Immunity Regulation
advertisement
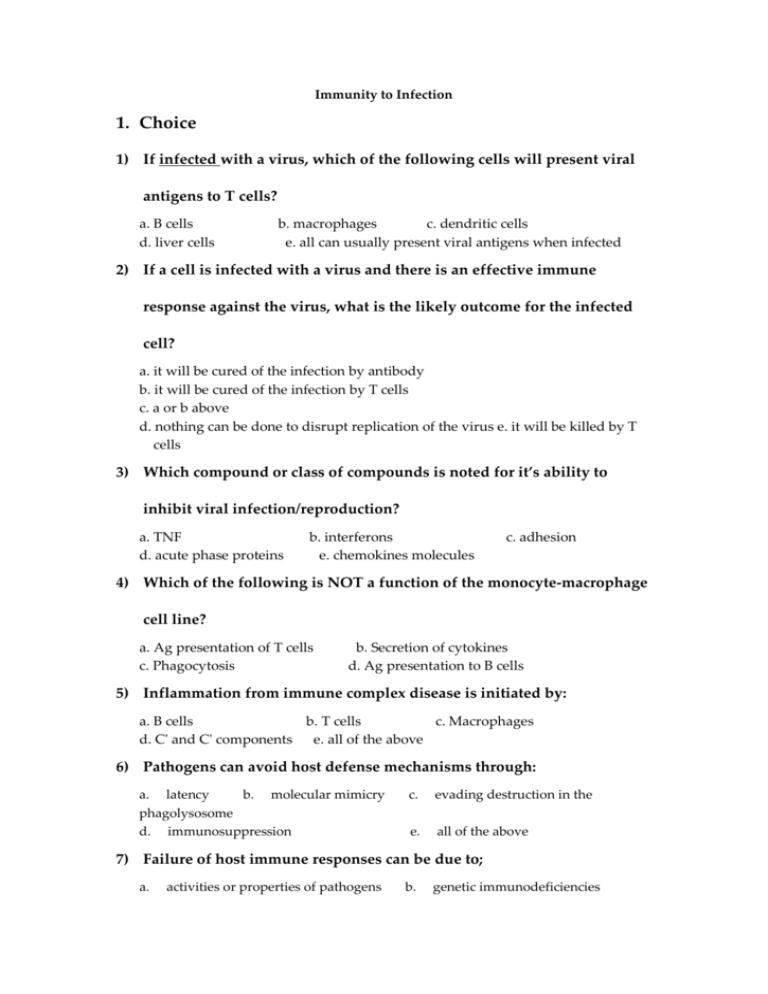
Immunity to Infection 1. Choice 1) If infected with a virus, which of the following cells will present viral antigens to T cells? a. B cells d. liver cells b. macrophages c. dendritic cells e. all can usually present viral antigens when infected 2) If a cell is infected with a virus and there is an effective immune response against the virus, what is the likely outcome for the infected cell? a. it will be cured of the infection by antibody b. it will be cured of the infection by T cells c. a or b above d. nothing can be done to disrupt replication of the virus e. it will be killed by T cells 3) Which compound or class of compounds is noted for it’s ability to inhibit viral infection/reproduction? a. TNF d. acute phase proteins b. interferons e. chemokines molecules c. adhesion 4) Which of the following is NOT a function of the monocyte-macrophage cell line? a. Ag presentation of T cells c. Phagocytosis b. Secretion of cytokines d. Ag presentation to B cells 5) Inflammation from immune complex disease is initiated by: a. B cells b. T cells c. Macrophages d. C' and C' components e. all of the above 6) Pathogens can avoid host defense mechanisms through: a. latency b. molecular mimicry phagolysosome d. immunosuppression c. evading destruction in the e. all of the above 7) Failure of host immune responses can be due to; a. activities or properties of pathogens b. genetic immunodeficiencies c. e. developmental abnormalities all of the above d. specific infectious agents 8) Transplants are never rejected if the donor and host are: a. identical at all genes (ie identical twins) b. identical at class I MHC molecules c. identical at class II MHC molecules d. identical at both class I and class II MHC molecules e. NONE of the above 9) A patient is seen in immunology clinic because of recurrent infections with pyogenic bacteria. It has been observed that neutrophils and macrophages accumulate at the area of infection, but are unable to kill encapsulated bacteria. One of the individuals involved in treating this patient performed a test to determine whether the phagocytes could ingest opsonized bacteria normally. The patient's cells were able to ingest Ab coated bacteria and the patient had normal serum Ig levels. Therefore, lack of killing is related to: a. lack of IgG b. lack of FcgR on the patient's macrophages c. lack of ability to kill in a phagolysosome or form phagolysosomes d. lack of C' components e. all of the above 10) Both bacteria and viruses have the ability to be intracellular pathogens. Which of the following is true concerning the immune response to intracellular organisms? a. Ab is effective for clearing out the infection b. Th1 and Tc effector cells are required for recovery depending on the type of infection c. only innate immune responses are necessary d. Th2 effector cells enhance clearing of the organisms e. all of the above 11) Inflammatory responses are non-specific, however the initiating events of inflammation may be due to tissue damage or Th1 cytokine release. Which of the following statements are true concerning Th1 induced inflammatory responses? a. they occur in response to intravesicular pathogens b. they are type IV hypersensitivity responses c. Th1cells respond to Ags presented on macrophages and endothelial cells d. in these responses, macrophages are activated by cytokines and CD40-CD40 ligand interactions e. all of the above 12) Innate immunity is nonspecific, however it interacts with specific immunity during the immune response. At which of the following stages of an immune response do specific and non-specific components interact? a. activation of T cell effector funtions at the site of infection b. direct stimulation of Ab production c. activation of naive T cells to effector T cells d. a and c e. all of the above 13) Inflammatory responses are non-specific, however the initiating events of inflammation may be due to tissue damage or Th1 cytokine release. Which of the following statements are true concerning Th1 induced inflammatory responses? a. the cytokines released by Th1 effector cells make endothelial cells sticky b. the cytokines released by Th1 effector cells do not activate macrophages c. Th1 effector cells cannot activate additional Th1 cells d. Abs are an important component of the response e. all of the above 14) Macrophages which lack receptors for CR1 and Fcg are: a. unable to phagocytize opsonized bacteria c. activated killer cells d. dendritic cells b. more efficient at phagocytosis e. all of the above 15) Which of the following is NOT characteristic of the early stages of a localized inflammatory response? a. attack by cytotoxic T cells b. release of histamine c. increased permeability of capillaries d. dilation of blood vessels 2. Question 1. Viruses have been shown to evade every aspect of innate and adaptive immunity. Viruses which can evade the host’s immune system to establish