- India Environment Portal
advertisement

Draft Guidelines for Regulating Food High in
Fat, Sugar and Salt (HFSS) also popularly
known as Junk Food
Working Group set up by the Expert Group set up as per the
order dated September 4, 2013 of the Honorable High Court of
Delhi
January 16, 2014
1
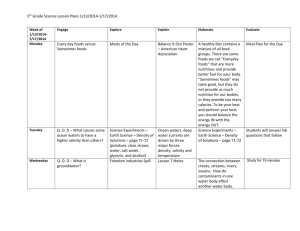
Contents
1. Background
1.1 Directions of the Honorable Court
1.2 FSSAI draft guidelines: Review and analysis
2. Balanced diet, junk food and non-communicable diseases
2.1 Balanced diet and dietary needs of children
2.2 HFSS food and the ingredients of concern
2.3 HFSS food consumption in India
2.4 HFSS food and the burden of non-communicable diseases
2.5 HFSS food regulations
3. Draft guidelines for regulating consumption of HFSS food among children
Annexure
1.
Details of HFSS food regulatory status across the world
2.
Nutrient Profiling Model of the United Kingdom and Scoring
3.
Model school canteen policy – Australia
4.
Minutes of Meeting of Working Group set up by the Expert Group held on January 8,
2013
Guidelines on wholesome food and nutrition in school canteen submitted by Industry
representatives on January 3, 2014
5.
References
2
Working Group set up by the Expert Group set up as per the order dated September 4, 2013 of the
Honorable High Court of Delhi on guidelines for making available quality and safe food in schools.
Members
1. Dr Sunita Narain, Director General, Centre for Science and Environment, Delhi (Co-Chair)
2. Dr Rekha Harish, Professor and HoD, Dept. of Paediatrics, Government Medical College,
Jammu(Co-Chair)
3. Dr Anju Seth, Professor, Dept. of Paediatrics, Lady Hardinge Medical College, Delhi
4. Ms Anuja Aggarwal, Nutritionist, AIIMS, Delhi
5. Dr K Damayanti, Scientist C, National Institute of Nutrition, Hyderabad
6. Ms. Kumkum Marwah, Representative, Advisor Nutrition, Ministry of Health and Family Welfare
7. Dr Umesh Kapil, Professor, Public Health Nutrition, AIIMS, Delhi
The representatives of industry associations and experts listed below, submitted on January 3, 2013 a
document titled, Guidelines on Wholesome Food and Nutrition for School Canteen. This document was
discussed at the meeting of the working group on January 8, 2013. The minutes of the meeting record the
areas of agreement and outstanding issues where there was no consensus (Annexure 5). The current
guidelines incorporate the issues where there was agreement. However, as there are outstanding issues
where no agreement was possible, the document submitted by the representatives of industry
associations and experts is given in Annexure 6.
1.
2.
3.
4.
5.
6.
Mr. N Ramasubramanian, Retailers Association of India*
Dr. P. S. M. Chandran, Retailers Association of India*
Dr Mridul Salgame, Restaurant Association of India*
Mr Sunil Adsule, National Restaurant Association of India**
Mr Sanjay Khajuria, All India Food Processors’ Association**
Dr S Jindal, All India Food Processors Association**
* New members of the Working Group as per the Expert Group Meeting of December 3, 2013
**New members of the Working Group as per the Expert Group Meeting of December 13, 2013
Meeting Details
Time: 2:00 PM to 5:00 PM
Place: CSE Office, India Habitat Centre, New Delhi
Meeting 1
Meeting 2
Meeting 3
November 26, 2013
December 06, 2013
January 08, 2014
3
Section1: Background
1.1 Directions of the Honorable Court
Order dated September 4, 2013 of the Honorable High Court of Delhi; W.P. (C) 8568/2010: Uday
Foundation for Congenital Defects and Rare Blood Groups Versus Union of India and Others
----------------------------------------------------------------------------------------------------------------------------- --------------The key concern expressed by the Court in the order dated September 4, 2013 is the ill effects of
consuming ‘junk food’ as a 'dietary habit' by children. The Honorable Court says "Whereas nobody
can question the interest of the society in its children eating wholesome and nutritious food and abjuring
eating ‘junk food’, which may be consumed once in a while; to satisfy the tongue. Ordinarily, as a daily
intake, wholesome and nutritious food should be consumed by the children. The ill effects of eating ‘junk
food’ in today’s environ [environment] has been documented by public health experts as also
pediatricians’.
With reference to the term 'junk food', the Court clearly is referring to the food that is high in
calories and low in nutrition. The Court recognizes that medical problems such as obesity,
hypertension and diabetes in children are direct consequence of excessive consumption of junk
food. Further, in order to prepare the draft guidelines, it directed Central Advisory Committee of
FSSAI to consult experts in public health, particularly health of a child, adolescent and the youth;
and those with expertise on junk food and its ill effects if consumed as a dietary habit. The order
says “The FSSAI would be permitted to take the help of experts in the field of not only public health but
even those who are concerned with the dietary habits of the adolescent and the youth as also those who
have expertise in controlling child obesity, child hypertension, child diabetes etc. i.e. such medical
problems which are faced by children today which are the direct consequences of excessive consumption
of ‘junk food’ by the children.”
The Court notes the inadequacy of the draft guidelines submitted by Nielson India Pvt. Ltd. in
addressing the prayers in the original petition. It directed that the guidelines submitted would at
best be a take off point with reference to the data collected and analyzed. The order says that “The
report submitted by Nielsen (India) Pvt. Ltd. would at best be a take off point with reference to the data
collected and analyzed."
-------------------------------------------------------------------------------------------------------------------------------------------Later, in the order dated 29 October, 2013, the Court once again clarified over the key concern of
the original writ petition and said "We only need to highlight that our order dated September 04, 2013
brings out that the concern in the writ petition is not with hazardous food or with a standard of food safety
envisaged by the Act. The concern is with a dietary habit and promotion of what is popularly known as
junk food amongst school children"
Case background
In Dec 2010, Uday Foundation for Congenital Defects and Rare Blood Groups filed a writ petition
before the Hon'ble High Court of Delhi. Citing the growing incidence of childhood obesity, the
petitioner prayed the Hon'ble Court to pass certain directions that were aimed at limiting the
availability and exposure of junk food to children. Subsequently, the Court directed the Union of India
to file an affidavit stating steps being contemplated or going to be taken and file an action taken
report. After an additional counter affidavit stating that the FSSAI is undertaking a project for
development of guidelines for making available quality and safe food in schools, the Hon'ble Court in
January 2012 allowed six months to complete this study. The draft guidelines prepared by Neilsen 4
India Pvt. Ltd., to whom FSSAI awarded the project were later submitted. The Court gave further
directions in its order of September 4, 2013 (as above)
1.2. FSSAI draft guidelines: Review and analysis
Draft Guidelines for Making Available Quality and Safe Food in Schools
Submitted to the Honorable High Court of Delhi
-------------------------------------------------------------------------------------------------------------------------------------------How the guidelines fail to address the original petition?
The draft guidelines for making available quality and safe food in schools, submitted by Neilson seem to
be focused on meals provided by the government under nation-wide programmes such mid-day meal
scheme of the Department of Education and Literacy, Ministry of Human Resource and Development.
The essence of original petition on the other hand is about limiting the availability of unhealthy and
unhygienic food products that are commercially sold to urban school children and regulating
advertisements targeted to this vulnerable group of consumer, which has limited discretion. The prayers
in the original petition are:
1. To immediately ban junk food and carbonated drinks in all unaided and private schools and
schools under Central and State government and local municipality in Delhi
2. To initiate measures to discourage the availability of fast food, unhygienic food and foods with
unhealthy ingredients within 500 yards of the schools in Delhi
3. To further direct respondents to develop a comprehensive school canteen policy, which
emphasizes healthy nutrition among school going children?
4. To ban junk food and carbonated drinks advertisements in media as well as in the television
through any means
The draft guidelines are clearly addressing other end of the nutrition problem in India. It is about providing
appropriate nutrition to the under-nourished children, whereas the premise of the original petition is
increasing health problems in children due to excess calories from junk food. Consequently, the
geographic focus of the survey and subsequent guidelines seem inappropriate to address the prayers in
the petition.
In terms of the public health objective, the guidelines are about reducing the incidence of diet related
deficiency diseases such as iron deficiency anemia, vitamin A and iodine deficiency diseases in children.
However, the directions sought by the petitioner are to prevent early onset of non-communicable
diseases such as obesity, diabetes, blood pressure in children.
In terms of observations on specifics of the guidelines, with reference to the guidelines mentioned on
quality and safety of the food, well laid out and time tested guidelines are already available under the MidDay Meal Scheme. These could be used if required. Moreover, FSSAI's Food Safety and Standards
(Licensing and Registration of Food Businesses) Regulations, 2011 also cater to similar issues of
General Hygiene and Sanitary Practices that are to be mandatorily followed by food business operators.
The guidelines also fail to appropriately classify unhealthy food in a section wherein the issue of
unhealthy and unhygienic food in schools and nearby is addressed briefly. Also, there is no mention of
suggestions on promotion of unhealthy foods and advertisements.
There is limited clarity on the design of the survey and how at its first place it was envisaged to
address the original prayers in total or partly. What is known is that the study objectives set by
FSSAI were in the knowledge of the Honorable High Court of Delhi. However, the Court in its order
5
dated 04 September, 2013 has directed further consultation with experts and suggested
considering the data and analyses of the submitted guidelines as a take off point at best.
Section 2: Balanced Diet, HFSSfood and Non-communicable diseases
2.1Balanced diet and dietary needs of children1
As per "Dietary Guidelines for Indians, 2011" by National Institute of Nutrition (NIN), a balanced diet is
one which provides all nutrients in required amounts and proper proportions. It should provide around 5060% of total calories from carbohydrates, preferably from complex carbohydrates, about 10-15% from
proteins and 20-30% from both visible and invisible fat. In addition, it should provide other non-nutrients
such as dietary fibre, antioxidants, which bestow positive health benefits.
The guidelines depict the importance of foods through a "Food Pyramid". Balanced diet is recommended
through a blend of four basic food groups such as cereals, millets and pulses; vegetables and fruits; oils,
fats and nuts; milk and animal foods. Notably, food items such as burgers, pizza, fries, chocolates, ice
cream, jam etc are not considered the right choice to meet nutrient needs and must be eaten sparingly.
Figure 1: Food Pyramid by NIN
Eat Sparingly
Eat Moderately
Eat Liberally
Consume Adequately
Source: Dietary Guidelines for Indians,NIN; Reproduction of the figure mentioned
The guidelines recommendpreferring traditional and home-made foods; avoiding replacing meals with
snack foods; and limit consumption of sugar and processed foods which provide only (empty) calories. It
further statesthat "processed foods being rich in fats, salt, sugar and preservatives may pose a health risk
if consumed regularly".
6
It also recognizes children's special needs of growth, fighting infections, maturation, bone development
and bodybuilding. Nutritionally adequate and balanced diet has an important role in appropriate body
composition, body mass index and reduced risk of diet-related chronic diseases in later life.
2.2 ‘HFSS Food' and ingredients of concern
As per NIN “junk foods as those containing little or no proteins, vitamins or minerals but are rich in salt,
sugar, fats and are high in energy (calories).”
Globally as well, the term junk food is popularly used to identify food items with little or no nutritional value
but high in salt, sugar and fat.
Foods with similar attributes are termed as:
HFSS foods i.e. foods that are 'high in fat, salt and sugar' by WHO and several other countries
FMNV i.e. ‘foods of minimal nutritional value’ such as in the US
EDNPFC, i.e. ‘energy dense and nutrient poor foods for children’ such as in Republic of Korea
'Energy dense' foods by certain associations and countries
Such foods are regarded as not conducive in maintaining health. Key characteristics include:
Imbalance of nutrients:Excess of nutrients such as fat, sugar and salt (sodium) that have
negative impact on health, if consumed in high amount. In addition, proteins, vitamins,
phytochemicals, minerals and dietary fibre with a positive impact on health could be absent
orpresent in limited quantity.
Unfavorable nutrients and chemicals: Presence oftrans fats and preservatives and additives
used in processed foods that are known to have negative impact on health
Ingredients of junk food are known to impact health in several ways. Excess consumption is linked to
obesity. Numerous studies across the world have established strong linkage with non-communicable
diseases (NCDs) such as diabetes, hypertension, heart disease and cancer.
Sugar: Sugar is empty calories with no beneficial effect and there is no safe level of its intake. High use
of sugar, particularly fructose, is harmful as it is addictive and induces more consumption2. Studies have
confirmed that fructose which is most commonly used in carbonated beverages has toxic effects on the
liver that are similar to that of alcohol3.Studieshave established direct relationship of sugar with obesity,
diabetes and metabolic syndrome4.
Salt: Salt is added for preservation and enhancing the taste of food. High salt content in diet is strongly
associated with high blood pressure and related cardiovascular diseases 5. Evidence suggests that high
salt intake increases mass of left ventricle, stiffens and narrows arteries, including coronary and renal
arteries. It increases the probability of stroke, severity of cardiac failure and tendency for platelets to
aggregate6. As per WHO, cutting down on dietary salt intake to recommended 5 g per day has a major
impact on reducing blood pressure and cardiovascular diseases.
Saturated Fatty Acid (SFA): SFAs are widely used in packaged foods including milk chocolate,
cookies, crackers, and snack chips. When consumed in excess of the recommended (limit less than 10%
of total calorie intake), SFAs are known to clog arteries and increase risk of heart attack and stroke.
7
Trans Fatty Acid (TFA): TFAs are formed during the process of hydrogenation of vegetable oils
(PHVOs) to make it semi solid that enables longer shelf life, better form and texture. Typically they are
found to be high in bakery products and snacks that are deep-fried in PHVOs.TFAs are well known to
have an adverse impact on blood lipid levels as they reduce the amount of good cholesterol (HDL) and
increase bad cholesterol (LDL). Their consumption increases insulin resistance and promotes obesity.
WHO recommends less than 1 percent of calories from TFAs.
Besides the above key ingredients of concern, Caffeineused in carbonated beverages and energy drinks
is an addictive stimulant, which if consumed in excess can lead to impaired muscle and nerve functions,
dehydration and a host of other disorders7. For children, caffeine consumption should not exceed
2.5mg/kg per day and for adolescents 100mg/day is the recommended limit.
