Fungal Infections in the ICU
advertisement

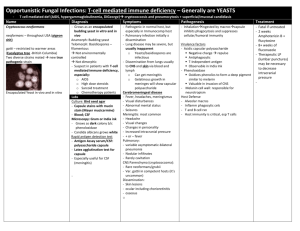
Invasive Fungal Infections in Critically Ill Patients Abhay Dhand M.D. Director, Transplant Infectious Diseases Westchester Medical Center, Valhalla NY Invasive Fungal Infections in Critically Ill Patients Objectives: 1. To understand the epidemiology and risk factors for invasive fungal infections in critically ill patients. 2. To familiarize with various investigative modalities for diagnosis of invasive fungal infections. 3. To understand the available anti-fungal therapies and their optimal use in patients in ICU setting. 4. To learn important drug interactions between anti-fungal therapies and commonly used drugs in ICU setting. Incidence of Fatal Invasive Mycoses in USA Rate per 100,000 Population 0.6 Candidiasis 0.4 0.2 Aspergillosis 0.0 1981 1986 1991 Year Mc Neil et al 2001 Clin Infect Dis 33;641 1996 Focus on Candidiasis • Invasive Candida infections: – 4th most common nosocomial bloodstream infection in the USA with mortality approaching 40% in line related candidemia* Pathogen Coagulase-negative staphylococci Staphylococcus aureus Enterococci Candida species No. of Isolates Incidence (%) 3908 1928 1354 934 31.9 15.7 11.1 7.6 *In a 3-year (1995–1998) surveillance study of 49 hospitals in the United States. Adapted from Edmond MB et al Clin Infect Dis 1999;29:239–244; Andriole VT J Antimicrob Chemother 1999;44:151–162; Uzun O, Anaissie EJ Ann Oncol 2000;11:1517–1521. Species of Candida Most Commonly Isolated in Bloodstream Infections In an international surveillance study 1997-1998: C. tropicalis 8% C. krusei 2% other Candida spp 5% C. albicans 54% C. parapsilosis 15% C. glabrata 16% Adapted from Pfaller MA et al and The SENTRY Participant Group Antimicrob Agents Chemother 2000;44:747–751. Since then increase in Candida spp. with higher incidence of fluconazole resistance. Snydman DR. 2003. Chest 123(Suppl 5):500S-503S). Garbino J. et al. 2002. Medicine;81:425-433. Invasive Candidiasis in the ICU Common in the ICU (9.8/1000 admissions) With high morbidity (increased LOS ~22 days) & mortality (~ 30-40%) • Difficult to diagnose (cultures positive in only ~ 50%). • We can define ICU risk factors for candidiasis and target the population at highest risk with empiric Rx. • Recent increase in Candida spp. resistant to fluconazole. Eur J Clin Microbiol Infect Dis. 2004:23; 739-744. Risk for Invasive Mycosis •Non-Neutropenic patients: related to barrier breakdown, change in colonization. – – – – – – – – Acute renal failure (RR 4.2) Parenteral nutrition with intralipid (RR 3.6) Prior surgery specially GI (RR 7.3) Indwelling central line ? Triple lumen (RR 5.4) Broad spectrum antibiotics Diabetes Burns Mechanical Ventilation Adapted from Blumberg HM et al, and the NEMIS Study Group Clin Infect Dis 2001;33:177–186; Garber G Drugs 2001; 61(suppl 1):1–12. Risk for Invasive Mycosis • Neutropenic patients: risks related to non- neutropenic patients plus immune cell suppression and underlying malignancy. – Steroids • Severe immunosuppression: BMT or SOT Adapted from Blumberg HM et al, and the NEMIS Study Group Clin Infect Dis 2001;33:177–186; Garber G Drugs 2001; 61(suppl 1):1–12. Major Risk Factors: Candidiasis Prior antibiotic use, Central venous catheters, Total parenteral nutrition, Major surgery (abdominal) within one week, Steroids, Immunosuppression. Intensive care unit length of stay: the rate of infections rising rapidly after 7-10 days Dimopoulos G, et al. Candidemia in immunocompromised and immunocompetent critically ill patients: a prospective comparative study. Eur J Clin Microbiol Infect Dis. 2007 Candidemia in Non-neutropenic ICU Patients Risk Factors for Non-albicans Candida Spp. Nationwide Australian prospective cohort study. Patients with ICU-acquired candidemia over 3 yr. C albicans 62%, C glabrata 18%, C parasilopsis 8%, C tropicalis 6%, C krusei 4%, Other Candida spp. 2% Independent risk factors for non-albicans candida or potentially fluconazole-resistant species: Age (OR 1.3), Recent GI surgery (OR 2.9), Prior exposure to systemic antifungal agents (OR 4.6) especially fluconazole (OR 5.7). . EG Playford et al. Crit. Care Med. 2008; 36(7): 2034-2039 Risk Factor Selection Malignancy, Diabetes, Renal disease, Steroids, TPN, Burns Fever Antibiotics Selection of Candida and Colonization Skin or mucosal damage Instrumention CVC GI surgery Infection: Invasive Candidiasis Pathogens Responsible for Invasive Fungal Infections in HSCT and SOT Recipients* Based on data on 886 invasive fungal infections; 71% of infections were caused by Candida or Aspergillus spp 29% 42% Candida spp Aspergillus spp Other fungi 29% *Pooled data from infections in HSCT and SOT recipients. HSCT indicates hematopoietic stem cell transplant; SOT, solid organ transplant. Pappas PG, et al. In: Program and Abstracts of the 42nd Annual Meeting of the Infectious Diseases Society of America. 