a chronic, persistent infection have a selective advantage over those viruses which are not able to evade the immune system…...Three examples of viral immune evasion strategies are described below. For each of the three strategies, please state whether virally-infected cells would be killed by i) CTLs and/or ii) NK cells, and explain why target cell killing would or would not occur (1 sentence) a. HIV taken from HLA-A2 positive individuals often harbors mutations in the sole viral epitope presented by HLA-A2, resulting in loss of binding to HLA-A2. i) HLA-A2-restricted CTLs ii) NK cells b.Human cytomegalovirus (HCMV) encodes a protein called US3 that binds to MHC Class I molecules and retains them in the ER, so that they never get presented on the cell surface. i) CTLs ii) NK cells c. Poxviruses encode a protein called crmA, which can inhibit caspases, which are proteins in the apoptosis cascade downstream of granzymes and Fas. i) CTLs ii) NK cellsd. Other viruses have strategies to evade MHC Class II presentation, and therefore CD4+ T cell activation. Given that eradication of the infected cell requires MHC Class I presentation, give two reasons why would it be advantageous for these viruses to inhibit CD4+ T cell activation. 2. Bacterial killing mechanisms that operate within neutrophils Immunity Regulation and Transplantation Immunology 1. "Simple True-False" type. (For each numbered statement, mark "a" if true, "b" if false.) 1) Most nonclassical MHC genes were discovered through restriction mapping techniques. 2) All genes in the MHC of a species code for histocompatibility antigens. 2. Choice 1) Which statement about regulation of expression of MHC molecules is incorrect? a. INF-( up-regulates expression of class II molecules on non-traditional antigen-presenting cells through induction of the transactivator CIITA. b. induction and repression mechanisms of regulation of expression of MHC molecules are reflected in the cellular distribution and density of expression on different cell types. c. cytomegalovirus down-regulates expression of class I molecules through production of a viral protein that binds β2m. d. several promoter motifs of class II genes are recognized by transcription factors such as CIITA and RFX; defects in these transcription factors may be responsible for some forms of “bare lymphocyte syndrome”. e. the anti-inflammatory effects of corticosteroids and prostaglandins may be associated with there ability to up-regulate expression of class II molecules. 2) Hyperacute graft rejection occurs when; a. the donor has made an immune response against the host b. the host makes an immune response to a newly grafted tissue c. the host has preformed Ab against the grafted tissue d. the host makes a low level immune response to a graft e. all of the above 3) Allograft rejection occurs when a host and graft are: a. identical at all the genes b. differ in genes at the MHC locus c. from identical twins d. a and c e. all of the above 4) Which of the following is (are) protein(s) that kill target cell by punching holes in its membranes? a. perforins d. a and c b. cytotoxins c. membrane attactk complex of C' e. all of the above 5) 6) 3. Question 1) Give a critique on factors that influence graft rejection. 2) Review the experimental evidence for immunological tolerance to self. 3) What are the transplantation rejections? How are they classified? What are the possible mechanisms of these rejections? 4) Outline the mechanisms that generate and maintain tolerance in T cells. Discuss how defects in (a) central and (b) peripheral T cell tolerance may lead to disease. 5) What is the evidence that supports the importance of tissue matching of unrelated cadaveric transplant donor-recipient pairs? 6) What are the mechanisms of solid organ graft rejection and how might tolerance be achieved? 7) How to match the donor/recipient for renal transplantation? 8) Compare and contrast antigen processing and presentation by direct and indirect pathways with in transplantation. 9) The mechanism of peripheral and central tolerance in mature T cells 10) Describe the balance between in Th1 and Th2. 11) Write short notes on the physiological function of each of the following molecules and their relevance in diseases of the immune system: a. Foxp3 b. CTLA-4 c. CD80/CD86 d. The character T regulatory cells e. Anergy f. GVHR g. donor Tumor Immunology 1. Choice 1) Immunomodulation of host immune responses can: a. be used to increase the immune response to cancers b. stimulate Ab production with vaccines c. inhibit responses grafted tissue d. a and c e. all of above 2. Question 1) 2) 3) 4) 5) 6) Tumor specific antigen Tumor associated antigen How the tumor antigens are processed and present by tumor cells? Review the contribution of the host anti-tumor mechanism. How the tumor to escape the host anti-tumor mechanism. Review the strategy of immunotherapy for tumor.

![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)