adult soap note
advertisement
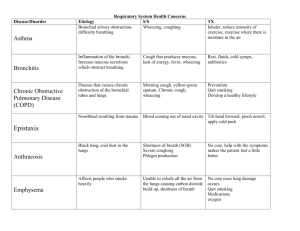
SUBJECTIVE DATA (S): IDENTIFYING DATA: Initials: G.B. Age: 61 years Race: Caucasian Gender: Female Marital Status: Married CHIEF COMPLAINT (CC): Patient complains of “cough and congestion for 2 weeks.” HISTORY OF PRESENT ILLNESS (HPI): Patient c/o dry cough x 2 weeks. Patient states she just got back from a cruise and was in the casinos on the ship a lot. She thought the cigarette smoke could have been making her cough but it is not any better. She now feels congestion in her chest and c/o hoarseness and expiratory wheezing. location: congestion in chest quality: patient describes a feeling of tightness in her chest severity: patient rates pain a “3” on a scale from 1-10. She states her cough is constant and is continuing to worsen timing: symptoms started 2 weeks ago setting: patient states her symptoms started while she was on a cruise in the ship’s casinos alleviating and aggravating factors: cough is worse at night, with any physical exertion, or when she gets hot. She states she still coughs at rest but it is somewhat better. associated signs and symptoms: hoarseness and expiratory wheezing PAST MEDICAL HISTORY (PMH): Allergies: NKDA Current medications: citalopram 40 mg tablet, levothyroxine 50 mcg tablet, pantoprazole 40 mg tablet, delayed release Age/health status: 61 years Appropriate immunization status: Up to date on all vaccines; Flu vaccine given November 2013. She states she will be getting the flu and pneumonia vaccines at her primary physician’s office this fall. Previous screening tests result: Patient states she had a pap smear and mammogram in March 2014 and both were reported normal. Dates of illnesses during childhood: N/A Major adult illnesses: Patient states she has a history of depression, hypothyroidism, and GERD Injuries: N/A Hospitalizations: No hospitalizations other than when she had a tonsillectomy as a child Surgeries: Tonsillectomy at age 10 FAMILY HISTORY (FH): Father has a history of HTN and Type II Diabetes; Mother has a history of COPD. Patient has 1 sister who has HTN. She does not have any children. SOCIAL HISTORY (SH): She is married and works as a social worker for DHR. She is independent with her ADLs and lives with her husband. She states she currently exercises about 3 times per week which includes brisk walking for about 1 mile. She is a former smoker- ½ pack/day but she states she quit 5 years ago. She does drink alcohol occasionally if she is at a social event. She drinks caffeine (coffee or soda) 1-3 times daily. No illicit drug use. REVIEW OF SYSTEMS (ROS): 1. Constitutional symptoms- Patient reports fatigue, fever, and difficulty sleeping due to coughing. Patient denies chills, malaise, night sweats, unexplained weight loss or weight gain, loss of appetite. 2. Eyes- Patient denies blurred vision, difficulty focusing, ocular pain, diplopia, scotoma, peripheral visual changes, and dry eyes. Patient states she does wear reading glasses. Date of last eye exam was in 2013. 3. Ears, nose, mouth, and throat- Patient reports headaches and hoarseness. Patient denies vertigo, sinus problems, epistaxis, dental problems, oral lesions, hearing loss or changes, nasal congestion, sore throat. Date of last dental visit was about 6 months ago. 4. Cardiovascular- Patient states she exercises about 3 times a week for about 30 minutes to an hour. Patient denies any history of heart murmur, chest pain, palpitations, dyspnea, activity intolerance, varicose veins, edema. Date of last EKG and cholesterol level was in March 2014 at her yearly physical and was reported normal. 5. Respiratory- Patient reports cough, SOB on exertion, difficulty breathing at times, expiratory wheezing, chest tightness/pain on inspiration, exposure to secondary smoke. Patient denies history of respiratory infections, exposure to TB, hemoptysis. Patient states she has never had a chest x-ray. Her last TB skin test was done in March 2014 for work and it was negative. Patient states she is a former smoker but quit 5 years ago. 6. Gastrointestinal- Patient reports a history of GERD. She states she was diagnosed about 1 year ago and it is managed well with protonix. Patient denies dysphagia, reflux, pyrosis, loss of appetite, bloating, nausea, vomiting, diarrhea, constipation, hematemesis, abdominal or epigastric pain, hematochezia, change in bowel habits, food intolerance, flatulence, hemorrhoids. Patient states she tries to eat healthy, well-balanced meals. 