to Manitol Salt Agar (MSA) for next incubation. If there were not any growth,it suggested as candida spp, and if there were, it suggested as staphylococcus. For species identification biochemical test was performed for bacteria and microscopic examination for candida morphology. Statistical method used manual tabulation to draw distribution and epidemiological pattern of microorganism isolated from the lesion. Result Table 1 lists the frequency of microorganism include Candida species which were isolated from 30 angular cheilitis patients. S.aureus was isolated from 10 (33,3%) samples, s.epidermidis 8 (26,6%), s.saproficus 5 (16,6%), streptococcus spp 3 (10%) , negative basil 3 (10%), and candida tropicalis 1 (3,3%). Discussion Angular cheilitis most commonly caused by secondary infection of candida. In a research by Ohman and partner reported the microorganism found in angular cheilitis was 20% infected by candidiasis, 20% infected by bacteria, and 60% mixed infection from both microorganism. 1 Streptococcus aureus dominated the bacteria species, and candida albicans prevalent for Candida infection. The result of the present study is not accordance with the above reports which showed that 96% angular cheilitis infected by bacteria even that this research concordance for bacteria species isolated that is s.aureu. But it show a shift in epidemiological pattern which only 10 sampel (33,3%) s.aureus found. For candidiasis, Candida albicans was the prevalent fungi infected to human. Even some reports suggest that a shift has rise in the distribution of infection wit non-albicans candida spp.2-7 As in report of Li et al, that C.glabrata is increasingly implicated in human infection and should got an attention because of the mortality rate is high.2 This research accordance with review by Capoor et al in 2005 in fungi infected human which report C.tropicalis (48%) as the prominence Candida spp in his research. This report only found 22,5% C.albicans which rank as a third Candida Spp, after C. Tropicalis and C. Parapsilopsis. This report is ini agreement with several published reports from India and abroad. 7 In our small but prosective study, interesting result has found where angular cheilitis isolated microorganisme predominance by bacteria Spp. mainly s.aureus and only one Candida Spp. that is C.tropicalis which by some report emerging as a pathogen Candida. The differences between the presenter sult and thoe of other tudies may be due to the variation in the clinical observations, number and age ranges of subjects, geographic locations, the eesign studies and sampling techniques. But, it is still a very worth result that have to considering in evidence based therapeutic, since in our dental hospital angular cheilitis still manage by using anti-fungi. References 1. Zunt LS., Oral Candidiasis : diagnosis and treatment. The journal of practical hygiene .2000.9(10). 2. Li L, Redding S, Bagtzoglou-AD., Candida glabrata,an emerging oral oportunistic pathogen. J.Dent.Res.2007. 86 (3) : 204-215. 3. Kadir T, Uygun B, Akyuz S., Prevalence of candida species in Turkih Children : Relationhip between dietary in take and carriage. J. Archives of Oral Biology.2005. 50 : 33-37. 4. Katirace F, Khosravi AR, Khalaj V, Hajiabdolbagi M, Khaksar A, Rasoolinejad M, Yekaninejad M.S., Oropharyngeal candidiasis and oral yeast colonization in Iranian Human Immunodeficiency Virus positif patients. J. De Mycologie Medicale. 2009.214-217. 5. Mieller FT, Jabra-Rizk MA, Baqui AAMA, Kelley JI, Meeks VI, Merz WG, et al., Oral candida dublinensis as a clinically important species in HIV positive patients in the limited status. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:573-80 6. Dimopulous G, Ntziora F, Rachitis G, Armaganidis A, Falagas ME., Candida albicans versus non-albicans intensive care unit acquired bloodstream infections : Diffrences in risk factors and outcome. Anesth Analg. 2008 : 106 : 523-529. 7. Capoor MR, Nair D, Deb Monorama, Verma PK, Srivastava L, Anggarwal P., Emergences of non-albicans candida species and antifungal resistence in tertiary care hospital., J.Inf. Dis.2005. 58.344-348. 8. Gomez-Lopes A, Pan D, Cuesta I, Izquierdo AA, Rodriquez-Tudela JL, Cuenca-Eterella M., Molecular identification and susceptibility profile in vitro of the emerging pathogen candida. Diagnostic Microbiology and Inf.Dis. 2010,66,116-119.



![medicine18_11[^]](http://s3.studylib.net/store/data/007210290_1-19e9d9cbcdcc24ec73570d20e7751302-300x300.png)