Mycology - BMC Dentists 2011

Mycology
Introduction
Mycology is study of fungi and fugal infection.
Fungi are define as Eukaryotic organism, consisting of microscopic branching filaments called hyphae carrying spores.
Or as unicellular yeast.
Fungi are found every where as saprophytes , may found in soil, vegetable, water and disseminated in air or as pathogenic .
Classification of fungi
(1) Morphological classification
1- Filamentous form.
2-Yeast.
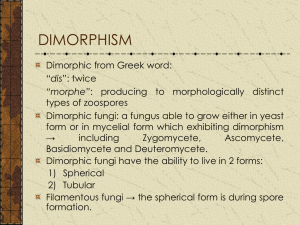
3- Dimorphic.
(2) Clinical classification
1- Superficial mycosis.
2- Subcutaneous mycosis.
3- Systemic mycosis.
4- Mycotoxicosis .
Yeast Identification
Candida is present as normal flora in the mouth, GIT and vagina.
Species include: o o o o o o
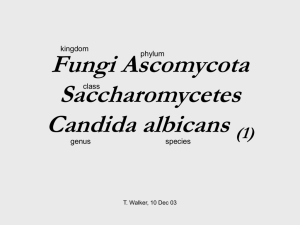
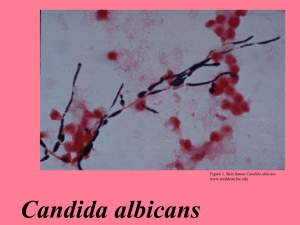
Candida albicans (the most important)
Candida tropicalis
Candida krusei
Candida parapsilosis
Candida glabrata
Candida dubliniensis
3)
4)
5)
2)
1)
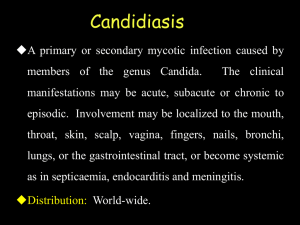
Diseases
Oral thrush or moniliasis (patches of creamy white exudate that cover the mucous membrane of the mouth).
o
Vulvovaginal moniliasis: itching and cheese appearing vaginal discharge. It occurs in females with:
Prolonged use of broad spectrum antibiotics
(superinfection) o o
Contraceptive pills
Pregnancy
Rash in the skin folds
Diaper rash.
Paronychia of the nails (thickening and loss of the nails).
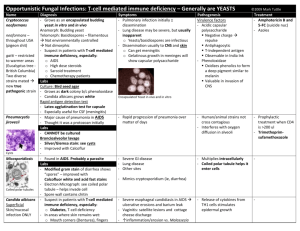
In immunocompromised individuals:
1)
2)
3)
Esophageal thrush.
Chronic mucocutaneous candidiasis.
Systemic or disseminated candidiasis (even to the eye).
Laboratory diagnosis of Candida albicans
Specimen: It is according to the site of the lesion i.e. exudates, vaginal, oral swab, tissue, nail scrap, blood.
1.
Microscopic Examination
1- Stained smears: With Gram stain, yeast cells are seen as Gram positive, oval budding yeast cells attached to pseudohyphae.
2- 40% KOH: budding yeast, pseudohyphae.
2. Culture: Grow on Sabouraud’s dextrose agar (SDA) at 37 0 C.
Identification of candida on the plate is done by: a.
Morphology: Soft cream colored colonies with yeasty odor.
b.
Gram film: Gram positive oval budding yeast cells.
3.
Biochemical reactions:
To differentiate between Candida albicans and other species.
a.
Germ tube test: Candida albicans forms germ tube when incubated in serum for 1 – 2 hour at 37 0 C.
b.
Chlamydospore formation: Candida albicans forms chlamydospores on corn meal.
c.
Sugar fermentation: Candida albicans ferment glucose and maltose with acid and gas production.
d.
Inoculation of the yeast on chromogenic agar:
Each candida specie produces a different color on this medium.
Germ tube Chlamydospores
CHROMagar
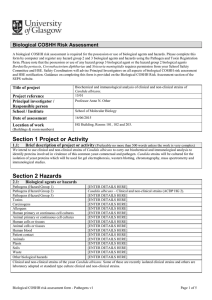
GTT: Germ tube test:
(a) Inoculate 3ml of horse serum & incubate for 2-3 hrs.
(b) Put drop of preparation on slide & screen with 10X , 40X for tube like structure i.e. germ tube.
GTT positive > production of germ tubes in plasma after 3 hours incubation at 37 0 C . C. albicans.
Germ tube negative > Budding blastoconidia only are seen.
other Candida species.
Procedure:
Using clean, dry and sterile test tubes.
Using a Pasteur pipette, dispense 3 drops of fresh pooled human serum into the tubes.
Serum can be obtained from the Serology lab.
With a sterile wooden applicator stick, lightly touch a yeast colony and place the stick into the serum.
Suspend the yeast in the serum. Discard the stick in a discard container.
Incubate the test at 35 o C for 2.5-3 hours.
Place a drop of the suspension on a clean microscope slide.
Place a clean cover glass over the suspension and then examine it with a microscope using the low power objective.
Use the high power objective to confirm the presence or absence of germ tubes.
Read controls and record results.
If time is not allowed to read and record the test results add a drop of 10% formalin/formaldehyde to each tube, seal the top with parafilm, and store at 2-4 in the refrigerator.
A: +ve GTT B: -ve GTT