2.3 Junk food and burden of NCDs in children
WHO reports that Non-Communicable Diseases are the leading cause of death worldwide:
Unhealthy diets, especially the excessive consumption of calories, salt, saturated fat and sugar
cause at least 40% of all deaths from NCDs, and approximately one-quarter of all deaths globally
Over 80% of global deaths due to cardiovascular diseases and diabetes occur in low- and middleincome countries. NCDs also kill at a younger age in these countries, where 29% of NCD deaths
occur among people under the age of 60, compared to 13% in high-income countries
In India, as of 2008, about 53% of all deaths were due to NCDs.The disease burden of NCDs is
expected to reach to 57% by 2020 as compared to 29% in 19909
WHO says unhealthy diet is associated with three out of four major NCDs. It is known one of the
modifiable risk factors:
Table 1: Modifiable risk factors - Unhealthy diet associated with three out of four major NCDs
Tobacco Unhealthy diet
Physical
Harmful use of
Use
inactivity
alcohol
Cardiovascular diseases
√
√
√
√
Diabetes(Type2)
√
√
√
√
Cancers
√
√
√
√
Chronic Respiratory
Diseases
√
Unhealthy diet leads to metabolic changes and conditions such as overweight, high blood pressure, raised
blood glucose and cholesterol, which are among the leading causes of NCD deaths in India 10
Childhood obesity
Childhood obesity is one of the most serious public health challenges of the 21st century. Overweight
children are likely to become obese adults. As per WHO, about 44% of the diabetes burden and 23% of
the CVD burden is attributable to overweight and obesity. Overweight children are more likely than nonoverweight children to develop insulin resistance, hyperinsulinemia, diabetes and cardiovascular diseases
at a younger age, which in turn are associated with a higher chance of premature death and disability11.
8
Studies have established the link between consumption of HFSS food and obesity. Numerous studies
done among school children of Delhi, Amritsar, and Southern Indiashow that the prevalence of
overweight/obesity is high and on the rise.Inurban post-pubertal children of Delhi it increased from 16% in
2002 to about 24% in 2006. It is high among the affluent class and children of private schools compared to
low and middle-income groups12
Hypertension
In India, hypertension is the leading NCD risk and estimated to be attributable for over 10 per cent of all
deaths13.Hypertension is strongly associated with high Body Mass Index (BMI) and salt intake. A cross
sectional study14, published in Epidemiology in 2013, among 400 school children in Chennai found that
the total prevalence of hypertension was 21.5%. Several other studies done in India suggest high
prevalence of hypertension in overweight and obese children compared to normal weight children15.
As per WHO, the amount of dietary salt consumed is an important determinant of blood pressure levels
and overall cardiovascular risk. World Heart Federation says that a universal reduction in dietary intake of
about 3 gms of salt, would lead to a 50% reduction in the number of people needing treatment for
hypertension. The same decrease would lead to a 22% drop in the number of deaths resulting from
strokes and a 16% fall in the number of deaths from coronary heart disease16
Diabetes and pediatricmetabolic syndrome
Type 2 diabetes which is very common in adults is now increasingly being reported in children. The
leading risk factor for kids is being overweight, often connected with an unhealthy diet and lack of
physical activity.According to a study done by Dr Anoop Mishra et al on post pubertal Indian children,
67% males with high BMI were found to have insulin resistance while overall prevalence was about 22%
in males and 36% in females17. As per the Diabetes Atlas 2006 published by the International Diabetes
Federation, the number of people with diabetes in India is around 40.9 million and is expected to rise to
69.9 million by 2025 unless urgent preventive steps are taken18.
Metabolic syndrome is a cluster of the risk factors for type-2 diabetes and cardiovascular
diseasecharacterized byabdominal obesity and others such as high blood pressure and increased plasma
glucose. The prevalence of metabolic syndrome in overweight children was found to be about 18 times
higher than their normal weight counterparts in Delhi.19
Coronary Heart Disease (CHD
CHD is expected to be the single most important cause of death in India by the year 2015. According to
the World Heart Federation, 35% of all CHD deaths in India occur in those aged 35-64 years. CHD affects
Indians with greater frequency and at a younger age than counterparts in developed countries, as well as
many other developing countries20.The age group 20-29 has seen the highest rise with double the
number of cases since 2000 as per a study in Indian Journal of Medical Research 21.
A study published in the American Journal of Clinical Nutrition in 2009 showed that those students
who attended school near fast food restaurants were heavier than their counterparts who attended
school that were not near a fast food restaurant. Students with a high intake of fast food had a low
intake of fruits and vegetables22.
Another study published recently in Endocrine Reviewsstate that one of the key determinants of
childhood obesity was increased calorie intake among school children. Unrestricted access to
energy-dense fast foods in school cafeteria, school vending machines, and school neighborhood
9
along with low knowledge about dietary components are found to be the major contributors. The
researchers recommend that schools must keep healthy food in their cafeteria and suggested a ban
on sweetened beverages and energy-dense junk food in schools to curb childhood obesity23
2.4 HFSS food consumption in India
Consumption of 'HFSS Food' is steeply increasing both in urban and rural areas. The ease of availability,
taste, low cost, aggressive marketing and advertisements and peer pressure make them popular with
children and adolescents.
Table 2: Consumption of processed foods (gm or ml/day) at 95 th percentile among urban
population in India (unpublished data, NIN study done for FSSAI)
Food group
Fried snacks
Noodles
Bakery items
Carbonated &caffeinated
beverages
HIG (High
Income
group)
61.0
100
12.2
200.0
MIG (Middle
Income Group)
55.6
100
6.0
57.1
LIG (Lower
Income
Group)
75.0
94
27.2
70.8
ILW (Industrial
Labor
workers)
53.8
29.3
16.1
71.4
Slums
68.5
100
60.0
42.8
A study on the HFSS Food eating habits of school children in Delhi found that 60-70% of children in
different age groups consumed chips at least 2-3 times a week24. In another study among overweight
adolescent girls (16-18 years) in Kurukshetra in 2013, the mean daily energy intake was found to be
about 110 per cent of the Recommended Daily Allowance (RDA) andfat intake was almost double of the
RDA.The most common (60.4%) effect of skipping meal was consumption of foods such as potato chips,
chocolate and carbonated drinks25.
According to an assessment by CRISIL in 2013, the fast food restaurant market is increasingly expanding
to Tier II and Tier III cities. It is projected to double in the next few couple of years and annual spending
per middle class household at such restaurants is expected to increase 1.5 times by 2015-1626.
HFSS food replacing balanced diet is a key issue: As perNIN dietary guidelines "the shift from
traditional to 'modern' foods, changing cooking practices, increased intake of processed and ready-to-eat
foods, intensive marketing of HFSS foods and 'health' beverages have affected people's perception of
foods as well as their dietary behavior. Irrational preference for energy-dense foods and those with high
sugar and salt content pose a serious health risk to the people, especially children. The increasing
number of overweight and obese people in the community and the resulting burden of chronic noncommunicable diseases necessitate systematic nutrition educational interventions on a massive scale."
Additionally, a lot is at stake if balanced diet is replaced:A diverse range of macronutrients and
micronutrients in its most natural form; Original flavors, colors and aroma that continue to keep the
appetite alive for a lifetime; A wide range of time tested spices and herbs that continue to act at a
prophylactic level (preventive) at sub-therapeutic levels.
10
2.5 HFSS food regulations
There is an overwhelming view that children’s exposure to HFSS food must be minimized and regulated.
The 2004 Global Strategy on Diet, Physical Activity and Health of WHOstated that “food advertising
messages that encourage unhealthy dietary practices should be discouraged and the governmentshould
develop a multi-sectoral approach to address any such issues.” Later, it was noted that advertising to
children included promotion that is deliberately targeted at children and promotion targeting other groups
but to which children are widely exposed.In 2012, WHO provided a framework for implementing the set of
recommendations on the marketing of food and non-alcoholic beverages to children.
WHO Europe in its latest report in 2013 acknowledged that marketing of food and beverage products that
are high in fat, sugar and salt to children is recognized as an important cause of child obesity and dietrelated non-communicable diseases.
To respond to obesity and NCD epidemic, several countries have adopted one or more of the following
three approaches. Typically food items that are high in fat, sugar, salt and low in nutritive value are
selected for regulating their exposure and availability to children.
To ban the use and availability of such food in schools
To regulate the marketing of such foods so that exposure is reduced
To impose taxes on such foods so that use is restricted
Table 3: Summary of regulatory status across the world (non exhaustive)*
Ban in Schools
Advertisements Restricted
Tax Imposed
Canada, Ontario (2011)
Australia (Bill Proposed/pending)
France (2012)
Costa Rica (2012)
Canada (1971)
Hungary (2011)
Latvia (2006)
France (2007)
Ireland (under progress)
Lithuania (2010)
Lithuania (under progress)
Latvia (2010)
Mexico (2011)
New Zealand (2010)
Mexico (2013)
Peru (2013)
Norway (2012)
Peru (under progress)
Philippines (2007)
Peru (2013)
Romania (under progress)
Poland (under progress)
Poland (2007)
Switzerland (2008)
South Korea (2009)
Romania (2008)
Taiwan (under progress)
UK, England (2006)
South Korea (2010)
United States (San
Francisco)
UK, Scotland (2008)
Sweden (1991)
United Arab Emirates (2011)
Taiwan (under progress)
United States (to be implemented) United Kingdom (2008)
United States (under progress)
Uruguay (2013)
*Details are mentioned in annexure
Several countries have imposed a tax on beverages, energy drinks, sugar sweetened/flavored
beverages, packaged sweets, ice creams, jam, salty snacks, chocolates and food flavoringswhile an
indicative list of food items either banned from schools or with advertising restrictions is given below:
11
Table 4: Indicative food items with restricted marketing/availability in schools (non exhaustive)
Cereal products with added
sugars
Cola and other carbonated
sweetened drink
Mayonnaise, peanut butter
Cheddar cheese
Chocolate and nougat
Pizzas
Butter and margarine
Roasted chicken bites and
Chicken nuggets
Pork rinds, fried tacos and tortas
Sausages and burgers
Yoghurt candies and Water ices
Cakes and muffins
Potato chips and crisps
Fizzy orange drink and sweet
juices
Marshmallow candies, spun candy,
and candy-coated popcorn
Cookies
Drinking chocolate powder and
sports drinks
Hamburgers and instant noodles
Confectionary- sugar boiled
confectionary, candies
Onion rings, sweetened
milkshakes
Jams, marmalades, highlysweetened syrup, sweets,
French fries
Crispy chicken strips in tortilla
wrap
Atole (a sweetened corn starchbased beverage)
12
Section 3: Guidelines for regulating consumption of HFSS food
among children
Principles on which the proposed guidelines are based upon:
Children are not the best judge of their food choice. Theyhave limited
understanding on the impact of food on their health. Broadly, they are not aware about
the concept of balanced diet and what kind of food is to be consumed and avoided to
achieve it. They also lack required know-how on diseases and its relation to diet.While
on one hand, they lack awareness and necessary discretion, they are being
aggressively targeted by food marketing on other side. They are one of the biggest
viewer groups of television and food advertisements constitute a major share of overall
TV, radio and print advertisements across the world.
Schools are not the right place for promoting HFSS foods. Schools are a place to
learn right values and constructive behaviors for a lifetime. Since food consumption at
school is significant part of the overall daily diet, schools should not allow the canteens
to promote food habits that negatively impact the health of children.
Benefits of balanced, fresh and traditional food cannot be replaced. Frequent
consumption of foods high in salt, sugar and fats and low in other essential macro and
micronutrients is detrimental and should best be avoided. Such eating behaviors may
extend beyond schools and become a dietary habit
1. BAN THE AVAILABILITY OF MOST COMMON HFSS FOODS IN SCHOOLS AND
NEARBY AREAS OF 500 YARDS
The objective is to restrict the consumption of food in the school premise, where the
child is without parental supervision.
In schools and nearby areas of 500 yards, ban the availability of following most common
HFSS foods that are widely promoted and advertised, easily accessible to children, and
are standardized processed foods.Availability of similar foods is also banned/restricted
in schools of several countries across the world.
Table5: HFSS Foods to be banned in schools and in nearby areas of 500 yards
S. No.
Most Common HFSS Foods
1
Chips, fried packaged foods and similar packaged food items
2
Carbonated beverages
13
3
Sugar sweetened non-carbonated beverages
4
5
6
Instant noodles
Potato fries
Confectionery items such as chocolates, candies, gums
The identified foods are based on an evaluation done out of available similar foods in
India. They are considered unhealthy due to imbalance in nutrients i.e. high in fat,
sugar, salt and/or low in proteins, fibers and nuts. Two criteria have been used for
evaluation (see note 1: Objective and scientific criterion for categorizing HFSS).
FSSAI/NIN should initiate steps to develop a programme for identification of further
foods based on the above criterion and inform schools accordingly.
Besides the listed foods, another food category of concern is the non-standardised deep
fried foods such as samosa, chana bhatura, etc that are available in the school
canteens and nearby areas. More data is required on nutrient composition of such
foods. Moreover, such foods are non-standardised and therefore their nutrient
composition cannot be same, as it will depend on the ingredients used in different
institutions/households. The school management must ensure regulation of such foods
through canteen policies that promote healthy, wholesome and nutritious foods. The
school canteen policy would provide guidance on this matter to management.
2. TO DEVELOP A CANTEEN POLICY TO PROVIDE NUTRITIOUS, WHOLESOME
AND HEALTHY FOOD AT SCHOOL
Canteens in the schools should not be treated as commercial outlets. They carry a
social responsibility towards inculcating healthy eating behaviours. They can be used to
motivate children to consume healthy and hygienic food.Canteen policies based on
nutrition criteria has been developed in many other countries namely Australia, Canada,
Singapore, Abu Dhabi etc.A suitable canteen policy that enables nutritious, wholesome
and healthy foods to children should be developed in consultation with health ministry
and education ministry. It should be based on the following:
The school canteen policy should clearly specify the foods (category red), which
are not permitted for sale (as shortlisted above); foods that should be eaten most
(over 80% of the available choice/category green) and foods that should be eaten
sparingly (less than 20% of the available choice/category yellow).
14
The policy should be applicable for all types of schools such as primary,
secondary, day care, boarding etc. Depending upon the place and region, the
policy should include foods that are to be promoted as well as discouraged for
consumption by children.
The policy should also take into consideration non-standardized foods that are
sold in canteens and may extend to foods that are brought by children from home.
Regarding foods that are to be discouraged, suitable measures such as
decreasing the frequency and portion size could be suggested.
A 'School Health Team’ or similar unit could be set up in each school comprising
teachers, parents, studentsand school canteen operators, who will coordinate,
implement and monitor the canteen policy to make available quality and nutritious
food to students in schools.