2004. Abstract 671. Candidiasis in SOT Recipients Analysis of data from 19,237 HSCT and SOT recipients from 25 centers in the United States from 2001 to 2003 SOT recipients Incidence of invasive candidiasis, % 2.6 • Based on pooled data for both patient populations, the investigator-determined mortality attributable to invasive candidiasis was 24% ( overall mortality of 40%) HSCT indicates hematopoietic stem cell transplant; SOT, solid organ transplant. Andes D, et al. ICAAC 2004. Abstract M-1014. Invasive Candida Infections Reported in Various Transplant Types* 60 Prevalence, % 50 42 38 40 30 17 20 12 8 10 0 Liver Kidney Pancreas *Numbers reflect data collected by TRANSNET from 2001 to 2004. Lung Heart Andes D, et al. ICAAC 2004. Abstract M-1014. Invasive Mycosis MICU or SICU Oncology Candidiasis Loss of Barrier immunity SOT or BMT Aspergillosis Decreasing immunity Loss of barrier plus cellular immunity Aspergillosis in SOT Recipients Analysis of interim data from 4110 SOT procedures from 19 centers in the United States from March 2001 to December 2002 Incidence* Mortality† Heart 3 (0.8) 2 (66.7) Kidney 3 (0.1) 2 (66.7) Liver 3 (0.3) 1 (33.3) Lung 10 (3.5) 2 (20.0) Other 1 (0.4) 0 Transplant type, n (%) *Weighted aggregate incidence after 12 months. †Three months after diagnosis of aspergillosis. SOT indicates solid organ transplant. Morgan J, et al. Med Mycol. 2005;43(suppl 1):S49-S58. Case-fatality Rate, %* Aspergillosis Is Associated With a High Rate of Mortality in Many Patient Populations 100 80 60 40 20 0 Leukemia/ Bone Lymphoma Marrow/ HSCT Kidney Lung/Lung Liver Transplant and Heart Transplant Transplant AIDS/ HIV *Determined from 1941 patients from 50 studies published between 1995 and 1999. Lin SJ, et al. Clin Infect Dis. 2001;32:358-366. HSCT indicates hematopoietic stem cell transplant. Zygomycosis • Vulnerable populations – Malignancy – Bone marrow transplantation – Solid organ transplantation • • • • • Corticosteroid exposure GvHD CMV reactivity Neutropenia Uncontrolled Diabetes mellitus – Initial presentation with sinusitis – Occurrence as breakthrough prior Voriconazole prophylaxis • 56% mortality others… Fusarium sp. Penicillium sp. Trichosporon sp. Marr, CID 2002 Steinbach, J Infect 2004 Roden, et al. Clin Inf Dis 2005;41:634-53. Kontoyiannis et al. JID, 2005; 191:1350-60. Siwek et al. CID 2004; 39:584-87. Laboratory Diagnosis: Candida • Microbiology methods: – Recovery of Candida species from sterile sites (ex. blood, peritoneal fluid) is diagnostic of IC and recovery from multiple non-sterile sites is highly suggestive of IC in the atrisk patient. – Blood culture is positive in less than 50% of patients with autopsy proven IC. • Molecular methods: – early identification ex PNA FISH • Serological methods: – early diagnosis ex. 1,3 beta D glucan assay. • Histopatholgic methods. Clinical Diagnosis: Candida The clinical manifestations of IC are nonspecific, but may include: • Fever and progressive sepsis with multi-organ failure despite antibiotics. • Invasive candidiasis (IC) related cutaneous lesions. – Macronodular rash frequently confused with drug allergies. A biopsy of the deeper layers of skin particularly the vascularized areas and the dermis is important. • Ophthalmic lesions (Candida endophthalmitis). – A fundoscopic evaluation for the presence of Candida endophthalmitis should be performed in patients with candidemia. Serological Methods ? early aid in empiric therapy decision making • Plasma beta-D-glucan, a cell wall constituent of fungi, was measured before starting antifungal therapy empirically on postoperative patients, colonized with candida & having risk factors for candida infection. • 47% of those with positive test responded to Rx but 9% of those negative responded (p<.01) (OR= 13). • Number of sites colonized with candida also predicted response. Colonization at ≥ 3 sites vs. 