7. Genitourinary- Patient denies urgency, frequency, dysuria, suprapubic pain, nocturia, incontinence, hematuria, history of stones, vaginal discharge. Patient states her LMP was about 9 years ago. She does not take any hormone replacements. Her last pap smear was in March 2014 and was reported normal. Her last mammogram was in March 2014 and was reported normal. 8. Musculoskeletal- Patient denies back pain, joint pain, swelling, muscle pain or cramps, neck pain or stiffness, changes in ROM. She states she exercises about 3 times a week. She does wear her seatbelt. 9. Integumentary- Patient denies itching, uritcaria, hives, nail deformities, hair loss, moles, open areas, bruising. Patient denies breast tenderness, masses, skin changes. She states she uses sunscreen while outside and inspects her skin regularly for any changes. 10. Neurologic- Patient reports a headache. Patient denies weakness, numbness, muscular weakness, tingling, memory difficulties, involuntary movements or tremors, syncope, stroke, seizures, paresthesias. 11. Psychiatric- Patient reports a history of depression. She was diagnosed in her late 30s but states it is well controlled with celexa. Patient denies nightmares, mood changes, anxiety, nervousness, insomnia, suicidal thoughts, exposure to violence, or excessive anger. 12. Endocrine- Patient reports hypothyroidism. She was diagnosed about 10 years ago and has been taking levothyroxine to manage it. Patient denies cold or heat intolerance, polydipsia, polyphagia, polyuria, changes in skin, hair or nail texture, unexplained change in weight, changes in facial or body hair, changes in hat or glove size, use of hormonal therapy. 13. Hematologic/lymphatic- Patient denies unusual bleeding or bruising, lymph node enlargement or tenderness, fatigue, history of anemia, blood transfusions. Patient is unsure of last HCT result but states all lab work was done at her last physical in March 2014 and everything was reported to her as “normal”. 14. Allergic/immunologic- Patient denies seasonal allergies, allergy testing, exposure to blood or body fluids, use of steroids, or immunosuppression in self or family. She is unsure of her last Hep B vaccine but states she has had one for work. OBJECTIVE DATA (O): 1. Constitutional- VS: Temp- 96.8, BP- 124/74, HR- 74, RR- 18, O2 sat- 97%, Height5’5”, Weight- 170 lbs, BMI- 28.29; General Appearance: healthy-appearing, wellnourished, and well-developed . Level of Distress: NAD. Ambulation: ambulating normally. 2. Eyes- sclerae white. Conjunctivae pink. Pupils are PERRL, 3 mm bilaterally. Extraocular movements intact. 3. Ear, Nose, ThroatEars: external appearance normal-no lesions, redness, or swelling; on otoscopic exam tympanic membranes clear. Hearing is intact. Nose: appearance of nose normal with no mucous, inflammation, or lesions present. Nares patent. Septum is midline. Mouth: pink, moist mucous membranes. No missing or decayed teeth. Throat: no inflammation or lesions present. Tonsils WNL- no erythema, ulcers, masses, exudate, inflammation. 4. Cardiovascular- S1, S2. Regular rate and rhythm, no murmurs, gallops, or rubs Carotid Arteries: normal pulses bilaterally, no bruits present Pedal Pulses: 2+ bilaterally Extremities: no cyanosis, clubbing, or edema, less than 2 second refill noted 5. Respiratory- Even and unlabored. Bilateral expiratory wheezes and fine crackles in upper lobes on auscultation. Non-productive, hacking cough frequently. Patient is unable to take a deep breath without coughing. Fremitus is equal and there is no egophony. 6. Gastrointestinal- abdomen soft and nontender to palpation, nondistended. No rigidity or guarding, no masses present, BS present in all 4 quadrants 7. Genitourinary- No bladder distention, suprapubic pain, or CVA tenderness. Pelvic exam was not performed. 