A well-structured curriculum on balanced diet and its health impacts should be
introduced. The curriculum needs to take into account the level of students and
detail out as the children migrate from one class to another. NIN should be
involved in developing this curriculum.
Schools should also promote nutrition education and awareness among children
through various tools such as posters. If required a provision for funds from
Department of School Education and Literacy should be made.
Table 6: Food categorization and rationale
Green
Yellow
Red
Always on the menu
Select carefully
Approach should be greening,
small portion size and reduced
frequency
Not on the menu
Banned from schools as they are
high in fat, salt and sugar
Vegetables and legumes, fruits, grain (cereal)
foods;mostly wholegrain and/or high in fibre,
lean meat, egg, fish etc
Baked vegetable based snacks, ice creams,
milk-based ices and dairy desserts etc
Energy drinks, carbonated and other
sweetened beverages, Fried packaged foods,
chocolates,potato fries
15
3. REGULATE AND RESTRICT MARKETING AND PROMOTION OF 'HFSS FOOD'
TARGETED AT CHILDREN AND ADOLESCENTS
There is a substantial increase in advertising of foods high in fat, sugar and salt across
the world. Children are especially vulnerable to advertising because they cannot fully
understand the disguised persuasive techniques of the advertisements and judge
critically. The impact is exponential as proved by several studies. The objective is to
regulate the ‘exposure’ and ‘power’ of advertisements and promotional activities that are
targeted to children. These restrictions should be mandatorily enforced through
appropriate legislations and directives as the voluntary self-regulatory initiatives have
proved to address limited purpose.To begin with, list of foods shortlisted above are to be
considered. Subsequently, more foods identified as unhealthy be added.
Advertisements of ‘HFSS food’ targeted at children and adolescents should not be
designed and targeted to those <16 years of age across all media.
Such advertisements should not be allowed to broadcast on TV and radio during
4:00 PM to 10:00 PM on weekdays and during 8:00 AM to 10:00 PM on
weekends and holidays
Such advertisements should be banned from being broadcast during TV and
radio programmes having children and adolescents as a key audience. This
includes all kinds of cartoon shows and certain educational, entertainment and
sports programmes that are most designed for <16 years
There should be a ban on celebrity endorsements of 'HFSS food' by sports icons,
movie stars, child artists, famous cartoon and fictional characters
Restrictions should be imposed on such advertisements in new age marketing
channels such as internet, mobiles, paid TVs, social media. Special emphasis is
to be given to children related content such as gaming, sports, and academic
training modules.
Promotional activities of ‘HFSS food’ targeted at children are to be regulated.
Toys and other freebies should not be allowed to be given with such foods
Sports icons, movie stars, child artists, famous cartoon and fictional characters
should be barred from any open or disguised promotional activity in schools and
outside
In-school sponsorships of sports, cultural, literary or any other event by makers
(brands) of such foods should not be allowed
Promotion and marketing of such foods in all public areas where the children can
possibly aggregate (other than schools) is to be banned such as billboards,
advertisements at stadiums, airports and hospitals
16
4. FSSAI TO DEVELOP AND ENFORCE STRINGENT LABELING LAWS TO
ENABLE DISCLOSURE OF RELEVANT INFORMATION ON HFSS FOODS
The objective is to educate the consumer to facilitate an informed decision, as it is
critical to a healthy and balanced diet. In the current context, it is more about creating
awareness among parents at home that gets reflected into eating behaviors of the entire
family including children.As per WHO providing accurate, standardised and
comprehensible information on the content of food itemsis conducive to consumers
making healthy choices.
In India, the labeling rules mandate packaged food manufacturers to declare nutritional
information on product labels indicating the energy value in Kcal followed by the amount
of nutrients present.However, it needs to be made stringent. Centre for Science and
Environmentin the past found misleading claims on the amount of trans-fat present, lack
of standardized serving size and labeling criteria followed. Also, non-packaged HFSS
food items such as burger, fries and pizzas have their nutritional value and content on
their respective websites, which is of little or no value.
Nutrition Facts labeling at the back of the packet is to be mandatorily followed. It
should inform on how much the quantity of nutrients in a food packet and serving
size contribute to the total daily requirement. Desired information includes:
Serving size and number of serving size per packet/container
Per serving information and its contribution to RDA (in%) as per NIN
Calories
Key ingredients (in grams) such as total fat, saturated fat, transfat,
sugar, carbohydrates, proteins, salt/sodium etc
Total calorie count based on which RDA is calculated
Figure 2: Nutrition Facts Labelling
'
17
Front of the Pack' labeling that provides the Nutrition Facts in a simpler, easy to
understand figurative way is to be mandatorily practiced. Refer to an illustration below:
Figure 3: 'Front of the pack' Labeling
For non-packaged food items such as burgers, pizzas, stringent labeling regulations
must be enforced such as in the form of menu labeling, point of purchase labeling
boards, on paper wraps or boxes at the fast food outlets. Such labels should provide
information on calories and nutrients per serving size and as a percentage of RDA
by NIN.
5. ESTABLISH STRINGENT LIMITS FOR UNHEALTHY INGREDIENTS
From the perspective of controlling the intake of TFAs that are extensively used in
bakery, confectionery and deep fried cooking, a limit of 10% of trans fats in the cooking
medium i.e. Vanaspati etc. should be revised to 5% at the earliest. This would at least
make it closer to stringent norms followed in certain countries.
6. ENCOURAGE PHYSICAL ACTIVITY BY CHILDREN AND ADOLESCENTS
Physical activity complements maintaining good health if it is accompanied by a wellbalanced and nutritious diet. Government and schools should take initiatives to
encourage physical activity by children such as supporting infrastructure within and
18
outside the school, creating awareness among children and their parents, increasing
time and marks/grades allocated to sports.Children aged 5-17 should engage regularly
in physical activity of at least 40-45 minutes daily.
It is to be noted that the recommendations mentioned are just the beginning in
the task of regulating consumption of HFSS foods. They are far from being
sufficient. A lot needs to done in this regard and FSSAI should play an active role
in doing so. The work in this area will be critical to ensure food provides nutrition
and wellbeing to Indian children and secures their health.
Notes to explain the criterion based on which HFSS foods were identified and the sample menu
options for school canteen
Note 1: Objective and scientific criterion for categorizing HFSS
1. A scoring based nutrient profiling model practiced in the UK 1
Nutrient profiling is a science of classifying or ranking foods according to their nutritional composition for
reasons related to preventing disease and promoting health. The nutrient profiling model of the UK forms
the basis of a regulation, which prohibits advertising of specified food and beverages during children’s
programmes and programmes for which children under the age of 16 years form a disproportionate part
of the audience.
The model uses a simple scoring system wherein points are allocated on the basis of nutrient content of
100g of a food or drink. Points are awarded for ‘A’ nutrients (energy, saturated fat, total sugar and
sodium), and for ‘C’ nutrients (fruit, vegetables and nut content, fibre and protein). The score for ‘C’
nutrients is then subtracted from the score for ‘A’ nutrients to give the final nutrient profile score. If a food
or drink scores 11 or more ‘A’ points then it cannot score points for protein unless it also scores 5 points
for fruit, vegetables and nuts.Foods scoring 4 or more points, and drinks scoring 1 or more points, are
classified as ‘less healthy’ and are subject to controls on the advertising of foods to children on TV.
Table 7: Summary of scores depicting foods that are considered unhealthy*
Food Item
Branded Chips
Branded Aloo Bhujia
Cut-off score
4
4
Score
14
19
Branded instant noodles
4
19
Branded Aloo Burger
4
7
Branded Vegetable Burger
4
13
Branded Cola Drink 1
1
2
Branded Cola Drink 2
1
2
19
Branded Milk Chocolate
4
24
Branded Non-carbonated Fruit Beverage
1
3
* Scoring details are mentioned in annexure; source: company websites primarily
2. A “cut-off” criterion based on RDA of nutrients by NIN2, India
The criterion is based on RDA of nutrients provided by NIN, India. Most of these are in line with those
recommended by WHO. NIN guidelines have adapted to suit the Indian population.
Methodology for setting "cut-off" limit: RDA of calories and individual nutrients (refer 1 below) is
apportioned across meals and snacks throughout the day (refer 2 below).It is then compared with actual
amount of calories and respective nutrients that are present in foods. Foods with higher than the set 'cutoff' limit of one or more parameters are considered unhealthy. Breakfast and/or mid-morning snack is
considered for school children.
1. RDA of nutrients considered for children (based on 2100 Kcal for 10-12 years)
Salt/sodium: Total RDA for salt is 5 g /day, sodium 2 g/day as per NIN dietary guidelines
Total fats: Total fat intake should not be >30%E per day (WHO recommendation adopted by NIN)
Trans fatty acids (TFAs): Total RDA is <1% E per day (WHO recommendation adopted by NIN)
Added sugar: Total RDA 30 g sugar /day as per NIN dietary guidelines
Saturated fatty acid (SFAs): Total RDA is up to 8% E(WHO recommendation adopted by NIN)
2. Meal break–up considered (% total calories) developed by Working Group members
Breakfast
Mid morning snack
Lunch
Evening snack
Dinner
Bedtime
5%
25%
10%
25%
10%
25%
Table 8: Cut-off values for calories and nutrients that should not be exceeded in a snack or meal
Cut-off values of calories and nutrients (RDA for calories 2100) [ 10-12 years]*
% RDA
allocated
Kcal
limit
SFAs [g/% of
total]
TFAs [g/% of
total]
Sugar[g]
Salt/sodiu
m[g]
210
Total
fat[g/%
of total]
7/30
Snack
10
1.86/8
0.23/1
3
0.5/0.2
Meal
25
525
17.5/30
4.65/8
0.57/1
6.25
1.25/0.5
*Calculation illustration:
Kcal: 10% of 2100=210 Kcal; 25% of 2100=525 Kcal
Total fat: 30% E of 210 for snack = 63 Kcal and 63/9 (Kcal/gm of fat) = 7 g; similarly its 17.5 g for meal
SFAs: 8% E of 210 snack = 16.8 Kcal and 16.8/9 (Kcal/gm of fat) = 1.86; similarly its 4.65 g for meal
20
TFAs: 1% E of 210 snack =21 Kcal and 21/9 (Kcal/gm of fat) = 0.23 g; similarly its 0.57 g for meal
Sugar: 10% of 30 g (RDA) for a snack = 3g; similarly its 6.25 g for meal
Salt/Sodium: 10% of 5 g of salt (RDA) and 2 g of sodium (RDA) for a snack = 0.5 g of salt and 0.2 g of sodium;
similarly its 1.25 g of salt and 0.5 g of sodium per meal
Based on the cut-off values, various snack foods available in the India are evaluated. A red/bold figure in
the tables below highlights that the cut-off is exceeded vis-à-vis respective nutrient or calories.
Table 9: Examples of identified HFSS food items:
Food item
Calories[Kcal]
Total fat[g]
Sodium[g]
Branded Potato Chips
Serving
size
50 g
0.39
Added
sugar[g]
1
Saturated
fat[g]
5.35
272
17
Branded Aloo Bhujia
50 g
315
25
0.34
0
5
Branded Cola Drink
300 ml
132
0
0
33
0
Branded Instant Noodles
80 g
360
14
0.95
3.2
6.8
Branded Milk Chocolate
40 g
220
12
.045
21
8
Branded Non-carbonated
Fruit Beverage
Branded Aloo Burger
200 ml
146
0
0
34.6
0
155 g
352
14
0.84
8
NA
Source: Company websites primarily. Details mentioned in the annexure
Note 2: Sample menu options for healthy food (labeled green)
An indicative list of healthier sample menu options that could be categorised as green is provided below:
Table 10: Sample menu options with Kcal
Food items
Vegetable sandwiches (brown or multigrain
bread) {no mayonnaise, low fat cheese can
be used}
Fruit salad: 1 big katori
Single fruits (seasonal)
Chick pea vegetable chat 1 medium katori
Fruit custard 1 big katori
Veg poha 1 medium katori
Kcal
150200
Veg uttapam 1 medium
Vegetable pulao with veg raita; 1 medium
150
200
100
80-100
100
200
150
Food items
Paneer / chicken / egg / salami
sandwiches (brown or multigrain bread)
{no mayonnaise}(low fat cheese)
Fruit chat
Fruit yoghurts
Paneer/ vegetable cutlets 2 pc
Khandvi 2 pcs
Sprout salad 1 medium katori (sprouts
30g rest salad)
Veg upma 1 medium katori
Vegetable idlis with chutney: 2 pc
Kcal
200250
100
100
200
80
100
200
120
21
katori
Vegetable (whole wheat flour/multigrain
flour) kathi rolls: 1
150
Paneer/ chicken/egg (whole wheat
flour/multigrain flour) kathi rolls: 1
200
Table 11: Sample beverage options (200 ml) with Kcal
Beverages
Low fat milk shakes with seasonal fruits
(banana ,mango, cheeku , strawberry,
black current ) no added sugar
Fresh fruit juice
Smoothies with fruits
Kcal
180
Beverages
Fresh lime soda / shikanjee (with 10g
sugar)
Kcal
40
120
180
Badam milk
Salted / plain lassi
Jaljeera
180
120
60
22
Annexure 1
Details of HFSS food regulatory status across the world
Country
Regulation
Advertisements
(Bill proposed
but Pending)1
Details
In 2011, a bill to amend the ‘Broadcasting and Services Act,1992’ sought to:
Prohibit the broadcast or internet upload of ‘an unhealthy food
advertisement that is directed to children.’ Children are defined as ‘under
the age of 16 years’
Ban unhealthy food ads on commercial TV for select hours during
weekdays, weekends and holidays
Schools Ontario
(2011)2
As per the ‘School Food and Beverage Policy, 2010’, under the ‘Healthy
Food for School Act, 2008’:
‘Nutrition Standards’ are set for food and beverages sold in publicly
funded elementary and secondary schools. Food is divided into
vegetables and fruit, grain products, milk and alternatives, meat and
alternatives, mixed dishes (e.g., pizza, pasta, soup, salads, and
sandwiches), miscellaneous items and confectionery items (e.g., candy,
chocolate)
‘Nutrition Criteria’ based on ‘Nutrition Standards’ is outlined below for
schools:
Not permitted for sale: Contain few or no essential nutrients and/or
contain high amounts of fat, sugar, and/or sodium (e.g., deep-fried
and other fried foods, confectionery)
Sell most (≥ 80%): Healthiest options with higher levels of essential
nutrients and lower amounts of fat, sugar, and/or sodium. They must
make up at least 80 per cent of all food choices. Same requirement
applies to beverage choices
Sell less (≤ 20%): Mayhave slightly higher amounts of fat, sugar,
and/or sodium than food and beverages in the “sell most” category.