1 site (p=0.03) (OR=7.57). • In postoperative patients colonized with candida, & with fever despite antibiotics a beta-D-glucan assay was useful for deciding whether to start empiric therapy. Takesue Y et al. World J Surg. 2004; 28(6): 625-30. TREATMENT “I don’t want you to make the wrong mistake” —Yogi Berra Candidemia: Who do we treat? • Answer: Essentially everybody – Even a single +BC can be relevant – Concerned about hematogenous seeding • Spread to the eye – Can cause blindness – Lesions are common! – 26-29% rate Catheter Exchange? Yes! • Lots of consistent data – Without catheter removal, 82% had persistent infection • Lecciones, Clin Infect Dis 1992;14:875-883 – Shortened duration of fungemia from 5.6 to 2.6 days • P < 0.001 (Rex, Clin Infect Dis 1995;21:994-996) – Reduced mortality: 41% to 21% • P < 0.001 (Nguyen, Arch Intern Med 1995;155:2429-2435) • Especially true for C. parapsilosis – Very strong link with catheters • Kojic, Clin Microbiol Rev 2004;17:255-267 Candiduria • Asymptomatic candiduria – No treatment unless high-risk dissemination (AIII). – Focus on elimination of predisposing factors. (BIII). • High risk for dissemination – Urologic manipulations (BIII) • Use short course fluconazole or even amphotericin B – Neutropenic patients and low birth weight infants • Treat as for invasive candidiasis. • Consider imaging kidneys/collecting system (BIII) Can we wait for the blood culture results in candidemia? • Retrospective cohort analysis 1/2001-12/2004: N=157 patients with candidemia. • Delay in empiric Rx of candidemia till after blood cultures turn positive resulted in higher mortality. • Start of anti-fungal Rx >12 hrs of drawing a blood culture that turns positive had AOR= 2.09 for mortality, p=0.018. Morrel M et al. 2005. Antimicrob Agents Chemother. 49(9):3640-5 27 Mortality vs. number of days to initiate fluconazole after culture done 45 Variable 40 Mortality, % 35 30 25 20 15 Multivariate model independent risk factors for hospital mortality 17% Odds Ratio P Value Time to start fluconazole 1.50 0.014 APACHE II 1.13 <0.001 Up to 70% patients did not receive antifungals within 24 hours + blood Culture 10 5 0 0 1 2 3+ Days Garey KW et al. Clin Infect Dis. 2006;43:25. Therapy of IC in the ICU • A definitive diagnosis of IC may be delayed when the clinical and laboratory tools readily available to clinicians are used to assess patients for Candida infection. • A delay in diagnosis will unfortunately result in a delay in initiation of antifungal therapy, which is associated with increased mortality*. • Therefore, in the patient with suspected Candida infection, treatment may need to be initiated on the basis of individual patient factors before a definitive diagnosis is made. *Morrel M et al. 2005. Antimicrob Agents Chemother. 49(9): 3640-5. *Garey K et al. 2006. Clin Infect Dis. 43: 25-31. Aspergillosis Aspergillus species are found in : – – – – – – – – Soil Air; spores may be inhaled Water / storage tanks in hospitals etc Food Compost and decaying vegetation Fire proofing materials Bedding, pillows Ventilation and air conditioning systems – Computer fans Aspergillus spores Development of Aspergillosis INHALATION COLONIZATION Pulse steroid OKT3/Antilymphocyte therapy Antibiotic use Organ failure Re-transplantation Thrombocytopenia INFECTION DISSEMINATION Environmental exposure Construction Invasive aspergillosis in solid-organ transplantation: diagnosis • Radiology: chest X-ray and CT: no halo sign • Microbiology – Respiratory secretions: BAL/biopsy • Direct microscopy • culture – Serological surveillance • ELISA for galactomannan • PCR Ergin et al. Transplant International 2003; 16: 280-286 Strategies for dealing with systemic fungal infectious disease Optimal antifungal management? Temperature (°C) Treatment 4 1 40 Prophylaxis Empirical Pre-emptive Specific 39 38 37 36 PCR + Galactomannan+ Culture + Tissue + 10 0 Granulocytes Disease likelihood Remote Possible Probable disease Proven 1 0.1 -14 -7 0 7 14 21 28 35 Days after transplant 42 49 56 63 Site of Action of Selected Anti-fungal Agents Cell membrane Polyenes AmB (sterols) Azoles Fluconazole (CYP450) Cell wall Echinocandins Caspofungin (Glucan synthesis inhibitors) Adapted from Andriole VT J Antimicrob Chemother 1999;44:151–162; Graybill JR et al Antimicrob Agents Chemother 1997;41:1775–1777; Groll AH, Walsh TJ Expert Opin Invest Drugs 2001;10(8):1545– 1558.