8. Musculoskeletal- joint stability normal in all extremities, no tenderness to palpation 9. Integument/lymphaticInspection: No scaling or breaks on skin, face, neck, or arms. General palpation: no skin or subcutaneous tissue masses present, no tenderness, skin turgor normal Face: no rash, lesion, or discoloration present Lower Extremities: no rash, lesion, or discoloration present Upper Extremities: no rash, lesion, or discoloration present 10. Neurologic- Grossly oriented x3, communication ability within normal limits, attention and concentration normal. Sensation intact to light touch, gait within normal limits 11. Psychiatric- Judgment and insight intact, rate of thoughts normal and logical. Pleasant, calm, and cooperative. Patient appears to be happy/content. 12. Hematologic/immunologic- Lymph nodes not palpable, no tenderness or masses present, no bruising DIAGNOSTIC TESTS: X-RAY, CHEST - 08/26/14 Results: no acute findings that suggest pneumonia ASSESSMENT (A): 1. Bronchitis 490: Bronchitis, not specified acute or chronic Patient reports frequent cough that is worse at night, congestion, chest tightness, hoarseness, expiratory wheezing, headache, and fever. Bilateral expiratory wheezes and fine crackles in upper lobes on auscultation. Nonproductive, hacking cough frequently. Patient is unable to take a deep breath without coughing. Fremitus is equal and there is no egophony. 2. 311: Depression Currently controlled. Patient is taking citalopram 40 mg tablet daily 3. 244.9: Hypothyroidism Currently controlled. Patient is taking levothyroxine 50 mcg tablet daily 4. 530.81: GERD Currently controlled. Patient is taking pantoprazole 40 mg tablet, delayed release daily Differential Diagnoses: 1. Pneumonia Patient c/o cough, fever, chest discomfort, crackles and expiratory wheezes on exam. Refuting data: ruled out with chest x-ray. No shaking chills, rigors, tachycardia, tachypnea, uneven fremitus, or egophony. 2. Sinusitis Patient c/o cough, fever, headache, and difficulty breathing at times. Refuting data: Patient c/o congestion in chest and not sinuses. No sore throat, purulent nasal drainage, or ear pain. 3. Asthma Patient c/o chest tightness/congestion, non-productive cough, SOB with exertion, and wheezing. Refuting data: Patient’s complaint is acute. PFTs are needed to completely rule out. 4. Tuberculosis Patient c/o fatigue and fever, non-productive cough. Refuting data: No progressive dyspnea, night sweats, weight loss, or hemoptysis. CXR did not show TB. 5. GERD Patient c/o cough. Patient has a history of GERD. Refuting data: No heartburn or other GI symptoms noted. 6. Malignancy History of smoking. Patient c/o dyspnea at times, cough, fatigue, wheezing, and chest discomfort/tightness. Refuting data: No hemoptysis, recurrent respiratory infections, unexplained weight loss. PLAN (P): 1. Cefdinir 300mg capsule; Take 1 capsule by mouth every 12 hours for 10 days Albuerol sulfate HFA 90mcg/actuation aerosol inhaler; Inhale 2 puffs every 4 hours Depo-medrol 40mg/ml suspension for injection- IM injection in office Dexamethasone 4mg/ml injection solution- IM injection in office Take cefidinir 300mg twice a day for 10 days for the infection. Importance of finishing antibiotic even if symptoms improve or go away. Albuterol sulfate inhaler will help with the wheezing. Steroid shot in office will help control the symptoms and reduce inflammation so it will be easier for you to breathe. Continue with smoking cessation and avoid secondary smoke inhalation and other environmental irritants. Return to the urgent care clinic or follow-up with your primary physician if symptoms persist longer than 21 days or if condition worsens. Health promotion: flu and pneumonia vaccines at next primary physician appointment this month. 2. Continue taking citalopram 40 mg PO daily to manage depression. Continue follow-up with primary physician every 3 to 6 months. 3. Continue taking levothyroxine 50 mcg PO daily to manage hypothyroidism. Continue follow-up with primary physician for lab work to check thyroid levels. TSH levels should be monitored every 6 to 12 months. Take levothyroxine with water consistently 30-60 min before breakfast or at bedtime 4 hours after last meal. 4. Continue taking pantoprazole 40 mg PO daily to manage GERD. Lifestyle modifications such as avoiding foods that may precipitate reflux and cause heartburn. Adopt behaviors that may decrease acid exposure such as weight loss, elevating HOB, and avoiding lying down 3-4 hours after a meal. Continue follow-up with primary physician. -