They must make up no more than 20 per cent of all food choices.
Same requirement applies to beverage choices
As per the ‘Broadcast Code for Advertising to Children’ under 12 years, in
relation to food products:
Advertisements must not convey to a child that they are a substitute
for meals
Advertisements ought not to be portrayed in a way that it becomes
excessive for a person to consume
The quantity of food shown should not exceed the labelling or
serving size
Australia
Canada
Advertisements
(1971)3
Schools (2012)5
Quebec (1978)4
The Sec.248 of ‘Consumer Protection Act’ bans all advertisements
targeting children aged 13 years and less.
Regulation brought up to restrict food products that are high in fat, sugar,
calories and low in nutrition
Chips, cookies, candy and carbonated sodas banned from elementary
and high school
Tax (2011)6
Imposed taxes on soft drinks, ice-cream, sweets, chocolates etc.
Costa Rica
Finland
23
Advertisements
(2007)7
France
Tax (2012)8
Hungary
Ireland
Tax (2011)9
Tax Under
progress10
Schools
(2006)11
Latvia
Schools
(2010)12
Lithuania
Advertisements
Under
progress13
Schools
(2011)14
Mexico
Tax (2013)15
Advertisements
(2010)16
New
Zealand
Advertisement for unhealthy food must carry health messages:
"For your health, avoid eating too many foods that are high in fat,
sugar or salt"
"For your health, avoid snacking between meals"
Companies that do not provide public health warnings are penalised with
about 1.5 % of their advertising budget
Tax introduced on sweetened non-alcoholic drinks, energy drinks etc. Zero
calorie ‘diet drinks’ are exempted.
Tax imposed on beverages, energy drinks, packaged sweets, ice cream,
jam, salty snacks and food flavorings
Extra taxes on sugary drinks proposed in 2011
One of the earlyEU countries to:
Prohibit foodstuffs and drinks that are high in sugar, salt, artificial
colorings and flavorings from kindergartens, primary and secondary
public schools
Replaced those with ‘healthy alternatives’ such as dried fruit, unsalted
nuts, unsweetened fruit juice, wholegrain snacks, mineral water and milk
Restriction on the supply of HFSS foods and products in schools and all
children establishments. Prohibition of foodstuffs with > 0.4 mg/100 g of
sodium
A draft law that prohibits advertisements of confectionery, soft drinks and
snacks on TV and radio programmes and in press publications intended for
children
Published guidelines in order to reduce the consumption of high calorie
foods within the basic school.
Apply to about 220,000 public and private primary and middle schools
serving 25 million children
Schools barred from serving or selling sugary sodas, juices or processed
snacks, including local favorites such as tamarind candies
Banned unhealthy less-processed foods include pork rinds, atole (a
sweetened corn starch-based beverage), fried tacos and tortas.
Exceptions for healthier versions include tortas made from beans,
avocado and cheese, or chicken and vegetables.
All tacos, burritos and salads are to be low in fat
Legislation passed to contain twin epidemics of obesity and Type 2 diabetes
Tax imposed on soft drinks, sports drinks and sugary beverages
It also calls for tax on flavored beverages as well as concentrates,
powders, syrups, essences or flavor extracts
Advertisements for food and beverages that influence children aged under
14 years to adhere to the ‘Children’s Code for Advertising Food, 2010’ such
as:
Advertisements should not by implication, omission, ambiguity or
exaggerated claim mislead or deceive or be likely to mislead or deceive
children, abuse their trust or exploit their lack of knowledge without
reason play on fear
Persons or characters well-known to children shall not be used in
advertisements to promote food in such as way so as to undermine a
healthy diet as defined by the Food Nutrition Guidelines for Healthy
Children
24
Advertisements,
under progress
(2012)17
Norway
Schools
(2013)18
Peru
Advertisements
(2013)19
Tax
Under
progress20
Schools
(2007)21
Philippines
Schools
Under
progress22
Poland
The age limit is increased to 16 years from earlier set 12 years
Proposed to ban on advertisements of ‘unhealthy foods’ such as sodas,
cookies, chocolate, ice cream, greasy burgers, chewing gum with sugar,
yoghurt candies, sweet juices, sweetened milk drinks, and sugar cereals
Draft regulation on Marketing of Food and drink to children were
formulated. Section 4 of the Draft Regulations prescribes the prohibition
on marketing of unhealthy food and drink to children.
The law ‘Promoting Healthy Food for Children Act’ calls for
Healthy food in school kiosks or cafeterias
A system for monitoring nutrition, overweight, and obesity among
children and adolescents
Controls on advertising aimed at children and adolescents
Nutrition education in schools and more physical activity
The ‘Promoting Healthy Food for Children Act’ considers the age limit of 16
years and prohibits
Advertisements that encourage ‘immoderate consumption’ of food and
non-alcoholic beverages with HFSS and shows ‘inappropriate portions’
Suggests that parents are ‘more intelligent or more generous’ in
purchasing a particular product
Plans to introduce tax on foods that are high in fat, salt or sugarcontent
Through Guidelines issued by the Department of Education to the school
canteens in public elementary and secondary schools:
Prohibited sale of carbonated drinks, sugar based synthetic or artificial
flavored juices, junk foods and any food product that may be detrimental
to the child’s health
Foods allowed to be sold in school canteens include:
Only nutrient rich food like root crops, noodles, rice and corn
products in native preparation
Fruits and vegetables in season and fortified food products labeled
rich in protein, energy, vitamins and minerals
Milk, shakes and juices prepared from fruits and vegetables in
season
A bill is currently on hold until December 2013 for comments from EU
commission and member states. Once approved in its present form from 1
Jan 2014, it will ban the sale of foods and drinks with HFSS in
kindergartens, primary schools, secondary schools and other educational
and care institutions as follows:
Sweets and confectionery and bakery wares with sugar content
exceeding 10 g of added sugars in 100 g of product
Fast food, instant food, snacks with sodium > 300 mg in 100 g of product
Dairy products with added sugars > 15 g in 100 g/ml of product
Cereal products with added sugars > 25 g in 100 g of product
Jams, marmalades, highly-sweetened syrups with content of added
sugars > 50 g in 100 g of product
Carbonated and still beverages with added sugars and synthetic
colorings; Energy and isotonic drinks
Schools are also restricted to advertise, present and promote purchase of
any of the banned foods listed above
25
Advertisements
(2007)23
As per Article 9 of the ‘Combating Unfair Commercial Practices Act,
2007’,“In all circumstances, aggressive commercial practices shall be
regarded as unfair commercial practices: including in an advertisement a
direct exhortation to children to buy advertised products or persuade their
parents or other adults to buy advertised products for them”.
Advertising
(2008)24
The Ministerial Order 1563/2008addressing the
Approval of the list of foods, not recommended for preschool children and
school children.
The principles, underlying healthy diets for children and adolescents also
establishes the criteria for which specific food items should not be
recommended.
These food items are not allowed to be sold within school premises in
order to encourage schoolchildren to adopt healthy dietary habits.
Sale of junk food and drinks in school and surrounding areas is banned by
the Health Ministry
Ban on advertisement of foods with HFSS such as hamburgers, pizzas,
instant noodles, chocolate and other candies and ice cream
Such advertisements are banned from 5pm to 7pm on TV and from
children’s programme at any time of the day
As per the ‘Radio and TV Act’:
All TV advertisements directed to children aged under 12 years are
banned from the first day of the commercial TV broadcast
Amendments to regulate the fast food are proposed in the ‘Food Sanitation
Management Act’, and the draft of a ‘National Nutrition Law. If approved, the
draft would restrict:
Advertising on children’s channels between 4 p.m. and 6 p.m.
Marketing methods used for fast food, such as giving away toys with
meals
Conducting promotional activities for fast foods or snacks including
chocolate, potato chips, fried chicken, french fries, cola and other
sugared drinks
Financial penalties to be imposed in case of violations
As per the guidelines ‘Guide of Health and Nutritional Practices of School
Canteen’ by Dubai Health Authority and Dubai Municipality:
All public and private schools in the Emirate of Dubai, banned foods with
high caloric value, artificial flavors and poor nutritional value such as
crisps, burgers, chocolate and sugary drinks
The ‘Smart Snacks in Schools’ nutrition standards programme under the
‘Healthy, Hunger-Free Kids Act, 2010’ puts a ban on junk foods in
schools. It will replace it with healthier items on school menus by 201415 school year in all grade levels (elementary, middle and high school).
As of now several states have policies for competitive foods segregated
into ‘Foods of Minimal Nutritional Value’ (FMNV) and all other foods
offered for individual sale.
FMNV includes carbonated beverages, water ices, chewing gum,
hard candy, jellies and gums, marshmallow candies, fondant,
licorice, spun candy, and candy-coated popcorn.
Other competitive foods offered for sale in schools include foods
purchased through a la carte in the cafeteria, vending machines,
school stores, canteens, and snack bars.
Romania
South
Korea
Schools
(2009)25
Advertisements
(2010)26
Sweden
Advertisements
(1991)27
Advertisements
Under
progress28
Taiwan
United
Arab
Emirates
Schools
(2011)29
Schools
Implementation
planned in
Future30
United
States
26
Advertisements
Under
progress31
The Interagency Working Group constituted under the ‘Omnibus
Appropriations Act, 2009’, proposed two ‘Nutrition Principles’ based on
which marketing of foods to children aged 2-17 is to be done after 2016:
Meaningful contribution to a healthful diet
Nutrients with negative impact on health or weight
About 20 categories of advertising, marketing and promotional activities
are identified in the FTC’s food marketing study definitions. These
include:
television, radio, and print advertising
company sponsored web sites, ads on third-party Internet sites,
and other digital advertising, such as email and text messaging
packaging and point-of-purchase displays and other in-store
marketing tools
advertising and product placement in movies, videos, and video
games
premium distribution, contests, and sweepstakes
cross promotions, including character licensing and toy cobranding
sponsorship of events, sports teams, and individual athletes
word-of-mouth and viral marketing
celebrity endorsements
in-school marketing
Philanthropic activity tied to branding opportunities
Tax31
San Francisco (proposed, 2013)
Propose to Introduce tax on soda and sugar sweetened beverages
Schools
England (2006)32
Vending machines not allowed selling chocolates, crisps or fizzy drinks,
etc.
Low-quality fast food served in school canteens is also banned
United
Kingdom
Advertisements
(2008)34
Uruguay
Advertisements
(2013)35
Scotland (2008)33
Restricted savory snacks
Prohibited confectionary such as chocolate, chocolate products and
sweets
Prohibited sugary soft drinks, fizzy drinks etc.
Menus must not contain more than three deep-fried items in a single
week (including chips). Chips, if served, must be served as part of a
meal.
The Ofcom, an independent regulator along with Department of Health and
Food Safety Agency put:
Ban on advertisements of HFSS food and drinks in and around
programmes for under 16 (including pre-school children)
Restrictions on programmes sponsored by food and drink products that
are HFSS
Restrictions on use of celebrities, cartoon characters and free gifts as
incentives while promoting food and drinks that are HFSS
The newly approved ‘Healthy Diets in Educational Units’ law bans
advertising to children in school
27
Annexure 2
Nutrient Profiling Model of the United Kingdom and Scoring36
Step 1: Total A points
A maximum of ten points can be awarded for each nutrient. Total 'A' points = (points for energy) + (points
for saturated fat) + (points for sugars) + (points for sodium). The table below indicates the points scored,
depending on the amount of each nutrient in 100g of the food or drink:
Points
Energy (kJ)
Sat Fat (g)
Total Sugar (g)
Sodium (mg)
0
1
≤ 335
> 335
≤1
>1
≤ 4.5
> 4.5
≤ 90
>90
2
> 670
>2
>9
> 180
3
> 1005
>3
> 13.5
>270
4
> 1340
>4
> 18
> 360
5
> 1675
>5
> 22.5
> 450
6
> 2010
>6
> 27
> 540
7
>2345
>7
>31
>630
8
>2680
>8
>36
>720
9
>3015
>9
>40
>810
10
>3350
>10
>45
>900
If a food or drink scores 11 or more ‘A’ points then it cannot score points for protein unless it also scores 5
points for fruit, vegetables and nuts
Step 2: Total C points
A maximum of five points can be awarded for each nutrient/food component. Total 'C' points = (points for
% fruit, vegetable & nut content) + (points for fibre [either NSP or AOAC]) + (points for protein). The table
below indicates the points scored, depending on the amount of each nutrient/food component in 100g of
the food or drink:
Points
Fruit, Veg & Nuts (%)
Protein (g)
NSP Fibre ' (g)
Or AOAC Fibre '
(g)
0
≤ 40
≤ 1.6
≤ 0.7
≤ 0.9
1
>40
>1.6
>0.7
>0.9
2
>60
>3.2
>1.4
>1.9
3
-
>4.8
>2.1
>2.8
4
-
>6.4
>2.8
>3.7
5
>80
>8.0
>3.5
>4.7
*The nutrient profiling model was developed using NSP fibre intake; where the NSP value is not known,
AOAC fibre values can be used.
Step 3: Overall score
Overall score = Total ‘A’points – Total ‘C’ points
• If a food scores less than 11 ‘A’ points then the overall score is calculated as follows:
Total ‘A’ points (energy + saturated fat + sugars + sodium) Minus Total ‘C’ points (fruit, veg and nuts +
fibre + protein)
28
• If a food scores 11 or more ‘A’ points but scores 5 points for fruit, vegetables and nuts thenthe
overall score is calculated as follows:
Total ‘A’ points (energy + saturated fat + sugars + sodium) Minus Total ‘C’ points (fruit, vegetable and
nuts + fibre + protein)
• If a food scores 11 or more ‘A’ points, and less than 5 points for fruit, vegetables and nuts, then
the overall score is calculated as follows:
Total ‘A’ points (energy + saturated fat + sugars + sodium) Minus Points for fibre + points for fruit,
vegetables and nuts (not allowed to score for protein)
Assessment of the final score
A food is classified as 'less healthy' where it scores 4 points or more
A drink is classified as 'less healthy' where it scores 1 point or more
A food is not be subjected to advertising restriction if it scores 4 points or more and a drink scores less
than 1 point or more. A set of commonly available packed and non-packed foods are scored based on the
UK model. The scores depict that such foods can easily be categorised as ‘HFSS Food’ foods.
While scoring:
Nutrition values are primarily taken from respective Indian company websites. However, in few
cases where it is not available, respective US websites or a third party independent websites are
referred. In all cases sources are mentioned.
