Sunderlin - Insulin therapy in ICU
advertisement

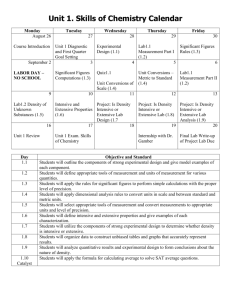
Elaine Sunderlin EBM Friday 1/22/2010 Intensive Insulin Therapy in Critically Ill Patients Greet Van den Berghe, MD, et.al NEJM, Vol 345, No. 19, November 8, 2001, 1359-1367 Background: Critically ill patients who require intensive care for > 5 days have a substantial risk of death and substantial morbidity. Hyperglycemia associated insulin resistance is common in critically ill patients, even those who do not have a previous diagnosis of diabetes Conflicting studies showing cardioprotective effects of tight glucose control following acute myocardial infarction Tight glucose control works to improve outcomes on a chronic basis, shouldn’t it do the same in the acute setting? Hypothesis: Hyperglycemia or relative insulin deficiency (or both) during critical illness may directly or indirectly confer a predisposition to complications such as severe infections, polyneuropathy, multiple-organ failure, and death. Type of Study: Prospective, randomized trial at one center comparing intensive insulin therapy vs conventional insulin therapy in patients admitted to the surgical ICU Blinded: no Patients were randomized and stratified according to the type of critical illness Methods: All adults receiving mechanical ventilation who were admitted to the SICU between 2/2/2000 and 1/18/2001 were eligible for enrollment. Only 14 patients were excluded; 5 were in other trials and 9 who were moribund or for who there were DNR orders. A total of 1548 were eventually enrolled, with 783 in the conventional treatment group and 765 in the intensive treatment group. Conventional treatment: a continuous infusion of insulin was started only if the blood glucose level exceeded 215mg/dl and the infusion was adjusted to maintain blood glucoses between 180-200 mg/dl Intensive treatment: continuous insulin infusion was started if the blood glucose level exceeded 110 mg/dl and was adjusted to maintain normoglycemia (80-110 mg/dl) Adjustments of insulin were based on whole-blood glucose in arterial blood measured in a glucose analyzer. Blood glucose was checked every 1-4 hours On admission, all patients were fed continuously w/ IV glucose (200300g/24hr). The next day, TPN, combined parenteral and enteral, or total enteral feeding was started. Primary outcome measure: Death from any cause in the ICU Secondary outcome measures: In-hospital death; the number of days in the ICU; the need for prolonged intensive care (>14 days) or readmission; the need for ventilatory support; renal replacement therapy; inotropic or vasopressor support; critical-illness polyneuropathy; markers of inflammation (CRP, WBC, body temp); bloodstream infection and use of antibiotics for >10 days; transfusion requirements; and hyperbilirubinemia Results: Conventional treatment group Intensive treatment group P value Death during intensive care 8.0% 4.6% <0.04 Death during 1st 5 days 1.8% 1.7% 0.9 Death in pts requiring >5 days of IC 20.2% 10.6% 0.005 Things to consider Rate of hypoglycemia (BG <40) significantly increased in the intensive treatment group (39 pts compared to 6 pts in the conventional group) Most of the patients were post-cardiac surgery 13% of patients enrolled had a reported history of diabetes. However, there were no recordings of HgbA1C’s so difficult to tell how many patients had previously undiagnosed DM There were no specific guidelines regarding feeding the patient. They did comment on standardization of the amount of calories in feedings. However, they never commented on if one group was on TPN longer than the other group. Did having the nurse spend more time in the intensive group patient’s room checking blood glucoses increase their quality of care compared to the conventional group? Interim analyses of overall mortality were performed at 3-month intervals. The 4th interim analysis indicated that conventional treatment was inferior and the study was subsequently stopped. Did stopping the study early amplify the results? For your review: Van den Berghe, et.al. “Intensive insulin therapy in the medical ICU”, NEJM 2006;354:449-61 Devos, P, et.al. “Impact of tight glucose control by intensive insulin therapy on ICU mortality and the rate of hypoglycemia; final results of the Glucontrol study”, Intensive Care Med 2007;33:Suppl 2:S189 Brunkhorst FM, et.al. “Intensive insulin therapy and pentastarch resuscitation in severe sepsis”, NEJM 2008;358:125-39 “Intensive versus Conventional Glucose Control in Critically Ill Patients; NICE-SUGAR Study Investigators”, NEJM 2009; 360;13:1283-1297