Conversion per 100 g is done with simple mathematical calculations
Energy in Kcal converted to energy KJ (1Kcal=4.184 kJ)
Content of fruit vegetable and nuts assumed to be <=40% wherever applicable
No scoring is done for proteins wherever total 'A' points are equal to or more than 11 (as per
scoring criteria of the model)
Table: Branded chips and Aloo Bhujia
Branded chips
Energy(kJ)
Saturated fat (g/100g)*
Total sugar (g/100g)
Sodium (mg/100g)
Nutrition
information
2276
Score
Branded Aloo Bhujia
Score
6
Nutrition
information
2552
5.35
5
10
9
2
0
0
0
770
8
670
7
Total A Points
19
8
24
Fruit, vegetable & nuts (%)
≤ 40
0
≤ 40
0
Fibre (g/100g)*
4.46
5
20
5
Protein (g/100g)
7.8
0
5
0
Total C points
Final Score: A-C
5
5
14
19
Source:*hfritolay.com; pepsicoindia.co.in; : haldiram.com
29
Table: Branded Aloo Burger and Vegetable Burger
Branded Aloo Burger
Nutrition
information
941.4
Score
Saturated fat (g/100g)
Branded Vegetable Burger
Score
2
Nutrition
information
1184
2.14*
2
5.88
5
Total sugar (g/100g)
5.12
1
5.06*
1
Sodium (mg/100g)
538
5
636
7
Energy(kJ)
Total A Points
3
10
16
≤ 40**
0
≤ 40
0
NSP fibre (g/100g)
2.56
3
2.56*
3
Protein (g/100g)
5.12
0
10.18
0
Fruit, vegetable & nuts (%)
Total C points
3
3
Final Score: A-C
7
13
Source:mcdonaldsindia.net; * Information not mentioned on Indian and US company website. Calculated based on same brand
potato fries from an independent website. ** Assumed to be less that 40% (by weight) based on ingredients; potato is not
considered a vegetable as per the model;www.kfc.co.in;
Table: Branded Cola Drink 1, Branded Cola Drink 2 and non Carbonated fruit beverage
Branded Cola Drink Branded Cola Drink 2
Non-carbonated Fruit
1
Beverage
Nutrition
information
184
Score
Score
0
Nutrition
information
184
Saturated fat (g/100g)
0
0
Total sugar (g/100g)
11
Sodium (mg/100g)
0
Energy(kJ)
Total A Points
Score
0
Nutrition
information
305.43
0
0
0
0
2
11
2
17.3
3
0
0
0
0
0
2
2
0
3
Fruit, vegetable & nuts (%)
0
0
0
0
15
0
NSP fibre (g/100g)
0
0
0
0
0
0
Protein (g/100g)
0
0
0
0
0
0
Total C points
0
0
0
Final Score: A-C
2
2
3
Source: pepsicoindia.co.in ; coca-colaindia.com;pepsicoindia.co.in; specific gravity considered same as water
Table: Branded Milk Chocolate
Branded Milk Chocolate
Nutrition information
Score
30
Energy(kJ)
2301
6
20
10
Total sugar (g/100g)
52.5
10
Sodium (mg/100g)
1125
1
Saturated fat (g/100g)
Total A Points
27
Fruit, vegetable & nuts (%)
0
0
NSP fibre (g/100g)
2.5
3
Protein (g/100g)
7.5
0
Total C points
3
Final Score: A-C
24
Source: caloriecount.about.com; required nutritional information is not available on company website
Calculations based on the Cut-off developed
Based on the threshold values of calories and individual nutrients as mentioned above, various snack and
meal foods available in the India are evaluated. A red/bold figure in the tables below highlights that the
thresholds are exceeded vis-à-vis respective nutrient or calories. A food exceeding the threshold of one
nutrient or calories is considered unhealthy.
Simple calculations are done based on the criteria depicted above. Most of the data is from respective
product websites. Only in few cases, where information is not available on respective company websites,
independent third party website is referred. In all cases, sources are mentioned. Simple mathematical
calculations are used to arrive at figures for the serving size.
Table: Common Snack foods – Packed
Common Snack foods – Packed
Food item
Serving
size
50 g*
Calories[Kcal]
Total fat[g]
Sodium[g]
272
17
50 g*
315
Branded Cola Drink 1
300 ml
Branded Cola Drink 2
Branded Potato
Chips
Branded Aloo Bhujia
Branded Instant
Noodles***
Branded Milk
Chocolate
Branded Noncarbonated Fruit
Beverage
0.39
Added
sugar[g]
1
Saturated
fat[g]
5.35**
25
0.34
0
5
132
0
0
33
0
300 ml
132
0
0.05
33
0
80 g
360
14
0.95
3.2
6.8
40 g
220
12
.045
21
8
200 ml
146
0
0
34.6
0
Source:* Serving size considered as 50 gms; ** Company website US; ***Independent website – caloriecount.com as information on
respective website is not available caloriecount.about.com ; pepsicoindia.co.incaloriecount.about.com ; coca-colaindia.com;
pepsicoindia.co.in ; haldiram.com ; pepsicoindia.co.in
31
Table:Common Snack foods - Non Packaged
Common Snack foods - Non Packaged
Food item
Branded Aloo Burger
Branded Vegetable
Burger
Branded Chicken
Burger 1
Branded Chicken
Burger 2
Branded Pizza
(Personal)
Branded Potato Fries 1
(Regular )
Branded Potato Fries 2
(Regular )
Serving
size
155 g
Calories[Kcal]
Sodium[g]
Sugar[g]
352
Total
fat[g]
14
0.84
8
Saturated
fat[g]
NA
188.3 g
534.8
24.99
1.2
NA
11.7
163 g
407
19
1.01
5
NA
195.8
463
21.3
0.97
NA
6.46
(110 g) 2
slices
110 g
288.2
4.84
0.5
1.48
2.86
343
17
0.26
0
NA
73.5 g
216.4
9.94
0.12
0
3.8
Source: mcdonaldsindia.net ; kfc.co.in;; pizzahut.co.in
Table: Branded Meal 1
Serving size
Calories[Kcal]
Total fat[g]
Sodium
[g]
Sugar[g]
Saturated
fat[g]
Branded Aloo Burger
155 g
352
14
0.84
8
NA
Branded Potato Fries
1 (Regular )
Branded Cola Drink 2
110 g
343
17
0.26
0
NA
300 ml
132
0
0.05
39
0
827
31
1.15
47
Total
Source: mcdonaldsindia.net ; .coca-colaindia.com
Table : Branded Meal 2
Serving size
Branded Chicken
Burger 2
Branded Potato Fries
2 (Regular )
Branded Cola Drink 2
Total
Calories[Kcal]
Total fat[g]
Sodium
[g]
Added
sugar[g]
Saturated
fat[g]
195.8
463
21.3
0.97
0
11.7
73.5 g
216.4
9.94
0.12
0
3.8
300 ml
132
0
0.05
33
0
811.4
31.24
1.14
33
15.5
Source: kfc.co.in ; www.kfc.co.in ; .coca-colaindia.com
32
Annexure 3
Model school canteen policy - Australia
Australia37
The National
Healthy
School
Canteen
(NHSC)
guidelines,
2010
The National Healthy School Canteens Guidelines for healthy foods and
drinks supplied in Australian school canteens is based on the current 2013
Australian Dietary Guidelines, which gives advice on the quality and quantity
of foods and drinks recommended for children in Australia to achieve
optimal health and limit the risk of chronic diseases related to poor nutrition
in adulthood. Foods and drinks have been classified according to the
amount of nutrients they provide and are classified as green amber and red
category.
Green: always on the menu: These foods and drinks are the best choices
for a healthy school canteen. A large variety of these foods and drinks must
be available every day and be the main choices on the menu. They contain
a wide range of nutrients and are generally low in saturated fat and/or sugar
and/or sodium (salt).
Amber: Select carefully: These foods and drinks contain some valuable
nutrients, moderate amounts of saturated fat and/or sugar and/or sodium
(salt) and if eaten regularly or in large amounts, may contribute to excess
energy
(kilojoules)being
consumed.
These foods and drinks must be assessed carefully against the Nutrient
Criteria Tables to ensure that:
• The healthiest choices from this category are selected
• These foods and drinks must not dominate the menu
• The serve size must be small
Red: not on the menu: These foods and drinks must not to be sold or
provided in schools, unless part of a special whole school event. These
foods and drinks may contain excess energy (kilojoules) and/or saturated fat
and/or sodium (salt) and/or sugar and are low in nutritional value
33
Annexure 4
Minutes of Meeting of Working Group set up by the Expert Group set up as per
the order dated September 4, 2013 of the Honorable High Court of Delhi on
guidelines for making available quality and safe food in schools
Date: January 8, 2014
Time: 3:00 PM to 5:30 PM
Place: Centre for Science and Environment, India Habitat Centre, New Delhi
Chair
Dr Sunita Narain, Director General, Centre for Science and Environment, Delhi
Participant Members
1. Dr Anju Seth, Professor, Dept. of Paediatrics, Lady Hardinge Medical College, Delhi
2. Ms Anuja Aggarwal, Nutritionist, AIIMS, Delhi
3. Dr Mridul Salgame, National Restaurant Association of India
4. Mr N Ramasubramanian, Retailers Association of India
5. Dr Rekha Harish, Professor and HoD, Dept. of Paediatrics, Government Medical College, Jammu
(participated via video conference)
6. Mr Sunil Adsule, National Restaurant Association of India*
7. Mr Sanjay Khajuria, All India Food Processors’ Association*
8. Dr Umesh Kapil, Professor, Public Health Nutrition, AIIMS, Delhi
Members not present**
1. Dr Jagdish Chandra, Professor, Dept. of Pediatrics, Lady Hardinge Medical College, Delhi
2. Dr K Damayanti, Scientist C, National Institute of Nutrition, Hyderabad
3. Ms Kumkum Marwah, Representative, Advisor Nutrition, Ministry of Health and Family Welfare
4. Dr P S M Chandran, Retailers Association of India
5. Dr S Jindal, All India Food Processors Association*
*New members of the Working Group as per the Expert Group Meeting of 13 December 2013
** Mr S K Sudhakar, Assistant Director at FSSAI, invited by the Chair of the Working Group as an
observer, was not present
34
Minutes
1. The Chair welcomed members of the Working Group and apprised about the new document
‘Guidelines on Wholesome Food and Nutrition for School Canteen’ (guideline 2) that was circulated
by Dr Mridul Salgame on behalf of the three Industry Associations. The Chair then requested to
present this document for the benefit of all members.
2. Dr N Ramasubramanian explained the contents and rationale of the document in detail. Mr Sanjay
Khajuria, Mr Sunil Adsule and Dr Salgame also shared their point of view on certain parts of the
document such as:
Indicative List of Recommended Foods in schools
Eat Less/Eat Just Right/Eat judiciously/ Eat Least/ Eat moderately/Eat responsibly: - Foods in
schools
Improving wholesomeness of foods made available in Schools
Implementation setup –for making available quality and safe food in schools - “The School
Health Team”
3. The Chair requested comments from respective members of the Working Group, which were shared
and discussed at length.
4. Dr Umesh Kapil expressed concern on implementation and monitoring of proposed guidelines. He
mentioned that it would be impractical to monitor the conversion of unhealthy junk food to healthy
food at school level. Referring to a majority of schools lacking canteens, he suggested that the focus
should not be on recipes. As a practical approach, he emphasised on defining ingredients and setting
their upper limits to categorize foods that should be banned in schools and nearby area of about 500
meters. He also requested for clarification in proposed guideline related to eating less/just
right/judiciously/least/moderately/responsibly and stressed on the importance of cut-offs developed in
the previous document (circulated by the Working Group and discussed in the Expert Group meeting
of 13th Dec 2013). He requested the Chair to consider banning junk foods completely from schools
and 500 meters near-by.
5. Responding to the point made by Mr Adsule on empowerment of school health teams that are
proposed to be set up to implement, Dr Kapil mentioned that such programs exist since 1962 under
state governments and take care of health issues. It may not be practical to create new health team/
program for this purpose. Dr Salgame mentioned that the existing health teams may not be well
oriented to nutrition and safety aspects and that this needed to be incorporated as suggested in the
guideline 2.
6. In her response to the content of the new document, Dr Anju Seth mentioned that it has no mention of
the rising incidence of obesity and other related NCDs and their correlation to junk food. Referring to
the criteria for categorising foods as mentioned in the previous document, she raised her concern
about the lack of specifics in the new document and the importance of it in monitoring the guidelines.
She also advised that no amount of exercise can negate problems due to over eating.
7. Dr Rekha Harish mentioned that she endorses the previous document. She stated that the new
document is descriptive but does not reflect well on quantitative aspects that are most required in this
context. It does not provide specific information on the amount, proportion, frequency and other
objective criteria around foods and ingredients as mentioned in the previous document. She
emphasised that HFSS foods (foods high in fat, salt, sugar as defined by WHO) are the key concern
35
and there is no mention of limits of saturated fat, trans-fatty acids, salt and sugar in new document. It
also fails to establish a link between ‘food pyramid’ and ‘traffic light’ concept proposed earlier and
does not talk about associated co-morbidities. She raised her concern on the ambiguity on eating
less/just right/judiciously/least/moderately/responsibly as stated in the new document. She opined
that it would be difficult for parents, schools, students to understand and apply this. They would not
get a sense of what is to be eaten and how much.
8. Dr Rekha also appreciated the proposed concept of greening of foods in the circulated guidelines 2
(improving the nutrition content of certain foods), particularly, about the proposed low/mild calorie
options for beverages e.g. nimbu pani that would be replacing the carbonated beverages. Referring to
the WHO fact sheet on obesity, she elucidated the role that food industry can play in limiting salt,
sugar and fats in foods and in responsible food marketing. She also expressed her satisfaction on
the mentioning of physical activity in the new document.
9. Ms Anuja Aggarwal commented that an objective criterion to classify foods is mandatory to formulate
guidelines for junk food. With reference to the new document, she pointed out the lack of clarity in
determining what is eating less/just right/judiciously/least/moderately/responsibly. She requested if it
could be provided to all members of the Working Group.
10. Mr Adsule, mentioned that MDMS (Mid-day Meal Scheme) has cut-offs of ingredients and could be
referred to address the issue on objectivity. Dr Kapil suggested that MDMs is for a specific objective
that addresses a deficit. The issue at hand is about junk food which is available in schools and
nearby. The two issues are separate. Dr Rekha further explained that MDM is given to those who are
often under-nourished with no access to green leafy vegetables. It also aims to increase the school
attendance. The schools that are of concern in this case do not have MDMs. She agreed with Dr
Kapil that both issues should not be mixed.
11. Mr Khajuria, Mr Adsule and Dr Salgame mentioned that the new document addresses the Terms of
Reference (ToR) set for the Working Group in the first meeting of the Expert Group (held on 25
September, 2013). They said that certain parts of the previous guidelines (guideline 1) were beyond
the ToR. Mr Adsule also mentioned about the dual issue of over and under nutrition. Dr Seth
mentioned that the new document does not address the original Public Interest Litigation (PIL) and
the Court order (dated 4 September, 2013) that focus on the problem of over nutrition. Mr Khajuria
and Dr Salgame submitted that they are there to discuss ToR and not the court order, which could be
discussed at another platform. Dr Seth further mentioned that the petition was the origin of this issue.
Dr Kapil was of the view that the ultimate aim is healthy school children and the Court is specific on
junk food in its order. The Chair read out the ToR and mentioned that information and guidelines
presented in the previous document are based on the interpretation of Working Group members.
Specifically, the Chair explained the link between the assigned task ‘To examine the national and
global legislations/guidelines on Nutrition and Food Safety and efficacy of these
legislations/guidelines’ and the guidelines formulated on junk food regulation through advertising
and labelling.
12. Another concern raised by Mr Khajuria, Mr Adsule, Mr Subramanian and Dr Salgame was about the
list of foods shortlisted in the previous document, which was suggested to be banned from the
schools and nearby areas. Dr Seth explained that the selection is linked to the products about which
information is available, and therefore to begin with, the list mentioned comprise more of packed
and/or branded foods. The list can certainly be expanded to foods such as samosa and similar foods
going forward. In similar regard Mr Khajuria later mentioned about branded burger not being
36
promoted in the schools and checked about how guidelines would address the issue of burger that is
made in schools. The Chair took the Working Group through the guideline in the earlier document
that acknowledges the applicability of same criteria on standardised and non-standardised foods.
13. Referring to a study, Mr Adsule mentioned about smuggling of energy drinks in schools of London as
an adverse effect of banning such foods. The Chair mentioned about the need to deglamourize such
foods and thereby the importance of guidelines in the previous document related to regulating food
marketing and appropriate labelling in awareness generation.
14. Based on the discussion between Dr Kapil, Dr Rekha, Mr Adsule and Mr Khajuria it was agreed that
40-45 minutes of physical activity is to be promoted and be proposed as guidelines. Mr Adsule
proposed the need for rigorous activities such as sports. Dr Kapil and Dr Rekha mentioned about
absence of such recommendations. Further, Dr Rekha highlighted the duration of school period and
advised not to increase it beyond 40-45 minutes.
15. The chair summarised the discussion and acknowledged that there are synergies and meeting
ground between the new and previous document. The guideline 2 needs clarification on the issue of
how it would determine the limits for eat-least foods and what would be the way eat responsibly would
be quantified.
16. Summarising the gaps highlighted by respective members, the Chair mentioned that the new
document (guideline 2) does not define and quantify the criteria for categorising foods that are to be
consumed more or less. It also needs to provide a framework to help understand the concept of
eating less/just right/judiciously/least/moderately/responsibly and include limits for ingredients of
concern such as fat, salt, and sugar.
17. Points of agreement within members of the Working Group are:
The need for an implementable canteen policy in schools
That there are specific foods that should be consumed more by school children and
certain foods that should be consumed less
The need for an objective and quantifiable criteria based on which foods could be
categorised
The need to build awareness about the food choices among school children, parents and
community at large and to promote physical activity
18. Points where the representatives of Industry Associations disagreed with other members are:
The need to regulate the availability of certain foods in near-by areas (500 yards)
The need to restrict/ ban sale of food based on objective quantified criterion in schools
The need for guidelines related to promotion and labelling to build awareness in
consumers and restrict sale in society as a whole
19. Follow up action:
a) Representatives of industry association and experts to give clarification on the criterion/
framework to categorise food, on Monday, January 13, 2014.
b) As requested by Mr Adsule, Dr Umesh Kapil or Ms Anuja Aggarwal to share the source of figures
for recommended sugar intake
c) Members agreed that as of now, there is no need to request postponement of the Expert Group
meeting that is scheduled for 15, January 2014 at FSSAI. The chair would submit the revised
document based on the discussions and inputs received.
37
The meeting ended with a vote of thanks by the Chair.
Annexure 5
Guidelines on wholesome food and nutrition in school canteen submitted by
Industry representatives on January 3, 2014
Contents
1. Objective& Scope
2. Healthy Lifestyle
3. Balanced Diet
4. Basics and Importance of Nutrition
5. Importance of physical activity
6. Dietary Recommendations in schools
7. Improving wholesomeness of foods made available in Schools
8. Recommendations for Physical Activity
9. Implementation setup –for making available quality and safe food in schools - “The
School Health Team”
10. Awareness Generation
38
11.
1. Objective & Scope:
As per the Economic Survey of India 2012-13, there are more than 141Lakh schools throughout
India. These schools are of widely varying type - from fully air-conditioned school equipped with
all facilities - to those even without apucca roof; from residential boarding school - to those
where children need to walk/travel long distance every day to school; from schools with only
selling food counter- to those schools which serve meals in schools.
The objective of this guidance document is to guide, assist the school management, teachers,
students, vendors for making available quality and safe food in school covering all types of
schools and facilities cited above.
2. Healthy Lifestyle:
A healthy lifestyle is cornerstone of good health, physical fitness, energy and reduced risk for
disease. It is based on the choices one makes about his or her daily habits. Good nutrition, daily
exercise and adequate sleep are the foundations for continuing health lifestyle. A healthy
lifestyle includes diet based on balance, variety and moderation coupled with regular physical
activity commensurate with one’s age, gender and body constitution.
WHO Global Strategy on Diet, Physical Activity and Health urges:
2“to develop, implement and evaluate actions recommended in the Strategy, as
appropriate to national circumstances and as part of their overall policies and
programmes, that promote individual and community health through healthy diet and
physical activity and reduce the risks and incidence of non-communicable diseases;
3to promote lifestyles that include a healthy diet and physical activity and foster energy
balance;
4to encourage and foster a favourable environment for the exercise of individual
responsibility for health through the adoption of lifestyles that include a healthy diet
and physical activity”
Healthy lifestyle primarily covers two aspects:
Balanced Diet
Physical Activity
1
Economic Survey 2012-13, Source : Statistics of School Education- 2010-11 (Provisional)
Fifty Seventh World Health Assembly WHA 57.17 (22nd May 2004) - Clause 2(1)
3
Fifty Seventh World Health Assembly WHA 57.17 (22nd May 2004) - Clause 2(2)
4
Fifty Seventh World Health Assembly WHA 57.17 (22nd May 2004) - Clause 2(6)
2
39
3.
5Balanced
Diet: In order to meet the nutrient needs, everyone has to eat daily at least one
food item in sufficient quantity from each of the five food groups. Such a diet, in which
various foodstuffs are mixed in suitable proportions to carry out adequately the three
functions (body-building, energy-yielding and protective, is known as a “Balanced Diet”.
The essential nutrients are protein, carbohydrate, fats and the different minerals and vitamins.
Each has a special job in the building and upkeep of the body. Hence, all the nutrients in the
proper proportions are needed by the body. Almost all natural foodstuffs contain a mixture of
different nutrients. There is, however, no single foodstuff in which the nutrients are present in
quantities sufficient to meet the daily needs of the body. This is why a combination of different
kinds of foodstuffs is essential in a diet. Howeverdepending on the predominant nutrient
contained, foodstuffs may be broadly classified under three heads. viz. Energy yielding, Bodybuilding and Protective foods.
Body-building foodstuffs are milk and milk products, meat, fish, eggs, pulses, dried beads and
nuts. Cereals too, contain some body building materials. The nutrients that build and renew are
proteins and minerals. Some examples of protective foodstuffs are green leafy vegetables, fresh
fruit, milk, meat, fish and eggs. The nutrients that carry out this protective function are chiefly
the vitamins and mineral salts.
The energy-yielding foodstuffs are chiefly cereals, sugars, fats and oils. The energy is measured
in terms of calories.
If the diet is deficient in one or more of these vital substances, it leads to a derangement of the
normal functioning of the different parts of the body resulting in ill-health, stunted growth and
imperfect development. A no less important task of the protective nutrients is to enable us to
utilize the other food factors for the production of energy and help to build the body.
Knowledge about the nutrients contained in foods makes the job of food selection and
consumption more meaningful. Foods are store-houses of these nutrients. All foodstuffs can
therefore, be conveniently grouped as in Table 1 to help us in such a selection. The
predominant nutrient in foods listed in a particular group is the same. Within the same group,
foods can be exchanged for one another depending on the individual's likes and the local
availability (Table 1).
5
Some Common Indian Recipes and their Nutritive Value, National Institute of Nutrition, Hyderabad, 2011
40
3.1. 6Benefits of a Balanced Diet
Opting for a balanced, adequate and varied diet is an important step towards a happy
and healthy lifestyle.
Vitamins and minerals in the diet are vital to boost immunity and healthy development,
A healthy diet can protect the human body against certain types of diseases, in
particular non-communicable diseases such as obesity, diabetes, cardiovascular
diseases, some types of cancer and skeletal conditions.
Healthy diets can also contribute to an adequate body weight.
Healthy eating is a good opportunity to enrich life by experimenting with different foods
from different cultures, origins and with different ways to prepare food.
The benefits of eating a wide variety of foods are also emotional, as variety and colour
are important ingredients of a balance diet.
4. Basics and Importance of Nutrition:
Nutrient Requirements and Recommended Dietary Allowances for Indians – A Report of the
Expert Group of the Indian Council of Medical Research, 2010 recognizes that - Humans need a
6
http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthylifestyle/benefits-of-a-balanced-diet
41
wide range of nutrients to lead a healthy and active life. The required nutrients for different
physiological groups can only be derived from a well-balanced diet. Components of the diet
must be chosen judiciously to provide all the nutrients to meet the human requirements in
proper proportions for the different physiological activities. The amount of each nutrient
needed for an individual depends upon his/her age, body weight and physiological status.Young
children grow rapidly and require nutrients not only for maintenance but also for growth. They
require relatively more nutrients (2-3 times) per kg body weight than adults.
The paradoxical co-occurrence of under and over nutrition, is a characteristic of rapidly
developing economies like India making the matter more complex for policy makers to address.
Role of appropriate and adequate nutrition in case of children is very important for growth,
physical wellbeing and maintaining healthy body weight. Many of us do realize that what we
eat on a daily basis will influence how we feel, function, and look, but some do not have a firm
grasp over just how much it will really matter. Those who lack the nutrients they need,
especially during the high growth years of childhood may not reach full height and may not
develop quite as optimally as they should. Children in their formative years should be guided to
pay attention to their eating habits, physical activity and hygienic practices to lay foundation for
proper health moving them in adult and later adult years.
Improving nutrition contributes to productivity and cognitive development of a child by
improving health, physical work capacity and school performance. Following nutrients play vital
role in all round growth and development of children:
4.1 Carbohydrate: Carbohydrates are either simple or complex, and are major sources
of energy in all human diets. They provide energy of 4 Cal/g. The simple carbohydrates,
glucose and fructose, are found in fruits, vegetables and honey, sucrose in sugar and
lactose in milk, while the complex polysaccharides are starches in cereals, millets, pulses
and root vegetables and glycogen in animal foods. The other complex carbohydrates
which are resistant to digestion in the human digestive tract are cellulose in vegetables
and whole grains, and gums and pectins in vegetables, fruits and cereals, which
constitute the dietary fiber component. In India, 70-80% of total dietary calories are
derived from carbohydrates present in plant foods such as cereals, millets and pulses.
Food ingredients like simple sugars, namely cane sugar, glucose etc. are pure
carbohydrates. Starch is a complex carbohydrate made up of glucose units. Glucose
derived from starch and other sugars present in the diet is the main source of energy in
the body.
4.2 Dietary Fibre delays and retards absorption of carbohydrates and fats and increases
the satiety value. Diets rich in fibre reduce glucose and lipids in blood and increase the
bulk of the stools. Diets rich in complex carbohydrates are healthier than low-fibre diets
42
based on refined foods. Vegetable, particularly leafy ones, fruits, condiments & spices
and unrefined cereals are comparatively rich in fibre.
4.3 Protein: Proteins are primary structural and functional components of every living
cell. Almost half the protein in our body is in the form of muscle and the rest of it is in
bone, cartilage and skin. Proteins are complex molecules composed of different amino
acids. Certain amino acids which are termed “essential” have to be obtained from
proteins in the diet since they are not synthesized in the human body. Other
nonessential amino acids can be synthesized in the body to build proteins. Proteins
perform a wide range of functions and also provide energy (4 Cal/g). Protein
requirements vary with age, physiological status and stress. More proteins are required
by growing infants and children and individuals during infections and illness or stress.
Animal foods like milk, meat, fish and eggs and plant foods such as pulses and legumes
are rich sources of proteins. Animal proteins are of high quality as they provide all the
essential amino acids in right proportions, while plant or vegetable proteins are not of
the same quality because of their low content of some of the essential amino acids.
However, a combination of cereals, millets and pulses provides most of the amino acids,
which complement each other to provide better quality proteins.
4.4 Fat: Fat is an important component of diet and serves a number of functions in the
body. Oils and fats such as butter, ghee and vanaspaticonstitute dietary visible fats. Fats
are a concentrated source of energy providing 9 Cal/g. It also imparts palatability to a
diet and retards stomach emptying time. Presence of fat in the diet is important for the
absorption of fat soluble vitamins like Vitamin A and carotene present in the diet. It is
necessary to have adequate and good quality fat in the diet with sufficient
polyunsaturated fatty acids in proper proportions for meeting the requirements of
essential fatty acids. The type and quantity of fat in the daily diet influence the level of
cholesterol and triglycerides in the blood. Diets should include adequate amounts of fat
particularly in the case of infants and children, to provide concentrated energy since
their energy needs per kg body weight are nearly twice those of adults. Excess of these
substances could lead to obesity, diabetes, cardiovascular disease and cancer.
These essential fatty acids are also important for the structure and function of cells. Fats
in the diet can be of two kinds, the visible and invisible fat. The visible fats are those
derived from animal fats like butter, ghee and those derived from vegetable fats like,
groundnut, mustard, coconut, safflower, sunflower, Rice bran oil etc. Hydrogenated
vegetable fat is commonly known as vanaspati.
4.5 Vitamins: Vitamins are organic substances present in small amounts in many foods.
They are required for carrying out many vital functions of the body and many of them
are involved in the utilization of the major nutrients like proteins, fat and carbohydrates.
43
Although they are needed in small amounts, they are essential for health and well-being
of the body. Their deficiency can lead to serious illness.
Vitamins are broadly classified as:
Fat soluble vitamins – These can be stored in the body in small amounts. These
are Vitamin A (for good eyesight), Vitamin D (for strong bones), Vitamin K (for
blood clotting) and Vitamin E (for healthy skin).
Water Soluble Vitamins- These cannot be stored in body and hence these should
be taken in adequate amounts through our daily diet. These are Vit. B1, Vit. B2
and Niacin (for release of energy from food), Vit. B6, Vit. B12 and Folic Acid (for
healthy red blood cells) and Vit.C (for fighting infection and boosting immunity)
4.6 Minerals: A large number of minerals and trace elements are present in body. Some
of these form part of body structural component and some others act as catalytic agents
in many body reactions. For example Iron (an important component for blood required
for carrying oxygen in blood and building up stamina); Calcium, Phosphorous and
Magnesium (for strong bones); Sodium and Potassium (important elements present in
fluids required for electrolyte balance); Zinc, Selenium, Copper, Manganese,
Magnesium, etc. (are either structural part or activate a large number of enzyme
systems); Iodine (part of hormone thyroxine; etc.)
4.7 Water: Human beings can survive for some weeks without food, but without water
we would perish after only a few days. It is necessary for digestion and elimination of
waste products; regulation of body temperature and acts a lubricant for joints and eyes.
5. Importance of Physical Activity
Physical activity is defined as any bodily movement produced by skeletal muscles that require
energy expenditure. Regular moderate intensity physical activity – such as walking, cycling, or
participating in sports – has significant benefits for health. Most people know that physical
activity burns calories, which can help with weight management. The benefits of physical
activity - and health risks associated with inactivity - extend far beyond weight management. In
fact, few lifestyle choices have as large an impact on health and wellbeing as regular physical
activity. Research shows regular physical activity not only helps reduce the risk for, and
improves management of, heart disease and diabetes, it also helps improve sleep and stress
management.
There is widespread consensus that weight gain is primarily the result of an imbalance of
energy - specifically too many calories consumed and not enough calories expended. In order
to lose body weight you need to either burn more calories or consume fewer calories, or both.
This concept of balancing calories in and out is what the experts refer to as 'energy balance'.
When it comes to managing weight, it's important to balance the calories you take in with the
44
calories you burn by consuming a sensible, balanced diet combined with regular physical
activity.
For children and young people of this age group physical activity includes play, games, sports,
transportation, recreation, physical education or planned exercise, in the context of family,
school, and community activities.
6. Dietary Recommendations in Schools:
A balanced diet is one which provides all the nutrients in required amounts and proper
proportions. It can be achieved through a blend of the five food groups. The quantities of foods
needed to meet the nutrient requirements vary with age, gender, physiological status and
physical activity. A balanced diet should provide around 50-60% of total calories from
carbohydrates, preferably from complex carbohydrates, about 10-15% from proteins and 2030% from total fat.
6.1 Indicative List of Recommended7 Foods in schools: Following is the indicative8 list of the
foods recommended in school.
a)
W
hole Wheat Roti/Pooriwith Seasonal Vegetable
b)
M
ulti Whole Grain Roti/Pooriwith Seasonal Vegetable
c)
R
ice and Dal
d)
V
egetable Pulao
e)
R
ice & Black Chana
f)
W
heat Halwa with Black Chana
g)
S
weet Dalia
h)
R
ice & White Chana
i)
R
ice and Rajmah
7
Drawn from Mid-Day Meal Programme/ Supplementary Nutrition Programme of various State Governments in
India namely Delhi, UP, Haryana, Punjab, Tamil Nadu
8
Indicative: Depending upon the geography, seasonality, food habits the school food team may choose from this
list or replace with similar food options.
45
j)
K
arhiChawal
k)
B
ulgar wheat uppuma or Khichri/Greens and dhal kootu, Payasam,
Papaya/Tomato/Nellikai, egg
l)
T
amarind rice/Greens kootu with dhal /BalaharPayasam,
Papaya/Tomato/Nellikai, green gram
m)
D
hal rice, Greens and dhal kootu, BalaharPayasam, Papaya/Tomato/Nellikai,
Bengal Gram
n)
P
otato, rice, sambar
o)
I
dli, Wada, Sambar
S
p)
ambar and rice
q)
K
heer
r)
M
ilk and milk products like Curd, Butter milk, lassi
6.2 Eat Less/Eat Just Right/Eat judiciously/ Eat Least/ Eat moderately/Eat responsibly: Foods in schools:Over consumption of some foods may lead to dietary imbalance, hence
responsible /moderate consumption is suggested for students in schools. An indicative list
for reference purposes is as given below:
a)
D
eep fried Products
b)
P
izza
c)
B
urger
d)
N
oodle
e)
C
hocolate, candies
f)
C
arbonated Beverages
46
g)
I
ce Cream
7. Improving wholesomeness of foods made available in Schools
Ensuring safe and quality food in schools is a multi-dimensional challenge, which needs to be
addressed through various aspects by the School Health Team such as:
a) Ingredients:
E.g.
o Use of MUFA/PUFA rich oils such as mustard oil, rice bran oil, soyabean oil,
sunflower oil etc. instead of Vanaspati/Partially hydrogenated vegetable
oil/Hydrogenated vegetable oil.
o Use of whole grains/multi grains e.g. Atta etc.
o Use of potable water
b) Sourcing: to identify and select the sources of food ingredients.
c) Preparation and Processing: E.g. in CholeBhatura, bhatura may be prepared from
whole wheat flour, methi, palak or other seasonal vegetables, and the same may be
prepared in a manner which reduces oil absorption.
Samosa may be prepared using blend of vegetable/minced meat/poultry/egg and
through means of reducing fat absorption and/or baking.
d) Storage: Ensuring compliance to storage instructions (in terms of temperature, time,
shelf life) for ingredients/foods/prepared meals.
Food Safety Practices: As elaborated in these guidelines as well as conditions of
licensing and registration as notified by Food Safety and Standards Authority of India.
The list in 7.2 is indicative of the products which may still be consumed in a responsible
manner. These foods can be innovated to become a part of recommended food. Such
innovated food which fulfill is nutritious and good for children to fulfill their nutrition,
energy and taste requirements may be developed considering the following criterion.
9Following principles will go a long way in improving wholesomeness of not only above
foods in 7.2, but in general as well:
a)
R
educe trans-fats in foods to ensure trans-fat content from partially hydrogenated
vegetable oil (PHVO) meet WHO criteria of <1% energy in a diet in a day. For e.g.
using oils e.g. mustard oil, rice bran oil, soybean oil, groundnut oil etc. in place of
hydrogenated vegetable oil / partially hydrogenated vegetable oil for various
preparations such as deep fried products.
9
As per WHO
47
b) Limit energy intake from total fats and shift fat consumption away from
saturated fats to unsaturated fats; Use healthier oil options instead of bakery
shortening or PHVO.
c) Limit the use of free sugars in school meals. For e.g. replace sweetened curd /
lassi with unsweetened versions.
d) Restrict the use of non-iodized salt and progressively reduce the intake of
sodium.
e) Increase consumption of fruits and vegetables, and legumes, whole grains and
nuts etc.
To improve wholesomeness
Deep fried Products
Include from the food groups as appropriate:
- Whole grain or
Pizza
- Milk or
Burger
- Pulses or
Noodle
- Fruits or
Chocolate, candies
- Vegetables or
Carbonated Beverages
- Fish or
Ice Cream
- Meat or
- Poultry or
- Egg or
- Nuts etc.
Examplesof aforesaid principles in improving wholesomeness of foods are:
A
a)
b)
c)
d)
e)
f)
g)
loo tikki which is typically deep fried can also be prepared by baking.
Using whole grain options of breads, buns, porridges etc.
Pizza prepared from whole wheat base, cheese to taste and adequate toppings
of vegetables/meat/poultry/fish.
Adding adequate quantity of vegetables / poultry / meat / egg in preparations
such as noodles, sandwiches, burgers etc.
Chat, a very popular snack can be made more wholesome by adding sprouts or
using low salt options.
Serving Ice cream, chocolate, candies which are low in fat/sugar or containing
fruits/vegetable/nuts.
Low calorie/mid calorie options of beverages E.g. Nimbupaani using low or no
sugar.
8. Recommendations for Physical Activity
48
For children and young people, physical activity includes play, games, sports, transportation,
chores, recreation, physical education, or planned exercise, in the context of family, school, and
community activities. The recommendations to improve cardio-respiratory and muscular
fitness, bone health, andcardiovascular and metabolic health biomarkers are:
a) Children aged 5-17 should accumulate at least 60 minutes of moderate - to vigorousintensity physical activity daily. E.g. Team sports like Football, Cricket, Basketball, Tennis,
Badminton, KhoKho, Kabaddi.
b) Amounts of physical activity greater than 60 minutes provide additional health benefits.
c) Most of the daily physical activity should be aerobic. Vigorous-intensity activities should
be incorporated, including those that strengthen muscle and bone, at least 3 times per
week. E.g. Cycling, Running, Swimming, Roller skating
The term "physical activity" should not be mistaken with only "exercise". Exercise, is a
subcategory of physical activity that is planned, structured, repetitive, and purposeful in the
sense that the improvement or maintenance of one or more components of physical fitness is
the objective. Physical activity includes exercise as well as other activities like walking, strolling
in garden, walking the dog, taking the stairs, house chores and recreational activities which
involve bodily movement and are done as part of playing, working and active transportation.
Physical inactivity due to insufficient participation in physical activity during leisure time and an
increase in sedentary behavior during occupational and domestic activities e.g. Watching TV,
Play Video Games, Indoor Card Games, Console Gaming etc. should be limited.
9. Implementation setup –for making available quality and safe food in schools - “The School
Health Team”: With a strength of over 1410 lakh school with wide range of systems /
infrastructure available with them the only way to implement this, the requirement of making
available quality and safe food, is to have a dedicated “School Health Team” as described
below.
a. A “School Health Team” to be set up in each school by the School Principal
comprising of teacher(s), parent(s), student(s) & school canteen operator(s) –
having about 7 to 10 members who will coordinate, implement and monitor the
guidelines to make available quality and safe food to students in schools.
b. The School Health Team will decide the type of food to be prepared in the school
kitchen / canteen and select raw materials and ingredients required for the
same.
10
Economic Survey 2012-13, Source : Statistics of School Education- 2010-11 (Provisional)
49
c. For such schools where food is not prepared and is sourced from outside and
made availableto children in the school, the School Health Team will select the
items of food to be made available as per these Guidelines.
d. The School Health Team will ensure that food made available in schools meets
the food safety, hygiene and sanitation requirements as per these Guidelines.
e. The School Health Team will study the gaps and recommend to the School
Principal, the necessary infrastructural facilities as per these Guidelines.
f. The School Health Team will design physical activity programs for students taking
into account age, climatic and other environmental conditions.
g. The School Health Team will strengthen awareness generation as described
section 11.
Since the systems available in schools across the country differ widely, a School Health Team
will have a crucial role in rolling out these guidelines in the schools. The variations in locations,
climatic conditions, availability of primary food / agri-inputs and other regional factors, food
habits have to be considered at each location and selection of food and implementation haveto
be done accordingly.
School Health Team will be best unit to appreciate the circumstances, material available,
climatic conditions, activity levels of students and another facilities / limitations and will be the
best placed in the interest of the students
This School Health Team may avail expertise of external resources such as nutritionist, physical
activity trainers, public health specialist, food safety expert etc. This team shall be responsible
for ensuring that all recommendations given as part of this guidance document are duly
implemented.
10. Awareness Generation
Awareness regarding quality of food, nutrition requirements, balanced diet, physical activity,
food safety hygiene and sanitation; amongst all concerned – teachers, students, parents, food
handlers, canteen operators / vendors, is very important for achieving the objectives of these
guidelines on a continued basis. There is a need to develop conducive environment in schools
regarding seriousness on health concerns, food quality and safety. It is recommended that the
School Food Team will develop awareness material as suggested below.
a) Information Modules regarding Hygienic Practices for school canteens
b) Information Modules regarding Nutrition Fundamentals – knowledge about nutrition
50
c)Information Modules regarding Promotion of Physical Activity
d) Discussion Group Quiz program on nutrition, hygiene, physical activity
e) Display of pictorial on nutrition, hygiene, physical activity in schools
51
References
Section 2
1.
2.
Dietary guidelines for Indians: A manual; NIN 2011
Role of ghrelin in food reward.Addict Biol. 2012 January; 17(1): 95–107.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3298643/
http://www.paho.org/nutricionydesarrollo/wp-content/uploads/2012/05/Comment.-Toxic-truth-about-sugar.pdf
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Lustig, R. H, Schmidt, L .A, Brindi, C. D; The toxic truth about sugar, Nature, Vole 482
http://www.nature.com/nature/journal/v482/n7383/full/482027a.html%3FWT.ec_id%3DNATURE-20120202
Malik, V.S Sugar sweetened beverages and the risk of metabolic syndrome and type 2 diabetes: A meta
analysishttp://care.diabetesjournals.org/content/33/11/2477.full
Salt Intake and Hypertension: Walking the Tight Rope; Can J Cardiol 1997;17:272B
Harmful effects of dietary salt in addition to hypertension; Journal of Human Hypertension (2002) 16, 213–223
Seifert et al, Health effects of energy drinks on children, adolescents and Young adults. Pediatrics, Feb 14, 2011
Antioxidants: The truth about BHA, BHT, TBHQ and other antioxidants used as food additives. ISBN: 9781907119002
World Health Organization - NCD Country Profiles , 2011; http://www.who.int/nmh/countries/ind_en.pdf
Global status report on non communicable diseases 2010.World Health Organization;
http://whqlibdoc.who.int/publications/2011/9789240686458_eng.pdf
Childhood obesity and adult morbidities; Am J Clin Nutr 2010;91(suppl):1499S–1505S,
http://ajcn.nutrition.org/content/91/5/1499S.full.pdf
Prevalence of overweight and obesity amongst school children in Delhi, India; Asia Pac J Clin Nutr 2008;17 (4):592-596
http://apjcn.nhri.org.tw/server/APJCN/17/4/592.pdf
Time to effectively address hypertension in India// Indian J Med Res 137, April 2013, pp 627-631
14. Prevalence and determinants of hypertension among urban school children in the age group of 13- 17 years in, Chennai,
Tamilnadu; IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861. Volume 8,
Issue 3
15. Prevalence and Determinants of Hypertension among Urban School children in the Age Group of 13- 17 Years in, Chennai,
Tamilnadu ; http://www.omicsonline.org/prevalence-and-determinants-of-hypertension-among-urban-school-children-in-theage-group-of-years-in-chennai-tamilnadu-2161-1165.1000130.pdf
16. http://www.world-heart-federation.org
17. High prevalence of insulin resistance in postpubertal Asian Indian children is associated with adverse truncal body fat
patterning, abdominal adiposity and excess body fat.; http://www.nature.com/ijo/journal/v28/n10/full/0802704a.html
18. http://www.idf.org/diabetesatlas
19. Prevalence of Pediatrics Metabolic Syndrome (PMS) amongst Children in the Age Group of 6–18 Years belonging to High
Income Group Residing in National Capital Territory (NCT) of Delhi; Indian J Pediatr (2010) 77:1041;
http://medind.nic.in/icb/t10/i9/icbt10i9p1041.pdf
20. Mark D Huffman, Coronary heart disease in India; Centre for Chronic Disease Control, New Delhi, India
21. http://online.wsj.com/news/articles/SB30001424052702304644104579191682155932364
22. Proximity of Fast-Food Restaurants to Schools and Adolescent Obesity; Am J Public Health. 2009;
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2661452/
23. Childhood Obesity in Developing Countries: Epidemiology, Determinants, and Prevention;
http://edrv.endojournals.org/content/33/1/48.long
24. Consumption of lifestyle foods among shildren, Anoop Mishra and Seema Gulati 2010; Unpublished data, presented at CSE’s
south Asian media briefing on food safety and environmental toxins, march 29-30, 2012
25. Increasing Proclivity for Junk Food among Overweight adolescent Girls in District Kurukshetra, India;
http://www.isca.in/IJBS/Archive/v2i3/14.ISCA-IRJBS-2013-026.pdf
26. http://www.techsciresearch.com/2114http://www.techsciresearch.com/2104
27. http://www.downtoearth.org.in/content/ban-plastic-packaging-junk-food-products-himachal-pradesh-upheld#.UsJVoXO
Section 3
1.
Dietary guidelines for Indians, A manual, NIN, 2011
52
2.
3.
4.
https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/216094/dh_123492.pdf
Nutrient Requirements and recommended dietary allowances for Indians, ICMR
Inputs from members of the Working Group
Annexure
1. Protecting Children from Junk Food Advertising (Broadcasting and Telecommunications Amendment) Bill 2011,
http://www.aph.gov.au/Parliamentary_Business/Bills_Legislation/Bills_Search_Results/Result?bId=s827 ; Taking Preventative
Action – A Response to Australia: The Healthiest Country by 2020 – The Report of the National Preventative Health Taskforce,
Australian Government, 46 (Commonwealth of Australia 2010),
http://www.preventativehealth.org.au/internet/preventativehealth/publishing.nsf/Content/6B7B17659424FBE5CA25772000095458/$
File/tpa.pdf
2. Healthy food for healthy schools protocol, Halton District School Board,
http://www.hdsb.ca/ParentInfo/Ontario%20Nutrition%20Standards%20for%20Schools/Healthy%20Food%20for%20Healthy%20Sch
ools%20Protocol%202011.pdf ; School food and beverage policy, October 4, 2010,
http://www.edu.gov.on.ca/extra/eng/ppm/ppm150.pdf
3. Broadcast Code for Advertising to Children – The Code,
http://www.adstandards.com/en/clearance/childrens/broadcastCodeForAdvertisingToChildren-TheCode.aspx#social
4. Consumer Protection Act, Quebec,
http://www2.publicationsduquebec.gouv.qc.ca/dynamicSearch/telecharge.php?type=2&file=/P_40_1/P40_1_A.html
5. UNSCEO, Restriction on Sale of Unhealthy foods in School Cafeterias are Established in Costa Rica,
http://portal.unesco.org/geography/en/ev.php-URL_ID=15181&URL_DO=DO_TOPIC&URL_SECTION=201.html
6. Food taxation in Europe: Evolution of the legislation, European Public Health Alliance, http://www.epha.org/spip.php?article4814
7. Dr Rhonda Jolly, Marketing Obesity? Junk Food, Advertising and Kids, 12th January 2011,
http://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp1011/11rp09#_Toc2826095
30; http://www.epha.org/spip.php?article2554
8. Food taxation in Europe: Evolution of the legislation, European Public Health Alliance, http://www.epha.org/spip.php?article4814;
Perkins, E. C., France’s New Sugary Drink Tax Take Effect Jan.1, Jan 01 2012, Digital Journal
http://digitaljournal.com/article/317037
9. Food taxation in Europe: Evolution of the legislation, European Public Health Alliance, http://www.epha.org/spip.php?article4814;
EU Food Law, Hungary hikes taxes, adds beer, alcopops and jam, 13th Dec. 2011,http://www.eurofoodlaw.com/policy/tax/hungaryhikes-taxes-adds-beer-alcopops-and-jam--1.htm ; EU Food Law, Hungary adopts chip Tax, 15th July
2011http://www.eurofoodlaw.com/policy/tax/hungary-adopts-chip-tax-18592.htm
10. Food taxation in Europe: Evolution of the legislation, European Public Health Alliance, http://www.epha.org/spip.php?article4814
11. Promotion of healthy food in Latvia’s schools, European Public Health Alliance, http://www.epha.org/spip.php?article2350 ; Ban on
junk-food sales in Latvian schools, 09 November 2006,http://www.euractiv.com/health/ban-junk-food-sales-latvian-scho-news217407
12. Marketing of foods high in fat, salt and sugar to children: update 2012–2013 (WHO Regional Office for Europe, Copenhagen,
Denmark : 2013) http://www.euro.who.int/__data/assets/pdf_file/0019/191125/e96859.pdf
13. Marketing of foods high in fat, salt and sugar to children: update 2012–2013 (WHO Regional Office for Europe, Copenhagen,
Denmark : 2013) http://www.euro.who.int/__data/assets/pdf_file/0019/191125/e96859.pdf
14. MEXICO CITY: putting the brakes on Junk Foods in Schools, http://peavyblack.com/2012/08/20/mexico-city-putting-the-brakes-onjunk-foods-in-schools/
15. ELINOR COMLAY, Coke Femsa shares fall as Mexico passes food, drink taxes, Thu Oct 31,
2013,http://www.reuters.com/article/2013/10/31/us-mexico-sodatax-idUSBRE99U16120131031
16. Children’s Code For Advertising Food 2010, Advertising Standards Authority, http://www.asa.co.nz/code_children_food.php
17. Norway: Tightening of Restrictions on Unhealthy Food Ads Aimed at Youth, Library of Congress,
http://www.loc.gov/lawweb/servlet/lloc_news?disp3_l205403682_text ; Alex Jhonston, Sorry Norway Food Companies, No More
Greasy Burger Ads for Kids, Dec. 11 2012 http://www.theepochtimes.com/n2/world/sorry-norway-food-companies-no-more-greasyburger-ads-for-kids-323868.html
18. Peruvian government promotes healthy food for children, says president, Lima May 16,
2013,http://www.presidencia.gob.pe/peruvian-government-promotes-healthy-food-for-children-says-president ; Latin American
53
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
countries crack down on junk food, The Lancet, Volume 382, Issue 9890, 385 - 386, 3 August
2013,http://download.thelancet.com/pdfs/journals/lancet/PIIS0140673613616578.pdf
Latin American countries crack down on junk food, The Lancet, Volume 382, Issue 9890, 385 - 386, 3 August
2013,http://download.thelancet.com/pdfs/journals/lancet/PIIS0140673613616578.pdf
'Fat tax' on unhealthy food must raise prices by 20% to have effect, says study, The Guardian, Wednesday 16 May 2012
http://www.theguardian.com/society/2012/may/16/fat-tax-unhealthy-food-effect ; Manuel Vigo, Peru could impose tax on junk food,
Jan. 2 2012 http://www.peruthisweek.com/news-1282-Peru-could-impose-tax-on-junk-food/
Department of Education, Philippines, http://deped.gov.ph/index.php/issuances/depedorders/2007/document/dos200708pdf?limit=100&format=raw
EU Food Law, Poland to ban junk foods in schools, Sept. 27 2013, http://www.eurofoodlaw.com/country-reports/eu-memberstates/poland/poland-to-ban-junk-foods-in-schools--1.htm (need to register)
The Act of 23 August 2007 on combating unfair commercial practices, Journal of Laws No. 171 of 2007, item 1206
https://www.google.co.in/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&ved=0CCoQFjAA&url=http%3A%2F%2Fwww.uok
ik.gov.pl%2Fdownload.php%3Fplik%3D7636&ei=WwegUvucMoebigf4yYCQDQ&usg=AFQjCNEyRxdALvn4tS5DJsSFbPygnc2XtQ&
bvm=bv.57155469,d.aGc
Marketing of foods high in fat, salt and sugar to children: update 2012–2013 (WHO Regional Office for Europe, Copenhagen,
Denmark : 2013) http://www.euro.who.int/__data/assets/pdf_file/0019/191125/e96859.pdf ; Ministry of Public Health. Ordin Nr. 1563
din 12 eptembrie 2008 [Ministerial Order No.1563 of 12 September 2008]. Official Journal for Romania, 2008, 651
http://str.calificativ.ro/news/preview/alimente_nerecomandate-1528.pdf
South Korea restricts TV ads for junk, Jan. 19 2010, http://www.telegraph.co.uk/expat/expatnews/7025149/South-Korea-restrictsTV-ads-for-junk.html; Schools Nationwide Ban Junk Foods, Jan 24 2009,
http://timescampus.ebse.co.kr/kids_ebs.htm?NID=89&code=ebs_headline
South Korea restricts TV ads for junk, Jan. 19 2010, http://www.telegraph.co.uk/expat/expatnews/7025149/South-Korea-restrictsTV-ads-for-junk.html
Evolution of the legislation in European countries, European Public Health Alliance, http://www.epha.org/spip.php?article2554; The
Radio and TV Act (1996:844), http://www.nonpubenfants.org/IMG/pdf/Loi_suedoise.pdf
The Amendment to Act Governing Food Sanitation Imposes Comprehensively Stricter Penalties on Non-Compliant Businesses,
Food & Drug Administration, Ministry of Health & Welfare, http://www.fda.gov.tw/EN/newsContent.aspx?id=9917&chk=2f6ee6587ee6-4361-a9e1-b53b4bf6fcbf ; Draft amendment to strengthen food safety approved, Executive Yuan, Republic of China (Taiwan),
Dec. 21 2013 http://www.ey.gov.tw/en/News_Content2.aspx?n=1C6028CA080A27B3&s=3D6A0D7AC95A64E1 ; Taiwan fast food
ads to be restricted, Jan 11 2013, http://www.taiwantoday.tw/ct.asp?xItem=200720&ctNode=445
Guide to Health and Nutritional Practices of School Canteens, Dubai Municipality, Dubai Health Authority,
http://www.dm.gov.ae/wps/wcm/connect/0f9efc3b-ac2d-4169-a426-170e55a02c06/School+canteens.pdf?MOD=AJPERES ; DHA
and Dubai Municipality issue healthy nutritional guidelines for all schools in Dubai, Government of Dubai, May 22nd 2011
http://www.dha.gov.ae/En/media/news/pages/dhaanddubaimunicipality.aspx
Smart Snacks in School – USDA’s “All Foods Sold in Schools” US Department of Agriculture
http://www.fns.usda.gov/cnd/governance/legislation/allfoods_flyer.pdf ; Smart Snacks in School, Food And Nutrition Service, US
Department of Agriculture http://www.fns.usda.gov/cnd/governance/legislation/allfoods.htm ; School Meals, Food and Nutrition
Service, US Department of Agriculture http://www.fns.usda.gov/cnd/menu/fmnv.htm ; School Meals Programmes - Competitive
Foods Are Available in Many Schools; Actions Taken to Restrict Them Differ by State and Locality, United States General
Accounting Office, April 2004 http://www.gao.gov/assets/250/242132.pdf
Food for Thought, Interagency Working Group on Food Marketing to Children,
http://ftc.gov/os/2011/04/110428foodmarketfactsheet.pdf
Oct 29 2013, San Francisco joins sugary drinks fray with tax proposal, http://www.reuters.com/article/2013/10/29/us-usa-sodacalifornia-idUSBRE99S19F20131029 ; 'Big Soda' set to outspend foes over tax, http://www.sfgate.com/bayarea/article/Big-Sodaset-to-outspend-foes-over-tax-5044936.php
BBC News, Junk food to be banned in schools, September 28th 2005 http://news.bbc.co.uk/2/hi/uk_news/education/4287712.stm ;
U.K. Bans Soft Drinks, Junk Food From School Vending October 10, 2005 http://www.preparedfoods.com/articles/u-k-bans-softdrinks-junk-food-from-school-vending; Junk food banned in maintained schools is being sold in academies, Monday 10 September
2012, http://www.theguardian.com/education/2012/sep/10/junk-food-academy-schools-claims
Healthy Eating in Schools - A Guide to Implementing the Nutritional Requirements for Food and Drink in Schools (Scotland)
Regulations 2008, Healthier Scotland, Scottish Government http://www.scotland.gov.uk/Resource/Doc/238187/0065394.pdf ; Health
Promotion and Nutrition in School, The Scottish Govt. http://www.scotland.gov.uk/Topics/Education/Schools/HLivi/foodnutrition ;
The Scotsman, Junk Food Law is Passed, March 15th 2003 http://www.scotsman.com/news/politics/top-stories/junk-food-law-ispassed-1-691025
Television Advertisement of Food and Drink Products to children, OFCOM, Independent Regulator and Competition Authority for the
UK Communications Industries http://stakeholders.ofcom.org.uk/consultations/foodads_new/statement/
Healthy Eating in Learning Centers http://www.parlamento.gub.uy/indexDB/textosaprobados/ListarTexto.asp?Id=1305 ; Advertising
Education Forum, Bill to ban ‘junk food’ advertising in schools adopted by Senate, April 11th 2011,
Uruguayhttp://www.aeforum.org/news/1365686024/Uruguay:Bill_to_ban_%E2%80%98junk_food%E2%80%99_advertising_in_sch
ools_adopted_by_Senate
54
36. http://www.food.gov.uk/multimedia/pdfs/techguidenutprofiling.pdf
37. https://www.health.gov.au/internet/main/publishing.nsf/Content/5FFB6A30ECEE9321CA257BF0001DAB17/$File/CanteenGuidelines.PDF
55